Consent and Capacity, Dr. Rebecca Verhaeghe
advertisement

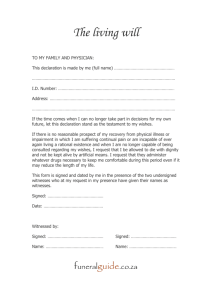
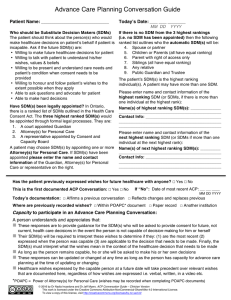
Practical Understanding and Applications NSPCN Huntsville Oct 21, 2014 Dr. Rebecca Verhaeghe Advance care planning Define: 1. 2. 3. 4. Advance Care Directives Capacity Consent Substitute Decision Maker/POAs/Family Deeper practical understanding of the purpose and meaning of capacity and consent Enhanced knowledge as to your role and responsibility in acquiring, communicating and implementing wishes, values and beliefs of your patient Ability to identify/evaluate your own values and biases and set boundaries consistent with patients needs Speaks to the “quality of understanding” regarding a specific treatment decision Can patient understand and appreciate the basics of what will happen if they accept or refuse a certain treatment or intervention Not a value judgement, not based on “right or wrong” treatment choices Does not involve coercion by healthcare providers Not carved in stone- can change mind, capacity can fluctuate Not based on a diagnosis or screening test Not a one time stop- ensure/assess understanding each and every time healthcare decision 1. 2. Capacity can fluctuate. “ A health care provider can rely upon previously documented evaluations and assessments , however the health care provider should review capacity as appropriate during interactions with patient. Two-part test: The patient can understand the information relevant to making a decision about the proposed treatment and Is able to appreciate the reasonably foreseeable consequence of their decision. Identify who can give consent—patient, SDM and if consent family members/other significant others Patients/families wishes should be elicited Context is crucial- take into account patients goals/values/beliefs. Someone who makes decisions on your behalf if you are incapable of making them yourself. Role of SDM: To make the same personal care choices that you would have made in that situation and follow your instructions if you gave any. acts only when you can’t make decisions yourself. May be temporary or indefinite You cannot choose: • Someone who is paid to provide you with personal care • Someone who is mentally incapable • Someone who is under the age of 16 The documentation of your SDM in event you become incapable of making a particular decision. The document appoints your SDM and gives them the power to make decisions about all aspects of your personal care. • Health care • Shelter, clothing, nutrition, hygiene • Personal safety 1) 2) 3) Inform/outline the nature of proposed treatment/intervention (CPR, other potentially Life-Sustaining Treatments Outline expected benefits (Right to receive) Likely to benefit Intervention has uncertain/unlikely benefit( lean towards treatment- suggest trial and suggestion to withdraw if benefit not seen Patient almost certainly will not benefit C H E M O / R A D S C P R D N R I N F E C T I O N H Y D R A T I O N F E E D I N G T U B E M E D I C A T I O N S T R A N S U F U S O N D I A L II S Y S I S S U R G E R Y C L O S U R E I N V E S T I G A T I O N Purpose- to assist patients in making choices and articulating their wishes about end of life care Nurses (CNO- guiding decisions about end of life care-2009) Core themes 1. Communication: communicate with patients and members of the inter-professional team to guide informed discussion about PATIENTS GOALS 2. Implementation: advocate for the PATIENTS WISHES and help implement the clients treatment and end of life care wishes Clarify patients expressed wishes regarding end of life care (previous advance directive, verbal/written expressions to POA/SDM Ongoing Review/update of patients “Plan of treatment” and communicate this to patient/family (with consent), interprofessional team) Document Prior to implementation -Ensure the plan of treatment involved the patient/family/inter-professional team and the patient has given informed consent Create a safe place for important conversations Tips- start open ended- make a connection- create a context…create a common ground. Give the patient a sense of control/self determination 1. Normalize---set expectations. Introduce yourself and your role “ “as part of your care team I, and other caregivers will be making the effort to involve you in the type of care and support you need. There are important questions that will be asked- the focus is not to frighten or bother you but to make sure that your wishes and needs remain the focus of our efforts.. Its best to have these discussions when you are feeling well enough” DO YOU HAVE ANY QUESTIONS? IS THERE ANYTHING THAT YOU HAVE THOUGHT OF- THINGS THAT YOUR WOULD WANT OR NOT WANT- (who have you shared this with, is there anything you want to share now (If not clear- clarify SDM in simple language (if you were too unwell at a given time to communicate your wishes, who would you choose to speak on your behalf) CONTENT/Information Gathering Medical ? “what is your understanding of your diagnosis ?”what do you think your prognosis is “how long do you think you have to live”- Have you asked or been told what to expect? Are you the type of person that would want to know? If not is thee anyone in your circle of family and/or friends that would want to/need to know” ? “who have you shared this with” “Is there anyone else you want to know, be updated about your conditions – is there anyone you don’t want information given to—ok to explore why ? “do you feel that you and your family/caregivers are on the same page Personal Normalize- its normal to experience feelings of anxiety when faced with uncertainty. Even if you are not usually an open person, we want you to know it important to share your emotions and reactions to what is happening to you. Anger, fear, regret, sadness– can all be a part of the process Tip-Provide the opportunity to express personal concerns— Open ended- Is there anything that you are worried about? As you reflect on your life?are there any unfinished business, wishes-important celebration/milestones you hope to meet/ Need relief from feeling they are a burden to others/or need to please or be strong for others (sign on door, boundary setting) Opportunity for closure- unfinished businessresolution “Are we good?” Managing conflicts with family members/interprofessional team Closure of difficult conversation- “ none of us have control over this disease process, or when your last breaths will be taken… but we can all work together to make this the most peaceful experience possible, and honor your life and relationships- embracing what is most important to you • • Closure of conversation Make sure opportunity given to communicate personal concerns -affirmation-”while you are physically unwellyou are still a whole person- worthy of respectful and compassionate care – every effort will be made to provide you with the dignity and privacy you require” Establish sense of preparedness, control, meaning (preserve autonomy/self determination) -MEANING- very individual- Outcome depends on patients “often dependant on interpretation” of events (respect cultural, religious personality factors)- is ok to reframe-as long as not pushing your own agenda “sometimes people who left the faith of their parents and childhood desire to come back to it when facing death…. That’s ok Requires Input from all involved in circle of care MD/NP ROLE- update re changes in the body, identify shift in direction- can be less involved as transition progresses Focus on what will make a difference to patient- physical, emotional, psychosocial, spiritual Do no harm- avoid over-sedation and uncontrolled pain Don’t avoid talking about the end Preparing- “are last rights important to you?” “is it important to have someone with you at the end?” everyone is different Have you communicated your thoughts about funeral/celebration of life ceremony Legal/financial arrangements “yesterdays history---tomorrows a mysterytoday is a gift- and that is why it is called the present” today- the focus needs to be on easing your suffering- provide opportunities for meaningful interaction. Our role is not to hasten death- or to prolong suffering…. FIND THE BALANCE Be hopeful—but realistic Letting go—songs, poems, permission giving A discussion between 2 or more people where: Stakes are high Opinions vary ( disagreement/opposing opinions anticipated) Strong emotions 1. 2. 3. 4. Advocate for the patients needs Validate the family members fears and concerns Educate about your role and responsibilities as a care provider Don’t get into a power-struggle Find common ground- “If your mother could speak, what would she hope you would do” Avoid conflict by having discussions early Address conflicts with team privately- work towards consensus of team members Correct misinformation/misunderstanding and answer questions If conflict continues – offer a referral to another professional /facilitate second opinion Consult- Ethics, offer resources to patient HEALTH CARE CONSENT ACT OFFICE OF PUBLIC GUARDIAN AND TRUSTEE, MAKING SUBSTITUTE HEALTH CARE DECISIONS MINISTRY OF ATTORNEY GENERALCAPACITY ASSESSMENT OFFICE Advocacy for the elderly- includes legal CCAC- capacity evaluation related to LTC Know your strengths and weaknesses (our greatest strength can become a weakness when under stress) Know and be able to identify your biases. This will protect you from projecting your values on to others. Establish good boundaries. Don’t feel pressured to answer questions or provide information outside of your scope of practice. Ask for help. If you make a mistake, exercise poor judgment, don’t keep it to yourself. Take care of yourself---so you can care for others in a professional and compassionate manner. Understand how your own experiences/values/worldview impact your approach to end of life and treatment discussions Develop internal filter/boundary setting that respects the individuals right to self determination Engage – in developing your skills/comfort Passion + Knowledge + Skills = Impact ENGAGE- catch the opportunity to communicate Consult-share your experiences with your teammates Access to best practice guidelines E-learning- modules Passion + Knowledge + Skills = Empowered Attitude, self reflection and Insight = Connection Supportive System-Shared focus-Common Goals= Culture of constructive care CPSO-decision-making for End of Life policy # 1-06 2006 Quality End of Life Care Coalition of Canada Blueprint for action 2010-2020 WHO- Palliative care for older people : better practices, 2011 Canadian Hospice Palliative Care Association Cd/training guide on educating future Physicians in Palliative and end of life care 2014 CNO Guiding Decisions About End-of –Life Care 2009 Speak Up- start the conversation about end of life care; www.advancecareplanning.ca Polypharmacy- Improved renal and cognitive function in a hospice patient www.annalsof longtermcare.com vol 22 issue 10 October 2014 CAPC- Center to advance palliative care- What Patients Want www.capc.org E-Learning modules- South West Hospice Palliative Care Network- Advance Care Planning info@swpalliativecare.ca Social Work- code of ethics and standard of practice Crucial Conversations Tools for Talking when the stakes are high. 2012 (Patterson, Grenny , McMillian Switzler )