Head & Neck Injuries
advertisement

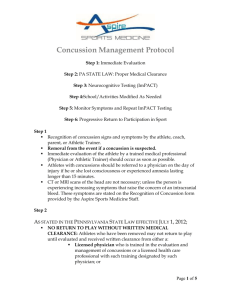
Head, Neck, & Facial Injuries Concussion Defined A brain injury caused by a blow to the head, face, neck or body OR caused by hitting a hard surface/object (ground, bat, ball, opponent, etc) CDC Fact Sheet for Coaches Concussion Facts A concussion is a brain injury All concussions are serious Concussions can occur without a loss of consciousness They can occur in any sport It can be accompanied by one or more signs/symptoms Headaches are the most common symptom Early recognition and proper management can prevent further injury or even death Concussions are most often associated with normal results MRI/CT Scans It is not necessary to lose consciousness to have a concussion Concussion Facts for Children Children are at higher risk of concussions due to continued brain development and decreased muscle tone and coordination Children and teens are more likely to get a concussion than adults Children and teens take longer to recover than adults Youth athletes are at greatest risk of catastrophic consequences from multiple concussions Sports Related Concussions As many as 3.8 million sports-related concussions per year % of all sports related injuries: 6.5% (2002-2009) 15% (2011) NY Daily News.com 20%-50%: Possible due to lack of reporting/hiding sx Rates of incidents (in order): FB, Girls SOC, Boys SOC, Girls BB, Wrestling, Boys BB, Cheer, SB, VB, Baseball 75% classified as mild Concussion Management What to look for: A forceful blow to the head or body AND/OR Any change in their behavior, thinking, or physical functioning Concussion On-Field Evaluation Neck Exam General Neurologic Exam Mental Status Exam On-Field Evaluation: Neck Exam Examine when appropriate: C-spine tenderness Dermatomes/Myotomes Care of the spine takes precedence over head injury evaluation Sideline Evaluation: History Questions Previous Length Time Any concussions of symptoms since fully asymptomatic LOC or Amnesia Sideline Evaluation: Concussion Testing Determine their symptoms Any athlete w/ symptom(s) is to be removed from play until cleared by health care professional! “When in doubt…sit them out!” Determine their level of consciousness LOC >30sec OR decreased consciousness = 911 Determine their orientation Evaluate their memory (before & after) and their concentration Sx’s & Symptoms Severity, duration, & number of sx = most important Headache Dizziness Nausea/Vomiting Blurred or double vision Fatigue Memory problems Amnesia Loss of consciousness Sensitivity to noise or light Vacant stare Delayed responses Decreased alertness & concentration Disorientation Poor coordination Inappropriate emotionality Behavior or personality changes Sideline Evaluation: General Neurological Exam Cranial Nerves: Pupillary evaluation Vision Balance Gait Coordination & Fine Movements Myotomes: Muscle Strength Dermatomes: Sensation 12 Cranial Nerves I. Olfactory: II. Optic: III. Oculomotor: IV. Trochlear: V. Trigeminal: VI. Abducens: VII. Facial: VIII. Vestibularcochlear: IX. Glossopharangeal: X. Vagus: XI. Accessory: XII. Hypoglossal: Smell Vision/sight PEARL Look up Facial sensation/clench jaw Lateral eye movement Smile/frown/raise eyebrows Hearing/balance Swallow Swallow/Say ahh Resisted shoulder shrug Stick out tongue Myotomes C5: Shoulder abduction C6: Elbow flexion/wrist extension C7: Elbow extension/wrist flexion C8: Ulnar deviation, thumb extension T1: Finger abduction/adduction Dermatomes C5: Lateral deltoid/arm C6: Lat. Forearm/thumb/index finger C7: Middle finger/forearm C8: 4th/5th phalanx/medial forearm T1: Medial arm Sideline Evaluation Cont. Orientation Where are we playing? Who are we playing? What is the score? Retrograde Amnesia Anterograde Amnesia What did they eat for breakfast that day? Repeat words & try to recall (girl, dog, green) Concentration Repeat days of week backward, start with today Repeat these #s backward: 419 (914) Post Concussion – General Care Any symptomatic athlete must be held from play Have concussed athlete sit & monitored Do not give them or let them take pain medication Contact parent(s)/guardian(s) Check every 5 min for at least 15 min Must be released to parent/guardian, or other responsible adult party in their absence, with take home instructions Do not leave athlete unattended! Do not let them drive home, especially by themselves Neuroimaging Studies Consider for: Prolonged LOC (30 sec+) Neurological deficits Post-traumatic seizures Worsening symptoms Persistent symptoms > one week Any suspected structural injury CT (acute bleeding) vs MRI (2-3 days: swelling) scans Any positive imaging findings mandates termination of season Seek Immediate Medical Care If: LOC > 30 sec at time of injury, or any LOC after initial trauma Severe or worsening headache Persistent nausea/vomiting Unusual behavior/Persistent mental status alterations Visual disturbances Worsening concussion symptoms Seizures Post Concussion Treatment Complete Physical and Mental Rest: No exercise Absence from school? Decreased school work/postpone reading, homework, and tests No texting, reading, or computer use Communicate about return to learn & play protocols Concussion Risks 3-5x’s more likely to get a subsequent concussion after receiving at least one previous head injury Repeated mild brain injuries occurring over an extended period (i.e., months or years) can result in cumulative neurologic and cognitive deficits Repeated mild brain injuries occurring within a short period (i.e., hours, days, weeks) can be catastrophic or fatal Concussion Risks A recent study found that NFL players who suffer multiple concussions are 30% more likely to suffer clinical depression later in life Concussion Risks Cerebral Edema: Epidural/Subdural Hematoma: Brain swelling Increases intracranial pressure which can cut off oxygen supply to brain Can be fatal if not treated quickly Bleeding in/around the brain Increases intracranial pressure Can be fatal if not treated quickly Signs: Severe headache, dizziness, vomiting, increased size of one pupil, or sudden weakness in an arm or leg Concussion Risks Second impact syndrome: Rare, but fatal condition Occurs when a second head injury is sustained before the first has time to completely heal Rapid brain swelling, which can result in fatal complications 50% chance of death 100% chance of morbidity One or more of their senses may be impaired either temporarily or permanently Story of Death: Case 1 October 1991, a 17-year-old HS FB player was tackled on the last play of the first half of a varsity game and struck his head on the ground. During half-time, he told a teammate that he felt ill and had a headache; he did not tell his coach or athletic trainer. He played again during the 3rd quarter and received several routine blows to his helmet during blocks and tackles. He then collapsed on the field and was taken to a local hospital in a coma. A CT-Scan revealed diffuse swelling of the brain and a small subdural hematoma. He was transferred to a regional trauma center, where attempts to reduce elevated intracranial pressure were unsuccessful, and he was pronounced dead 4 days later. Story of Death: Case 2 August 1993, a 19-year-old college football player reported a headache to family members after a full contact-practice during summer training. During practice the following day he collapsed on the field approximately 2 minutes after engaging in a tackle. He was transported to a nearby trauma center where a CT scan showed diffuse brain swelling and a thin subdural hematoma. Attempts to control the elevated intracranial pressure failed, and he was pronounced brain dead 3 days later. E:60 explores Preston Plevretes' life after tragedy Plevretes, then a 19-year-old sophomore at La Salle, received a second concussion while still symptomatic from his first He was briefly knocked unconscious but then awoke and was combative for 3-5 minutes before lapsing into a coma http://espn.go.com/video/clip?id=espn:516315 1 Concussion Grading Based on severity AND duration of symptoms The more symptoms and the more severe the symptoms are reported = more severe concussion Typically, the more sx the person reports and higher severity dictates a longer recovery A concussion cannot be truly graded until the symptoms have stopped How long will it take to recover? A recent 2011 study looked at how long it took high school athletes symptoms to resolve/clear 23.5% - less than 24 hours 33.8% - 1 to 3 days 20.6% - 4 to 6 days 19.6 - 1 week to 1 month 2.8% - more than a month Post Concussion Syndrome (PCS) Weeks to Months of persistent symptoms Exercise can trigger or aggravate symptoms Symptoms at 3 months: Headache Memory dysfunction Fatigue Irritability Dizziness Impaired concentration Sleep disturbance Depressed mood 42% 36% 30% 28% 26% 25% 20% 9% Pharmacotherapy for PCS Acetominophen, NSAIDs, Excedrin (Only Tylenol post acute concussion) Tricyclic Antidepressants Anti-nausea Medication Sleep Aids Beta-Blockers Calcium Channel Blockers Baseline & Sideline Tests ImPact ® Neurocognitive Test ~20 min test; Computerized; Cost Associated w/ Test Verbal and Visual Memory Reaction time Concentration Symptom Checklist $350-$750/year depending on number of athletes/concussions Limitations: no balance score, cannot be used post-injury on sidelines, long test, no 1-on-1 tester interaction Used by many professional, collegiate, and high school teams Baseline & Sideline Tests – Cont. SAC SCAT3 Cognitive Test (Memory, concentration, orientation) ~5 min test; 1 page; Free Cognitive Test, Balance, Symptom Checklist, Other Evaluation Tools, & Take Home Instructions ~7 min test; 3-4 pgs or use App; Free Standard test for FIFA, Olympic Games, Rugby, & many others NFL Form (NEW) Revised SCAT2 – No take home instructions ~5 min test; 1-2 sheets of paper; Free Standard for all NFL teams Concussion Evaluation Materials Concussion Research University of Pittsburgh Medical Center Neuropsychological Testing (IMPACT) Tests indicated cognitive deficits in asymptomatic athletes following 4 days post concussion Deficits also found in reaction time and processing speed when asymptomatic Research Continued 64 high school athletes with mild concussions (“bell ringers”) 2 groups: < 5 min signs/sx 5-15 min signs/sx Used IMPACT for baseline, 2, 4 & 7 days post injury < 5min signs/sx group: had deficits that gradually improved days 2-7. Back to baseline at day 7 5-15 min signs/sx group: had signif. deficits that gradually improved days 2-7. No return to baseline at day 7! Concussion Legislation 50 states, D.C., & Chicago have adopted concussion laws (2014) Washington State's concussion law became effective in July 2009, named for Zachery Lystedt Zachery Lystedt Late in the first half after a big play, his head hit the ground and he grabbed his helmet in obvious pain as he struggled to get up. He made it to the sideline, sat out for about 15 min, and then went back in for the remainder of the game. http://espn.go.com/video/clip?id=7525526 Lystedt Law & WIAA Guidelines Removal of any athlete suspected of having a concussion from practice/game Athletes cannot return to practice/game until evaluated by a licensed healthcare professional trained in the management of concussions and given written medical authorization Parents and athletes are required to sign a concussion information sheet each year School districts are required to work with the (WIAA) to develop guidelines for safe play Private non-profit youth leagues using public fields must comply as well Who Can Authorize RTP? Medical Doctors (MD) Doctor of Osteopathy (DO) Advanced Registered Nurse Practitioner (ARNP) Physicians Assistant (PA) Licensed Certified Athletic Trainers (ATC/L) Concussion Prevention Teach proper technique/mechanics Ensure proper equipment is worn and that it fits properly Recommend/require mouth guards Teach good sportsmanship Ensure your athletes are in good physical shape (Neck strength!) Return To Play Protocol Assess initial injury, remove athlete from play, sideline SCAT2?, complete rest until sx free DAY 1: 20 min Light Aerobic Activity DAY 2: 30 min Sport Specific Activity DAY 3: Non-Contact Practice with team DAY 4: Full Contact Practice with no return of sx DAY 5: Full Release by school ATC or team physician w/ a return to baseline SCAT2* and symptom free throughout all exertional testing Concussion Education Videos espn.go.com/video/clip?id=5163151 http://vimeo.com/15026404 Preston Plevretes E60 Video NATA’s Educational Video http://www.youtube.com/watch?v=VH2KjItY XUY CNN Big Hits, Broken Dreams Additional Resources CDC Heads NATA NCAA WIAA Up Sport Anatomy: Spine Spinous Process C4-C7 Disc Nerve Root ROM: Neck & Trunk Flexion Extension Lateral Bending Rotation Postural Malalignments: Spine Spinal Injuries: Bulging/Herniated Disc Neck Injuries: Axial Loading A force applied to the top of the head when the neck is partially flexed, which aligns the cervical vertebrae in a straight column Neck is unable to handle the force causing the cervical vertebrae to compress Results in a fracture or dislocation Neck Injuries: Axial Loading Primary cause for catastrophic cervical spine injuries (CSIs) resulting in paralysis. Head-down contact: initiating contact with the top of the helmet Neck Injuries: Axial Loading Spearing: intentional use of a head-down contact technique. Unintentional head-down contact: is the dropping of the head just before contact. Catastrophic CSIs from axial loading are not prevented by players’ standard equipment. Eric LeGrand: http://www.youtube.com/watch?v=NMklSv_VlxE Anthony Conner: http://www.youtube.com/watch?v=ITzuLkpb44k Neck Injuries: On-Field Acute Management Subjective: Observation: Look for crown of helmet or head contact Look at body posture and movement capabilities Palpation: Hx, MOI, C/O, Med/All Red Flags: Tingling, numbness, motor loss, neck pain over spinous process Palpate spinous processes of cervical vertebrae Special Tests: Active ROM: Move hands and feet Resisted ROM/Myotomes: Exp: Grip hand, resisted plantar flexion Dermatomes Dermatomes Neck Injuries: On-Field Acute Management Initial Care for Suspected Neck Injury: Stabilize C-Spine Call 911/Get AED??? Remove face mask If athlete is NOT wearing shoulder pads, remove helmet Monitor A, B, C’s Check for signs of concussion? If face down and not breathing…log roll and begin CPR Facial Injuries: Eye Basketball & baseball are most common sports Most sports related eye injuries are from blunt trauma Exp: Golf ball to the eye Corneal abrasions Exp: Finger to eye during basketball (Seen under blue light w/ stain) Eye Injury – Immediate Referral Sudden decrease in or loss of vision Loss of field of vision Pain w/ movement Diplopia Proptosis of the eye Double Vision Forward Displacement of Eye Light flashes or floaters Irregularly shaped pupil Foreign-body Red eye Blood in/around eye Halos around lights Corneal edema Laceration of the eye lid Broken contact lens or shattered eyeglasses Unable to look up Orbital floor fx possible Facial Injuries: Laceration Seen in basketball, field hockey, baseball, softball, martial arts/boxing, etc Management: Stop bleeding Clean wound Apply Steri-strips Cover wound Refer to Urgent Care for F/U Facial Injuries: Nose Deviated Septum Fracture of Nasal Bone Management: Stop bleeding Observe & Palpate Refer for x-rays Facial Injuries: Avulsed Tooth “Knocked-Out Tooth” Management: Pick up tooth by the crown (the chewing surface) not the root ASAP If dirty, gently rinse tooth with water or saline Replace tooth in socket ASAP(if possible) Hold the tooth in place with fingers or by gently biting down on it Keep tooth moist at all times. Do not use soap or chemicals Do not scrub, dry, or wrap up the tooth Emergency tooth preservation kit Milk Cup of saliva Mouth (next to cheek) Go to nearest available dentist within 30-60 minutes Cauliflower Ear Caused by blunt trauma or repeated friction Causes a hematoma which restricts blood flow to the cartilage, leads to cartilage death/scarring & possible infection As it heals it can shrivel up giving it a cauliflower-like appearance Tx: Drain blood from hematoma, antibiotics, & reduce inflammation Without tx it is permanent, w/ prompt/aggressive tx deformity is unlikely Common in wrestlers, boxers, & martial artists