von Willebrands Disease
advertisement
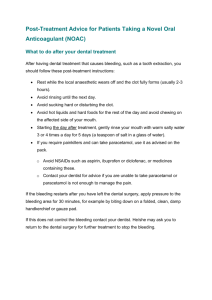
Managing Dental Patients with Medical Problems Dayton W. Daberkow II MD Leonard J. Chabert Internal Medicine Residency Program Director Houma, Louisiana Diabetes 45 year old male with history of diabetes type 2 on Glargine (Lantus) 30 units at bedtime and has a dental procedure in the morning. 20 minutes after the procedure the patient tells the nurse he fells very weak, his right arm is weak and his fingers are tingling. What do you recommend at this time? 1. 2. 3. 4. Contact EMS to transfer to emergency room for a stroke work-up. Make sure the patient is laying down and check on him in 30 minutes. Check the blood glucose with a glucometer. Give a rapidly absorbed form of 15 grams of a carbohydrate. Diabetes If the patient is unable to take anything by mouth, has an IV line and his glucose is 30 you should: 1. 2. 3. 4. Recheck the glucose in 20 minutes to make sure it is low before initiating any treatment. Administer 1 amp of D50 solution (25 to 50 mL of a 50% dextrose solution). Administer 1 amp of bicarbonate Administer 5 mg of Glucagon Diabetes If the patient does not have an IV then do the following if hypoglycemic: 1. 2. 3. 4. Administer 1 mg of glucagon IM or SQ at any body site. Administer 1 mg of epinephrine IM or SQ Administer 1 amp of D50 under the tongue Administer 1 mg of glucagon under the tongue Management of hypoglycemia in the office • Signs and symptoms: confusion, tremors, sweating, agitation, anxiety, dizziness, tingling or numbness, and tachycardia. Severe hypoglycemia may result in seizures or loss of consciousness. • Immediately check blood sugar with a glucometer. • If no glucometer available assume HYPOGLYCEMIA with above symptoms. Hyperglycemia can have some of these same symptoms but hypoglycemia more dangerous. Type 2 diabetes treated with oral hypoglycemic agents 55 y/o female with history of diabetes type 2 will have a dental procedure in the morning. She takes metformin twice a day. She will be not eating breakfast before the procedure. You advise her to do the following: 1. Take the morning dose of her metformin. 2. Hold morning dose of metformin, resume evening dose if eating. 3. Hold morning dose of metformin and double the dose at bedtime. 4. Hold both morning and evening dose of metformin. Type 2 diabetes treated with oral hypoglycemic agents • Sulfonylureas increase the risk of hypoglycemia • DPP-IV inhibitors (gliptins) and GLP-1 analogs (incretins) could alter GI motility • Metformin is contraindicated in conditions that increase the risk of renal hypoperfusion, lactate accumulation and tissue hypoxia • Therefore, hold all oral hypoglycemic agents before procedures that require morning fasting. If no fasting, patient may take oral hypoglycemics with careful glucose monitoring. Type 1 or insulin treated type 2 diabetes 35 male with history of diabetes type 2 is scheduled for a dental procedure the next day. He takes 25 units of Glargine (long acting insulin) nightly and 6 units of Novolog (rapid acting) with each meal. He will be NPO before the procedure. You recommend: 1. Hold Glargine and Novolog and resume the evening after the procedure. 2. Hold Glargine but begin and insulin infusion in the office. 3. Continue Glargine the night before procedure and give ½ dose of Novolog in the morning. 4. Continue Glargine the night before procedure and hold Novolog until patient eating. Type 1 or insulin treated type 2 diabetes For minor morning procedures: • Generally patients who use insulin can continue with their subcutaneous insulin for procedures that are not long and complex. • If the patient has borderline hypoglycemia or "tight" control of the fasting blood glucose, reduce the night time (supper or HS) long or intermediate acting insulin on the night prior to surgery to prevent hypoglycemia. • Type 1 diabetes can develop ketoacidosis if they take no insulin even they are NPO. Their basal metabolic needs when fasting require at least ½ their usual insulin requirements. • Hold short-acting insulin until eating. Type 1 or insulin treated type 2 diabetes For Procedures that are long or take place later in day where both breakfast and lunch are missed: •If insulin (both intermediate and short-acting insulin) taken only in morning, give one-half their total morning insulin to provide basal insulin during the procedure and prevent ketosis •Hold short-acting insulin morning of procedure if also on long acting insulin. •For patients who take insulin two or more times per day, give between onethird to one-half of the total morning dose (both intermediate and shortacting insulin) as intermediate acting insulin only •Patients on continuous insulin infusion may continue with their usual basal infusion rate. Start dextrose containing intravenous solution. Biphosphonates and Dental Surgery Osteonecrosis of Jaw (ONJ) • Risk factors include invasive dental procedures (eg, tooth extraction, dental implants, boney surgery); a diagnosis of cancer, with concomitant chemotherapy or corticosteroids; poor oral hygiene, ill-fitting dentures; and comorbid disorders (anemia, coagulopathy, infection, pre-existing dental disease). • Most cases after IV but some reports of oral therapy. • Manufacturer recommends discontinuing bisphosphonates in patients requiring invasive dental procedures. No real evidence this prevents ONJ. Blood Pressure Management 60 year-old-male with a history of hypertension is scheduled for a dental procedure. His past history and physical examination are unremarkable. He takes Verapamil 240 mg every day and his blood pressure in the office was 130/80. Which of the following is the best strategy for preoperative evaluation 1. Schedule an exercise stress test 2. Echocardiogram 3. Hold blood pressure pill before surgery 4. Take blood pressure pill AM of surgery Blood Pressure Management 55 year-old-female with a history of hypertension is scheduled for a dental procedure. Past history and PE are unremarkable. She takes HCTZ 25 mg every AM and office blood pressure is 200/120. Which of the following would be the best management? 1. Take HCTZ am of surgery and proceed to surgery. 2. Delay surgery and add another BP pill to get diastolic blood pressure less than 110 mm Hg. 3. Delay surgery and increase dose of HCTZ to get diastolic blood pressure less than 80. Blood Pressure Management • Elective surgery/procedures should be postponed in patients with blood pressures above 170/110 mmHg • Take all blood pressure pills with sip of water morning of procedure • Continue antihypertensive treatment throughout procedures, especially drugs like Clonidine and Beta- blockers to avoid severe post procedure hypertension. Hypertensive Emergencies • Repeat BP in both arms and again 10 minutes later and make sure the cuff size is the appropriate size (bag length 80% of limb circumference) • For severe hypertension systolic BP > 200 or diastolic BP > 120 assess whether the elevated BP is causing target organ damage • Assess neurologic, cardiac, renal function and retinas • Patients with evidence of target organ damage should be admitted to an ICU with invasive monitoring and parenteral antihypertensive therapy • Don’t lower BP aggressively if there are focal neurological signs; don’t allow diastolic BP to fall below 100 mm Hg Endocarditis Prophylaxis 26 year-old-male with a history of mitral valve prolapse with regurgitation 1. Amoxicillin 2.0 grams orally 1 hour before surgery (1997 AHA guidelines) 2. No prophylaxis needed (2007 AHA guidelines) 3. Amoxicillin 1.0 gram orally 1 hour before surgery 4. Amoxicillin 1.0 gram orally 1 hour before and 1.0 gram after surgery Endocarditis Prophylaxis 65 year-old-male with a history of a prosthetic mitral valve who’s jaw is broken and can’t swallow. 1. No prophylaxis needed 2. Amoxicillin 2.0 grams orally 1 hour before surgery 3. Ampicillin 2.0 grams IM/IV 30 minutes before surgery 4. Ampicillin 2.0 grams IM/IV 3 hours before and 1 hour after surgery Endocarditis Prophylaxis 44 year-old-female with a previous history of endocarditis who is allergic to penicillin 1. No prophylaxis needed 2. Cephalexin 500 mg 1 hour before surgery 3. Clindamycin 600 mg orally 1 hour before surgery 4. Azithromycin or Clarithromycin 500 mg orally 1 hour before surgery 5. 2 or 3 6. 3 or 4 Endocarditis Prophylaxis 50 year-old-female with a history of hypertrophic cardiomyopathy who is allergic to penicillin and can’t swallow 1. No prophylaxis needed (2007 AHA guidelines) 2. Vancomycin 1.0 gram IV 1-2 hours, complete infusion before surgery 3. Cephalexin 1.0 gram IV 30 minutes before surgery 4. Clindamycin 600 mg IV 30 minutes before surgery (1997 AHA guidelines) Cardiac Conditions Associated With Endocarditis Endocarditis Prophylaxis Recommended for High-risk categories: 1. Prosthetic cardiac valves, including bioprosthetic and homograft valves 2. Previous bacterial endocarditis 3. Complex cyanotic congenital heart disease (e.g.. Single ventricle states, transposition of the great arteries, tetralogy of Fallot) 4. Surgically constructed systemic pulmonary shunts or conduits 5. Cardiac Transplant with new valvulopathy Cardiac Conditions Associated With Endocarditis No Prophylaxis Recommended (2007 AHA Guidelines) Moderate risk category: Most other congenital cardiac malformations (other than high-risk) • Acquired valvular dysfunction (e.g.. Rheumatic heart disease AI, AS, MS, MI) • Hypertrophic cardiomyopathy • Mitral valve prolapse with valvular regurgitation and/or thickened leaflets • Cardiac Stents first 30 days? Endothelialized Endocarditis Prophylaxis Not Recommended Negligible-risk category (no greater risk than the general population) • Isolated secundum atrial septal defect • Surgical repair of atrial septal defect, ventricular septal defect, or patent ductus arteriosus (without residua beyond 6 months) • Previous coronary artery bypass graft surgery • Mitral valve prolapse without valvular regurgitation • Physiologic, functional, or innocent heart murmurs • Previous rheumatic fever without valvular dysfunction • Cardiac pacemakers (intravascular and epicardial) and implanted defibrillators Dental Procedures and Endocarditis Prophylaxis Endocarditis Prophylaxis Recommended: •Dental extractions •Periodontal procedures including surgery, scaling and root planing, probing, and recall maintenance •Dental implant placement and reimplantation of avulsed teeth •Endodontic (root canal) instrumentation or surgery only beyond the apex •Subgingival placement of antibiotic fibers or strips •Initial placement of orthodontic bands but not brackets •Intraligamentary local anesthetic injections •Prophylactic cleaning of teeth or implants where bleeding is anticipated Prophylaxis recommended • All dental procedures that involve manipulation of gingival tissue or the periapical region of teeth or perforation of the oral mucosa. • For patients only in the HIGH RISK category Prophylactic Regimens for Dental, Oral, Procedures Situation Standard general prophylaxis Agent Amoxicillin Regimen Adults 2.0g; children 50 mg/kg orally 1 hr before procedure Unable to take oral meds Ampicillin Adults 2.0g intramuscular (IM) or intravenously (IV); children: 50 mg/kg IM or IV within 30 min before procedure Prophylactic Regimens for Dental, Oral, Procedures Situation Allergic to penicillin Agent Clindamycin Regimen Adults 600 mg; children: 20 mg/kg orally 1 hr before procedure Azithromycin, Clarithromycin Adults 500 mg; children 15 mg/kg orally 1 hr before procedure Prophylactic Regimens for Dental, Oral, Procedures Situation Allergic to penicillin and unable to take before procedure Agent Clindamycin Regimen Adults: 600 mg IM/IV; children 20 mg/kg IM IV within 30 minutes Endocarditis Prophylaxis For patients having surgery, which of the following cases requires Endocarditis prophylaxis: (yes/no) 1. 26F with a hx of MVP w/o regurgitation 2. 40F with a physiologic/innocent heart murmur 3. 60M with a hx Endocarditis 4. 55M who has a systolic murmur that increases with valsalva and echocardiogram shows a thickened septum 5. 70F with a prosthetic aortic valve 6. 70F with a hx of CABG 2 months ago 7. 66M who had a cardiac pacemaker for SSS 8. 66M s/p repair of an atrial septal defect Prosthetic Joints • Prosthetic joints in > 2 years and no immunocompromising states no antibiotic prophylaxis. • Prosthetic joints in < 2 years and immunocompromised maybe antibiotic prophylaxis. Cardiac Conditions and Dental Procedures 62-year-old man with history of CABG 3 years ago is scheduled for a dental procedure. No other medical problems and physical examination is unremarkable. What historical information will best help you in managing this patient? 1. No headaches or dizziness 2. No shortness of breath (SOB) while sleeping 3. No chest pain or SOB at rest 4. No chest pain or SOB after walking up a flight of stairs Cardiac Conditions and Dental Procedures This same 62 year-old-man with a history of a CABG had chest pain over the past month that occurred with ambulation after one block and has been increasing in severity, duration, and frequency over the past 1 week. What is the best preoperative strategy? 1. Take nitroglycerin before dental procedure 2. Echocardiography 3. Proceed to dental procedure with no action 4. Cancel dental procedure and refer back to PCP or cardiologist Cardiac Conditions and Dental Procedures A 38 male is scheduled for a dental procedure. His physical examination revealed a jugular venous pressure of 8 cm, an S3 gallop, and bilateral crackles? He also says that he has had progressive SOB over that past 3 weeks? 1. Proceed to dental procedure 2. Coronary angiogram to decrease risk 3. Delay surgery and medically manage until the CHF has resolved Cardiac Conditions and Dental Procedures 55 year old female is scheduled for a dental procedure. She has a history of atrial fibrillation on no anticoagulation. She has had palpitations over past 2 weeks, is on metoprolol 25 mg twice a day and office heart rate is 120. You recommend: 1. Cancel procedure and refer to PCP for management of her atrial fibrillation and better heart rate control < 110 2. Proceed with procedure as long as heart rate < 130 3. Administer digoxin 0.25 mg in the office and have the patient stay until heart rate < 90 Active Cardiac Conditions for which patients should undergo evaluation and treatment before Non-cardiac Surgery 1. Unstable Coronary Syndromes Unstable or severe angina (CCS Class III or IV). Recent MI (more than 7 d less than 1 month). 2. Decompensated HF NYHA functional class IV; worsening or new-onset HF. Congestive Heart Failure Systolic Dysfunction Pharmacological Management • Diuretic - Furosemide 20-80 mg per day (200 mg in CRI). Best to give at 4-6 PM when volume status highest. • Spironolactone 25-100 mg BID • Angiotensin Converting Enzyme (ACE) inhibitor at bedtime (captopril, enalapril). Titrate to the largest tolerated dose. • Beta-Blockers with meals. • Discontinue ACE inhibitors if the serum potassium is >5.5 meq per L that cannot be reduced, sx hypotension, or hx of adverse reaction • Hydralazine/isosorbide dinitrate is an alternative for ACE inhibitors or ARB’s (Angiotensin II receptor blockers i.e. losartan) • Digoxin • Monitor electrolytes, control blood pressure • Avoid NSAIDS and COX-2 inhibitors Active Cardiac Conditions for which patients should undergo evaluation and treatment before Non-cardiac Surgery 3. Significant Arrhythmias – – – – – – – High grade AV block Mobitz Type II AV block 3rd degree AV block Symptomatic ventricular arrhythmias Supraventricular arrhythmias (atrial fibrillation with uncontrolled rate, HR greater 110 at rest) Symptomatic bradycardia Newly recognized ventricular tachycardia Active Cardiac Conditions for which patients should undergo evaluation and treatment before Non-cardiac Surgery 4. Severe Valvular Disease: Aortic Stenosis severe (mean pressure gradient > 40 mm Hg, aortic valve area < 1.0 cm2, or symptomatic) Mitral Stenosis Symptomatic (progressive dyspnea on exertion, exertional presyncope, or HF) Cardiac Risk for Non-cardiac Surgical Procedures Low (<1% cardiac risk)* Dental procedures Breast surgeries Endoscopic procedures Superficial procedures Cataract operation Ambulatory surgery *combined incidence of cardiac death and nonfatal MI. Noncardiac Surgery and medicines Perioperative Statin therapy: Protective effect on cardiac complications, therefore, continue through surgery/procedure. Alpha-2 Agonists: Clonidine has minimal hemodynamic effects and reduced postoperative mortality for up to 2 years. Continue through surgery/procedure Perioperative Calcium Channel Blockers: Reduced ischemia and supraventricular tachycardia and death and MI. Continue through surgery/procedure. Lung Disease and Dental Procedures A 25 year old male with history of asthma is scheduled for a dental procedure. What questions are important to ask him to assess the status of his asthma? 1. 2. 3. 4. 5. 6. What medicines are you currently taking? Do you have any pets in the house? Have you had any of the following, cough, wheezing, shortness of breath, chest pain over the past 2 weeks? Did you get your flu shot this year? 1,2 and 4 1 and 3 Lung Disease and Dental Procedures A 32 year old female with a history of Asthma is scheduled for a dental procedure. She takes fluticasone/salmeterol (100/50) 1 puff twice a day and an albuterol inhaler 2 puffs as needed daily. She has had to use her albuterol 4 times a day over the last week because of a lingering cough. You recommend: 1. Advise to stop the albuterol since it is making her cough worse. 2. Proceed with dental procedure since it will be less than 1 hour and no drugs will be used to affect her asthma 3. Send to ER immediately 4. Cancel procedure and refer to PCP to assess asthma Lung Disease and Dental Procedures Two weeks later this same 32 female is scheduled for her dental procedure. Her PCP increased her fluticasone/salmeterol to (200/50). She wants to get the procedure done and said the cough is better but does get short of breath twice a day and has had some chest pain. What test below would provide the most information about the current state of her asthma? 1. Pulmonary function studies. 2. Chest X-ray 3. Peak flow meter reading in the office 4. Arterial blood gas Lung Disease and Dental Procedures Severe Persistent Asthma • • • • Symptoms throughout the day Nocturnal symptoms frequent Nocturnal awakenings nightly Need for short-acting beta agonists for symptom relief several times per day • Peak flow rate: < 60% predicted Lung Disease and Dental Procedures Severe Persistent Asthma Treatment: • Medium to High-dose Inhaled Corticosteroids (ICS) and Long-acting Beta-2 agonist (LABA) • Omalizumab an anti-IgE therapy may be considered if there is objective evidence of allergies i.e. allergy skin tests • Oral corticosteroids as needed for severe symptoms Lung Disease and Dental Procedures Potential Risk Factors Asthma Maximize control before any procedure/surgery • No cough, SOB, wheezing • Peak flow greater than 80% predicted or personal best value • Pulmonary Exam should be free of wheezes Lung Disease and Dental Procedures 65 y/o M with history of COPD is scheduled for a dental procedure. He takes ipratropium bromide inhaler 2 puffs twice a day and a short-acting Beta-agonist 2 puffs twice a day. He has a non-productive cough that has been increasing the past 2 weeks. Lung exam reveals bilateral wheezes. Management before procedure: a. Increase both inpratropium bromide and the shortacting beta-agonist b. Begin antibiotics c. Get pulmonary function tests prior to surgery d. Perform procedure Lung Disease and Dental Procedures After 2 weeks of maximizing his inhalers by his PCP he still has a non-productive cough and SOB that is worse than 4 weeks ago. On lung exam he has bilateral wheezes that haven’t changed. The chest x-ray shows no infiltrate/pneumonia. Management: a. Proceed to procedure/surgery b. Begin Antibiotics c. Steroids-Prednisone 40 mg in AM for 7-10 days Lung Disease and Dental Procedures 55 y/o M with a history of COPD is scheduled for a dental procedure. He takes ipratropium bromide 2 puffs twice a day. Over the past 10 days he has had increasing SOB and a cough with productive sputum. On exam he has bilateral decreased breath sounds. What do you recommend? a. Cancel procedure and follow-up with PCP and get pulmonary function tests b. Send to ER and get a stat EKG c. Cancel procedure follow-up with PCP and get a Chest x-ray d. Proceed to procedure Lung Disease and Dental Procedures The chest x-ray showed no infiltrates/pneumonia. What do you think his PCP would be adding for further management before the dental procedure? a. Add short-acting beta-2 agonist b. Prednisone 40 mg for 7 days c. Continue ipratropium bromide inhaler d. Antibiotics e. All of the above Lung Disease and Dental Procedures COPD • Patients with COPD have an increased risk of postop/procedure pulmonary complications depending on severity • Treat patients who do not have optimal reduction of symptoms (cough, SOB) and optimal exercise capacity before surgery • Combinations of bronchodilators, physical therapy, smoking cessation, antibiotics for exacerbations, and corticosteroids will reduce the risk. Lung Disease and Dental Procedures COPD • Antibiotics only for COPD exacerbations as defined by change in character or amount of sputum production. • Patients with continued symptoms despite bronchodilator therapy may benefit from a 1-2 week preoperative/preprocedure course of steroids. Lung Disease and Dental Procedures Preventing Pulmonary Complications Pre-procedure: 1. Urge patient to stop smoking 2. Treat uncontrolled COPD or asthma before surgery 3. Delay procedure and administer antibiotics if a respiratory infection is present Lung Disease and Dental Procedures Pre-procedure Evaluation The history and physical examination are the most important parts of the pre-procedure pulmonary assessment History 1. Cough 2. Dyspnea 3. Wheezing 4. Exercise Tolerance Lung Disease and Dental Procedures History: 5. Smoking history 6. Medications 7. History of pneumonias 8. DVT/PE with prior surgeries 9. Known pulmonary disease COPD Asthma Restrictive disease Sleep Apnea Hepatic Disease and Dental Procedures Acute and chronic liver disease can significantly change the patient’s ability to tolerate surgery and anesthesia. Therefore, it is important to determine preoperatively if hepatic functions have been disturbed. If so, the severity of the functional impairment should be assessed and steps undertaken to minimize the operative/procedure risk. The functional disturbances that can occur as the result of liver disease include: Hepatic Disease and Dental Procedures 1. Bleeding Problems • Deficiency in the coagulation factors synthesized in the liver (II, VII, IX, X) and fibrinogen. • Thrombocytopenia secondary to an enlarged spleen or alcoholic depression of the bone marrow. • Portal hypertension causing esophageal varices which can bleed. 2. Fluid and electrolyte disturbances • Sodium retention, hypokalemia, hypocalcemia and hypoalbuminemia. • Edema, ascites and hepatorenal syndrome. Hepatic Disease and Dental Procedures 3. Malnutrition • Present in patients with significant liver disease due to anorexia, poor intake and hypermetabolic state. 4. Immunocompromised • Host defenses that rely on immunoproteins synthesized by the liver are impaired. • Increased risk of infection in patients with severe liver disease. 5. Central nervous system dysfunction • Hepatic encephalopathy. Events that occur perioperatively can exacerbate hepatic encephalopathy which can include blood in the GI tract. Hepatic Disease and Dental Procedures History of Liver disease should be suspected if the patient gives a history of significant or chronic alcohol intake, illicit drug use, tattoos, exposure to toxic materials, prior blood transfusions, sexual promiscuity, family history of liver disease or hepatitis, or jaundice. Hepatic Disease and Dental Procedures • Physical Examination. A patient may have no physical signs of liver disease. If active hepatitis exists, the liver may be enlarged and tender. Cirrhotic disease produces a small, hard, nontender liver. • Other findings may include increased abdominal girth, jaundice, palmar erythema, spider telangiectases, splenomegaly, and gynecomastia or testicular atrophy in men. Hepatic Disease and Dental Procedures Laboratory Examination if liver disease is suspected by history or by physical examination, blood chemistries should be obtained. A history of viral hepatitis or IV drug abuse is a definite indication for serology testing. Hepatic Disease and Dental Procedures • 40 y/o F is scheduled for surgery. History of a blood transfusion in 1988. Past medical history is unremarkable, her PE is normal and she has no symptoms. The dentist orders a comprehensive metabolic profile. The serum albumin, ALP, and PT are all within normal limits but the AST and ALT are elevated respectively at 150 normal (550) and 200 normal (5-55). No recent travel. • Hepatic Disease and Dental Procedures What other blood tests would you order? a. None proceed to procedure b. TSH, CBC and HBs Ag c. HBs Ag, Anti-HCV d. CBC and INR g. HBs Ag, IgM anti-BHc, Anti-HCV, IgM anti HAV Hepatic Disease and Dental Procedures Blood chemistry tests for liver disease • Serum glutamic oxaloacetic transaminase, (SGOT), (AST) • Serum glutamic pyruvic transaminase (SGPT), (ALT) • Gamma glutamyltranspeptidase (GGPT) • Total bilirubin • Alkaline phosphatase • Total serum protein • Serum albumin • Prothrombin time/INR Hepatic Disease and Dental Procedures Initial Hepatitis Serology: • HBsAg • IgM anti-BHc • anti-HCV • IgM anti-HAV (travel history, seafood) Hepatic Disease and Dental Procedures The 40 y/o F comes back to your office 1 week later and you inform her that the Hepatitis C antibody is positive. May she proceed to with her dental procedure? Hepatic Disease and Dental Procedures An asymptomatic patient with mild elevations of serum aminotransaminases (AST, ALT) that have stabilized and have a normal total bilirubin, PT time, and albumin should tolerate surgery. Patient must follow up with a liver specialist and avoid alcohol, and hepatotoxic drugs like acetaminophen, NSAIDS, benzodiazepines, and raw seafood. Hepatic Disease and Dental Procedures Testing for Hepatitis C • IV drug users • People who received a blood transfusion before July 1992 • Long-term hemodialysis patients • Health care workers who have had percutaneous exposure to HCV-positive blood • Those with abnormal liver enzyme tests • Baby Boomers 1946-1964 (CDC 2012) Hepatic Disease and Dental Procedures Others to consider testing for Hepatitis C: • People who have received transplanted organs • People who sniff illegal drugs • Individuals who have undergone tattooing or body piercing • Those who have a sexual partner with Hepatitis C or people with multiple sexual partners or have had numerous STD’s Hepatic Disease and Dental Procedures 55 y/o M with a history of alcohol abuse is scheduled for a dental procedure. No symptoms and his PE is normal. AST 400 (5-50), ALT 100 (5-55), total bilirubin 1.8 (.2 - 1.3), PT 14 (control 15), albumin 4.0 (3.5 - 5.0) Best management before surgery? a. Fresh frozen plasma and proceed to surgery b. Proceed directly to surgery c. Abstain from alcohol 4-6 weeks prior to surgery Hepatic Disease and Dental Procedures Alcoholic Liver Disease: Alcohol leads to a state of relative deoxygenation around the central veins of the liver, which may affect the metabolism of drugs. Therefore, a period of abstinence is advised because of the high surgical risk seen in active alcoholic hepatitis. Acetaminophen must be used with caution because of the toxic metabolites that can result in hepatic necrosis. Diazepam, barbiturates should also be used cautiously. Hepatic Disease and Dental Procedures Laboratory Examination 1. Liver Enzymes: If liver chemistries are elevated they should be repeated in 48 hours to determine whether they reflect hepatitis that is worsening or resolving. Dental procedures should be deferred until the enzymes have normalized or stabilized. 2. Total bilirubin > or = 4 mg/dl carries a high procedure risk. 3. Tests of Liver Synthetic Function: Patients with a serum albumin = or < 3.5 gm/dl, and a PT prolonged three seconds over control and resistant to Vitamin K administration have a high procedure risk. Hepatic Disease and Dental Procedures • A 42 y/o male with history of cirrhosis secondary to Hepatitis C is scheduled for a dental procedure. He is alert, oriented with no bleeding problems or other symptoms. On PE he has no ascites or other physical signs of liver disease. What laboratory values will help you in evaluating his surgical risk? • a. CBC • b. Serum Albumin • c. Potassium • d. Total Bilirubin, PT • e. a and b • f. b and d Hepatic Disease and Dental Procedures Table 1. Modified Child-Pugh Score Albumin (g/dL) Bilirubin (mg/dL) Prothrombin Time (Seconds prolonged) or International Normalized Ratio (INR) Ascites Encephalopathy *Class A = 5-6 points *Class B = 7-9 points *Class C = 10-15 points 1 > 3.5 <2 <4 Points* 2 2.8-3.5 2-3 4-6 3 < 2.8 >3 >6 < 1.7 1.7-2.3 > 2.3 Absent None Slight-moderate Tense Grade I-II Grade III-IV Hepatic Disease and Dental Procedures Patients with stable cirrhosis without signs of liver failure, encephalopathy, poor nutritional status, uncontrolled ascites, albumin < 3.5, and bilirubin > 3.0 can usually tolerate surgery. There are no prospective studies to show better surgical outcomes after preop interventions to improve liver function but accepted guidelines are that: Elective surgery is: (Dental Procedures as a guide) • Tolerated in Child’s class A cirrhosis • Permissible in Child’s class B cirrhosis (with preop preparation, not hepatic resection or cardiac surgery) • Contraindicated in Child’s class C cirrhosis Hepatic Disease and Dental Procedures MELD Score • For over 30 years, the principal predictor of operative risk in patients with cirrhosis has been the Child's classification, but newer studies suggest that the Model for End-Stage Liver Disease (MELD) score may be superior. • MELD is a prospectively developed and validated chronic liver disease severity scoring system that uses a patient's laboratory values for serum bilirubin, serum creatinine, and the international normalized ratio for prothrombin time (INR) to predict survival. Hepatic Disease and Dental Procedures In patients with chronic liver disease, an increasing MELD score is associated with increasing severity of hepatic dysfunction and risk of death. MELD > 15 high surgical risk MELD 10-15 moderate surgical risk MELD < 10 lowest surgical risk Hepatic Disease and Dental Procedures The 42 y/o male with a history of cirrhosis has an albumin 2.7, total bilirubin 1.6 (.1-1.2) and normal AST and ALT but his prothrombin time is 18 (control 10-12) or 6 seconds prolonged. He is not anemic by his CBC. Initial management prior to surgery: a. Proceed to surgery b. Type and cross 4 units and of packed red blood cells and transfuse c. Fresh frozen plasma 8 units d. Vitamin K 10 mg SQ e. Vitamin K 10 mg po Hepatic Disease and Dental Procedures His platelet count is 60,000/mm3 (140-450,000) and his PT doesn’t correct at all after 10 mg of vitamin K. How would you correct his coagulopathy to decrease his risk of bleeding? a. Transfuse 6 units of platelets b. FFP c. Cryoprecipitate 10 units IV d. DDAVP e. Plasma exchange Hepatic Disease and Dental Procedures Correction of Coagulation Deficiencies PLATELETS -Prophylactic platelet transfusions for counts < 50,000/mm3 for minor surgeries (liver biopsies). Major surgeries < 100,000. -Alcohol may directly suppress platelet production in alcohol-related liver disease Hepatic Disease and Dental Procedures Hypoprothombinemia (elevated PT) Poor nutrition or malabsorption due to cholestasis may cause Vitamin K deficiency. -Vitamin K 10 mg 1-3 doses PO/SQ Impaired hepatic synthetic function -FFP -Cryoprecipitate 10 U IV -DDAVP IV -Plasma Exchange * Aim for a PT within 3 seconds of control Hepatic Disease and Dental Procedures 36 year-old-female is scheduled for a dental procedure. Four weeks ago she had a viral illness in which her eyes turned yellow and resolved after 1 week. She has no problems except for joint aches in her hands, her physical exam is unremarkable. What blood tests would you order? a. AST, ALT, total bilirubin, PT b. AST, ALT, CBC, thyroid test c. HbsAg, IgM anti-BHc d. Anti-HCV, IgM anti HAV e. a, b, c f. b, c, d g. a, c, d Hepatic Disease and Dental Procedures The 36-year-old female’s blood tests come back positive for HBsAg and IgM anti-BHc and her AST is elevated at 450 and her ALT is elevated at 658. All other tests including PT and bilirubin were within normal limits. What would be your next management: a. Delay procedure until 1 month after liver enzymes have returned to normal b. Proceed to surgery and type and cross for 4 units of FFP. c. Proceed to surgery since patient only has joint pain. d. Perform a liver biopsy prior to surgery Hepatic Disease and Dental Procedures Acute hepatitis: The presence of acute viral or alcoholic hepatitis increases operative risk 10 % and postop complications 11 %. Elective surgery/procedure should be delayed until one month after liver enzymes have returned to normal. Hepatic Disease and Dental Procedures Complications in Patients with Chronic Liver Disease after procedure: Watch for: • Hepatic Encephalopathy: Precipitating factors/post-op complications include: GI bleeding, constipation, azotemia, hypokalemic alkalosis, sepsis, hypoxia and use of CNS depressant drugs. • Treat with restriction of protein 30 grams per day, enemas or cathartics to cleanse the bowel, lactulose (an oral unabsorbable disaccharide) in a dose needed to achieve mild diarrhea. • Careful selection of medications used and adjustment of dosage, if necessary. • Bleeding. • Prothrombin time and Bilirubin are probably the best measures of hepatic function. • Bilirubin can be expected to rise after: complicated surgery, multiple transfusions, bleeding, or with systemic infections. Hepatic Disease and Dental Procedures Summary of Key Points: An asymptomatic patient with mild elevations of serum aminotransferase levels should have a work-up to look for the causes of liver disease before elective surgery. This may include a liver biopsy. Hepatic Disease and Dental Procedures Procedures/Surgery is well tolerated in: • Chronic persistent hepatitis (asymptomatic mild chronic hepatitis) • Mild, chronic active hepatitis (if the patient is well compensated, has normal PT time, bilirubin, and albumin) • Child's class A or MELD <10 cirrhosis Hepatic Disease and Dental Procedures Procedures/Surgery Permissable in: Child's class B or MELD 10-15 cirrhosis (except those undergoing extensive hepatic resection or cardiac surgery) who have undergone thorough preoperative preparation. Hepatic Disease and Dental Procedures HIGH RISK PROCEDURE/SURGERY IN LIVER PATIENTS WITH THE FOLLOWING: • Severe chronic active hepatitis - elective surgery contraindicated in symptomatic disease. • Active alcoholic hepatitis - 6-12 weeks abstinence advised (steroids ?). • Obstructive jaundice - increased risk of renal failure, DIC, stress ulceration, impaired wound healing, dehiscence. • Acute or Fulminant Hepatitis of any cause - wait until evidence of clinical improvement in the underlying disease process to decrease risk. • Childs Class C cirrhosis or MELD > 15 cirrhosis. • Severe Coagulopathy. Bleeding Disorders and Dental Procedures 50 Year-old-male with no past medical history is scheduled for a dental procedure. He’s had no bleeding problems and his PE is unremarkable. His bleeding time is normal and CBC is normal except for a platelet count of 70,000. What would be the most appropriate management prior to surgery? 1. Proceed with procedure and check platelets 2 hours after completed 2. Transfuse 8 units of platelets to get count >100,000 3. Transfuse 4 units of platelets to get count >100,000 4. Delay elective procedure until cause is determined and corrected Bleeding Disorders and Dental Procedures Thrombocytopenia and Bleeding risk • Risk of bleeding related to the cause of the thrombocytopenia and patients associated conditions. • Delay elective procedures until cause is determined and corrected. • Healthy patients like young women with ITP have lower risk. • Patients with Systemic illnesses: aplastic anemia, chemotherapy induced are at higher risk. • Highest risk is patients with other hemostatic defects like liver disease and patients with sepsis and DIC. Coagulation factors not working. Bleeding Disorders and Dental Procedures Thrombocytopenia and Bleeding risk • A normal platelet count > 150,000/µL isn’t necessary for any procedure. • >100,000 /µL is considered adequate • >50,000 /µL adequate for minor surgeries • Unless other conditions (liver disease, ASA use) are present that can increase risk of bleeding, very few platelets are required to provide adequate hemostasis. • Avoid NSAIDS and Aspirin because they can impair platelet function. Bleeding Disorders and Dental Procedures Anticoagulation 60 year-old-female with a history of a mitral valve replacement 5 years ago is scheduled for a dental procedure. She has no complaints and her physical exam is unremarkable. She takes 5 mg of coumadin per day. What would be the most appropriate test to order? 1. CBC with platelets 2. PT/PTT and INR 3. Bleeding time 4. Liver profile Bleeding Disorders and Dental Procedures Her lab work shows an INR of 3.0. What do you recommend to manage her anticoagulation before surgery? 1. 2. 3. 4. Withhold 4 scheduled doses of coumadin Withhold 8 scheduled doses of coumadin Withhold 6 scheduled dose of coumadin Proceed to procedure without discontinuing coumadin (with good local control) Bleeding Disorders and Dental Procedures The INR is measured the day before dental procedure. What would be the goal of the INR before proceeding to surgery? 1. 2. 3. 4. INR 2.5-3.0 INR 4.0-6.0 INR 1.5-2.0 INR 1.0-1.5 Bleeding Disorders and Dental Procedures Since this patient has a mechanical valve and is at risk for a CVA, when would you recommend the patient to take warfarin after her dental procedure? 1. 2. 3. 4. Immediately after surgery. In 4-5 days. In 1-2 days. In 1 week. Bleeding Disorders and Dental Procedures Anticoagulated Patients and Dental Procedures must consider: 1. The individual patient (liver disease, history of CVA’s, healthy?) 2. The reason for the anticoagulation a. b. c. Deep venous thrombosis Atrial Fibrillation (history of CVA’s?) Prosthetic Valve 3. Nature of the procedure (extraction, how much bleeding?) Bleeding Disorders and Dental Procedures Mechanical heart valves or non-valvular atrial fibrillation • Ideally, have the INR in the low therapeutic range before surgery, but in practice difficult to do. • Don’t normalize the INR because of CVA risk. The longer the window of normalization without heparin the greater the risk of a CVA. • A-Fib: check INR, if in therapeutic range: 2-3, may proceed to surgery with good local control . If supertherapeutic hold several doses. • Mech. Valve: check INR, if in therapeutic range: 2.5-3.5 may proceed to surgery with good local control. Hold several doses if supertherapeutic and recheck INR. • Minor Surgery (extract teeth) with good local control, keep INR < 3.0 Bleeding Disorders and Dental Procedures Anticoagulation Review • ASA continue but if needed stop 1 week before procedure. • Clopidogrel (Plavix-antiplatelet agent) continue but if needed stop 1 week before procedure. • Ticlopidine (Ticlid-platelet aggregation inhibitor) stop 10-14 days before surgery if needed. • Stents (Bare-Metal): At least 1 month of Plavix/ASA. Best 6-12 months. • Drug-Eluting Stents need Plavix, ASA for 1 year. Bleeding Disorders and Dental Procedures Dabigatran (Pradexa) • Thrombin inhibitor taken twice a day. • Normal renal function > 50 cc/min: Stop 1-2 days before surgery. • Abnormal renal function < 50 cc/min: Stop 3-4 days before surgery. • With good local control: Continue or stop PM dose and AM dose day of surgery. Resume night of surgery. Works in 2-3 hours. Bleeding Disorders and Dental Procedures 62 year-old-male with a history of atrial fibrillation on 7.5 mg of coumadin every day is scheduled for a dental procedure (extraction). His INR is 8 and he has no bleeding. What would be the most appropriate management before surgery? 1. 2. 3. 4. 5. Withhold coumadin and wait till INR is 2.0-2.5 Administer Vitamin K 2.5 mg po Administer Vitamin K 5.0 mg IV 1 and 2 1 and 3 Bleeding Disorders and Dental Procedures Two weeks after a dental extraction, the patient comes to your office complaining of a nosebleed for 3 hours that won’t stop. He is back on 7.5 mg of coumadin and you order a stat INR which is 10. The best management for his bleeding would be the following 1. 2. 3. 4. 5. 6. Hold the next 6 doses of coumadin and check the INR in 6 days Admit and administer Vitamin K 10 mg IVP (over 20-60 mins) Admit and administer Vitamin K 5mg SQ Admit and administer fresh frozen plasma (FFP) IV 1 and 2 2 and 4 Bleeding Disorders and Dental Procedures • • • • • Reversing the Anticoagulant Effects of Warfarin Risk of bleeding rises sharply when INR > 5.0 Reduce INR by withholding coumadin or (Vit. K or FFP if needed emergently) Vitamin K > 10 mg can lead to coumadin resistance Vitamin K IV can cause anaphylactoid reactions so infuse slowly Vitamin K 1-2.5 mg po can reverse an INR 5-9 within 24 hours in most patients Bleeding Disorders and Dental Procedures Reversing the Anticoagulant Effects of Warfarin • When the INR > 9.0, a larger dose is needed 5 mg of Vitamin K po • If serious or life-threatening bleeding is present, or if rapid reversal of anticoagulation is required (eg, in preparation for emergency surgery), warfarin should be stopped and 10 mg of vitamin K1 administered by a slow intravenous infusion (eg, over 20 to 60 minutes), supplemented by transfusions of fresh frozen plasma (FFP, initial dose: 2 to 3 units; more as clinically indicated) Bleeding Disorders and Dental Procedures A 30 year-old-female is scheduled for a dental procedure. She has a history of moderately heavy menses and a prolonged bleeding time of 14 minutes. The rest of her lab studies showed the following: Platelet count 400,000 (150 - 450,000) PT 10 sec (control 11) PTT 55 sec (control 30) Mixing studies corrected to 34s (control 30) Factor VIII 25% (10-200% of normal) Bleeding Disorders and Dental Procedures The patient’s diagnosis? 1. Hemophilia A 2. Hemophilia B 3. von Willebrands Disease Management before surgery? 1. VWF Concentrates 2. Packed Red Blood Cells 3. DDAVP 4. 1 or 3 5. 1 or 2 Bleeding Disorders and Dental Procedures von Willebrands Disease • VWD is characterized by mutations that lead to an impairment in the synthesis or function of von Willebrand factor (VWF). There are also acquired forms of VWD. • VWF is necessary for normal platelet adhesion and is either deficient or defective • Autosomal dominent mostly - Some types recessive. The most common of the inherited bleeding disorders • Prevalence of 1% with random lab screening but symptomatic VWD 0.01 % Bleeding Disorders and Dental Procedures von Willebrands Disease • Von Willebrand factor (VWF) binds to platelets and endothelial components, forming an adhesive bridge at sites of endothelial injury. • VWF also contributes to fibrin clot formation by acting as a carrier protein for factor VIII, which has a greatly shortened half-life unless it is bound to VWF. • Type 1 most common form (75%); they produce an inadequate amount of normal VW factor. Type 2 (4 subtypes) have defective VW factor and Type 3, the rarest form, have virtually no VW factor • Most cases are mild and are not screened for Bleeding Disorders and Dental Procedures von Willebrands Disease HISTORY of bleeding very important, tip offs include: nosebleeds, copious bleeding from minor cuts or dental work, easy bruising, excessive menstrual bleeding, or family history of bleeding 5 Screening tests: – – – – Plasma VWF antigen (VWF:Ag) Plasma VWF activity (ristocetin cofactor activity, VWF:RCo) Factor VIII activity (FVIII) and PTT Bleeding Time or Platelet function analyzer (PFA) Bleeding Disorders and Dental Procedures von Willebrands Disease In Type I you usually see: • Prolonged bleeding time or abnormal PFA • Decreased factor VIII which is carried with VWF protein, • prolonged PTT • VWF:ag decreased • VWF:activity decreased Bleeding Disorders and Dental Procedures von Willebrands Disease Tx for Type I: • Mild: DDAVP (desmopressin) nasal spray 2 hrs before surgery. Weight >50 kg: 300 mcg (1 spray each nostril). Weight <50kg: 150 mcg (1 spray in one nostril). • DDAVP given IV: 0.3 mcg/kg in 50 cc Normal Saline over 20minutes 30 minutes before surgery. • DDAVP may use 2-4 doses every 12 hours if needed. • Minor Bleeding or Surgery: VWF Concentrates containing all VWF multimers. – Initial dose 60 ristocetin cofactor units followed by 40 units every 12-48 hours to keep VWF level >30 IU/dl for 3-5 days. Bleeding Disorders and Dental Procedures von Willebrands Disease Type II and III Severe or anticipate Major Surgery or bleeding: VWF Concentrates containing all VWF multimers. • 40 to 60 international units/kg; repeated doses of 20 to 40 international units/kg should be given approximately every 12 hours to maintain a level between 50 to 100 IU/dL of VWF ristocetin cofactor activity • VWF ristocetin cofactor levels of 100 IU/dL activity be maintained for 7 to 14 days Bleeding Disorders and Dental Procedures von Willebrands Disease Antifibrinolytic Agents: 1. Aminocaproic Acid: 50 mg/kg (maximum 5 gram dose) 4 times daily by mouth. 2. Tranexamic acid: 10 mg/kg 3 times daily IV. Topical Agents: 1. Topical Thrombin. 2. Micronized collagen (Avitene), which is available in strips for packing, Bleeding Disorders and Dental Procedures 65 year old female is scheduled for a dental procedure. No personal or family history of bleeding problems. Her pre-operative PTT was 94s (control 34) Other laboratory studies: Prothrombin time 12 sec (control 11) Platlelet count 350,000 (150-400,000) What other studies would you order to help assess her PTT? 1. Anemia panel 2. Mixing study (50-50 mix of patient and normal plasma) to see if PTT gets corrected 3. Factor 8, 9, 11, 12 4. Von Willebrand Factor Antigen, ristocetin cofactor assay activity Bleeding Disorders and Dental Procedures Laboratory studies: Mixing study corrected the PTT immediately Factor 8,9, 11 activity wnl. Factor 12 had 5% activity (60-139% of normal) Will this patient have any bleeding problems during or after surgery? Bleeding Disorders and Dental Procedures • • • • Factor XII Deficiency (Hageman) Autosomal recessive Lab findings: elevated PTT often greater than 100s The PTT may be corrected with addition of normal plasma Despite a high PTT these patients do not have bleeding problems even during major surgery or trauma Bleeding Disorders and Dental Procedures 55 y/o/F with is scheduled for a dental procedure. No personal or family history of bleeding problems. Her pre-operative PTT was 100s (control 34). Labs revealed the following: Mixing study corrected the PTT immediately Factor 8,9, 12 activity wnl Factor 11 had 5% activity (60-130% of normal) Is this patient at risk for bleeding? Bleeding Disorders and Dental Procedures Factor XI Deficiency • • • • • Rare autosomal recessive hereditary disorder More common in the Japanese and Eastern European Jews Lab findings: elevated PTT normal PT and BT PTT is corrected with normal plasma Individuals with partial FXI deficiency (ie, heterozygotes) usually have FXI activity between 20 and 70 % of normal. Those in the higher activity range can have a normal PTT. • Low incidence of spontaneous bleeding but may bleed excessively after surgery or trauma Bleeding Disorders and Dental Procedures Factor XI Deficiency Treatment • FFP (20cc/Kg loading dose and 10 cc/kg daily). • Factor XI replacement therapy to raise the factor XI level to between 30% to 45% of normal. Half-life is long 4 - 5 days, therefore permitting 1 - 2 transfusions per bleeding episode if minor. • Tranexamic acid used as a 5 % mouthwash ,as tablets in an oral dose of 1g or 25 mg/kg, or intravenously in a dose of 10 mg/kg. Doses should be repeated every 6 to 8 hours for a total of 7 days, starting 12 hours before surgery. Replacement therapy is not required. Bleeding Disorders and Dental Procedures 42 y/o F with a history of recurrent bleeding complications from nosebleeds and once after a tooth was pulled. Her pre-op labs: Bleeding time 5 min (<10 min) Platelet Count 290,000 (150,000 - 300,000 per microliter) PTT 32s (control 34) PT 10s (control 11) Her most likely diagnosis is: 1. Factor XII deficiency 2. Factor XI deficiency 3. Hemophilia A (factor VII deficiency) 4. Factor XIII deficiency Bleeding Disorders and Dental Procedures • • • • • Factor XIII deficiency Autosomal recessive trait Defective crosslinking of fibrin Coagulation and bleeding tests are normal Significant bleeding may occur after surgery Replacement therapy with FFP (preferably virusinactivated), cryoprecipitate, or pasteurized plasma concentrate prior to surgery to maintain hemostasis Bleeding Disorders and Dental Procedures A 22 year-old-male with a history of hemophilia A is scheduled for a dental procedure. He has no bleeding problems, his PTT is 65 sec and factor VIII is 10% What replacement therapy do you recommend to decrease his risk of bleeding? 1. DDAVP or Aminocaproic acid 2. Cryoprecipitate 3. Factor VIII concentrate 4. FFP Bleeding Disorders and Dental Procedures • • • • • Hemophilia A (Factor VIII deficiency) X-linked recessive, males usually affected but can occur in females Characterized by bleeding into soft tissues, muscles and weight bearing joints Mild disease, factor VIII >5%, infrequent bleeding, unless surgery Severe disease, factor VIII < 1%, bleed frequently even without trauma Prolonged PTT and all other tests normal Bleeding Disorders and Dental Procedures Replacement Therapy: determined by severity and anticipated bleeding • Severe disease - transfuse factor VIII concentrate to bring factor level to 100% prior to surgery. After the initial dose maintain factor VIII above 50% for 10 - 14 days after surgery • Moderate disease – factor VIII concentrate to get factor VIII around 50%. • Mild disease - DDAVP, Aminocaproic acid (Amicar), Tranexamic acid • Prior to surgery every patient should be screened for the presence of an inhibitor to factor VIII Bleeding Disorders and Dental Procedures A 17 year-old-boy with a family history of Hemophilia A is scheduled for a dental procedure. He’s had no bleeding problems and his PTT is normal at 30 sec (control 31). What would be your preoperative management to decrease his risk of bleeding. His CBC, bleeding time and platelet count are within normal limits. 1. Check Factor 9 level 2. Check Factor 8 level 3. Proceed to surgery since PTT normal, no risk of bleeding 4. Perform mixing studies Bleeding Disorders and Dental Procedures The lab reports that the patients Factor VIII level is 20% (normal is 60-100%). The appropriate management before surgery to decrease his risk of bleeding is which of the following? 1. Mild Hemophilia, treat with factor 8 concentrate 2. Mild Hemophilia but no bleeding risk because factor 8 >5% 3. Mild Hemophilia, treat with DDAVP or Aminocaproic acid because he may still bleed Bleeding Disorders and Dental Procedures A 27 year-old-male with a history of hemophilia B (factor 9 defy) is scheduled for surgery. He has no bleeding problems his PTT is 80 and his factor IX is 1%. What replacement therapy do you recommend to decrease his risk of bleeding? 1. 2. 3. 4. DDAVP or Amicar Cryoprecipitate Factor IX concentrate FFP Bleeding Disorders and Dental Procedures Hemophilia B (Factor IX deficiency, Christmas disease) • X-linked recessive • Clinical features similar to Hemophilia A • Prolonged PTT all other tests normal • Factor assay used to determine: severity, distinguish from factor VIII deficiency, and follow replacement therapy Replacement Therapy: • Severe disease: Factor IX concentrate as in Hemophilia A • Moderate/mild disease: FFP Bibliography • Friedman L, Chopra S, Bonis P. Assessing surgical risk in patients with Liver disease. UpToDate. 2008; version 16.2. • Friedman L. When patients with liver disease need surgery. Internal Medicine 1993; July: 25 - 34. • Patel T. Surgery in the patient with liver disease. Mayo Clin Proc. 1999; 74: 593 - 599. • Ortiz J, Lane C. A Primary Care Approach, Hepatitis C. Hippocrates 2000; November: 40-45. • Tonnesen H, Rosenberg J, et al. Effect of preoperative abstinence on poor postoperative outcome in alcohol misusers: randomized control trial. BMJ. 1999; 318:1311-6. • Friedman LS. The risk of surgery in patients with liver disease. Hepatology 1999; 29: 161 Bibliography • National Heart, Blood, and Lung Institute Expert Panel Report 3 (EPR 3): Guidelines for the Diagnosis and Management of Asthma. NIH Publication no. 08-4051, 2007 • Smetana GW. Preoperative Pulmonary Evaluation. N Engl J Med 1999; 340: 937 - 944. • Stoller JK, Barnes PJ, Hollingsworth H. Management of acute exacerbations of chronic obstructive pulmonary disease. UpToDate. 2009. • Fanta CH, Wood RA, Bochner BS, Hollingsworth H. An overview of asthma management. UpToDate. Topic 547 Version 23.0. 2013 Bibliography • Nadia A Khan, MD, MSc; William A Ghali, MD, MPH; Enrico Cagliero, MD. Perioperative management of diabetes mellitus. Topic 1753 Version 9.0; 2013 UpToDate. • Norman M Kaplan, MD. Perioperative management of hypertension. Topic 3868 Version 6.0; 2012 UpToDate. • Wilson W, et al. Prevention of Infective Endocarditis. A Guideline from the American Heart Association. Circulation. 2007; 115: 1-19. • Fleisher LA, et al. American College of Cardiology/American Heart Association 2007 Guidelines on Perioperative Cardiovascular Evaluation and Care for Noncardiac Surgery: Executive Summary. JACC 2007; 50; 1707-1732. • Eagle KA, Brundage BH, et al. American College of Cardiology/American Heart Association Guidelines for perioperative cardiovascular evaluation for non-cardiac surgery. J Am Coll Cardiol. 1996; 93: 910-948 Bibliography • Kearon C, Hirsh J. Management of anticoagulation before and after elective surgery. New Engl Jour Med. 1997; 336: 1506 1511 • Weibert RT, et al. Correction of excessive anticoagulation with low-dose oral vitamin K1. Ann Intern Med. 1997; 126: 959-62 • Hirsh J. Reversing of the Anticoagulant Effects of Warfarin by Vitamin K. Chest, 1998; 114:1505-1508 • Dunn AS, Turpie A. Perioperative Management of Patients Receiving Oral Anticoagulants. Arch Intern Med. 2003; 163:901-909. Bibliography • Rick M, Leung L, Landaw L. Treatment of von Willebrand disease. UpToDate. 2012. • Rick M, Leung L, Landaw L. Classification and pathophysiology of von Willebrand disease UpToDate. 2012.