Emergency Medicine Echocardiography
Cardiac Ultrasound in
Emergency Medicine
Anthony J. Weekes MD, RDMS
Sarah A. Stahmer MD
For the SAEM US Interest Group
Primary Indications
Thoraco-abdominal trauma
Pulseless Electrical Activity
Unexplained hypotension
Suspicion of pericardial effusion/tamponade
Secondary Indications
Acute Cardiac Ischemia
Pericardiocentesis
External pacer capture
Transvenous pacer placement
Main Clinical Questions
What is the overall cardiac wall motion?
Is there a pericardial effusion?
Cardiac probe selection
Small round footprint for scan between ribs
2.5 MHz: above average sized patient
3.5 MHz: average sized patient
5.0 MHz: below average sized patient or child
Main cardiac views
Parasternal
Subcostal
Apical
Wall Motion
Normal
Hyperkinetic
Akinetic
Dyskinetic: may fail to contract, bulges outward at systole
Hypokinetic
Orientation
Subcostal or subxiphoid view
Best all around imaging window
Good for identification of:
– Circumferential pericardial effusion
– Overall wall motion
Easy to obtain – liver is the acoustic window\
Subcostal View
Most practical in trauma setting
Away from airway and neck/chest procedures
Subcostal View
Liver as acoustic window
Alternative to apical 4 chamber view
Subcostal View
Subcostal View
Subcostal View
Angle probe right to see IVC
Response of IVC to sniff indicates central venous pressure
No collapse
–
–
–
–
Tamponade
CHF
PE
Pneumothorax
Parasternal Views
Next best imaging window
Good for imaging LV
Comparing chamber sizes
Localized effusions
Differentiating pericardial from pleural effusions
Parasternal Long Axis
Near sternum
3rd or 4th left intercostal space
Marker pointed to patient’s right shoulder (or left hip if screen is not reversed for cardiac imaging)
Rotate enough to elongate cardiac chambers
Parasternal Long Axis
Parasternal Long Axis View
Parasternal Short Axis
Obtained by 90° clockwise rotation of the probe towards the left shoulder (or right hip)
Sweep the beam from the base of the heart to the apex for different cross sectional views
Parasternal Short Axis View
Parasternal Short Axis
Apical View
Difficult view to obtain
Allows comparison of ventricular chamber size
Good window to assess septal/wall motion abnormalities
Apical Views
Patient in left lateral decubitus position
Probe placed at
PMI
Probe marker at 6 o’clock (or right shoulder)
4 chamber view
Apical 4 chamber view
Marker pointed to the floor
Similar to parasternal view but apex well visualized
Angle beam superiorly for 5 chamber view
Apical 4 chamber view
Apical 2 chamber view
Patient in left lateral decubitus position
Probe placed at
PMI
Probe marker at 3 o’clock
2 chamber view
Apical 2 chamber view
Good look at inferior and anterior walls
Apical 2 chamber view
From apical 4, rotate probe 90° counterclockwise
Good view for long view of left sided chambers and mitral valve
Abnormal findings
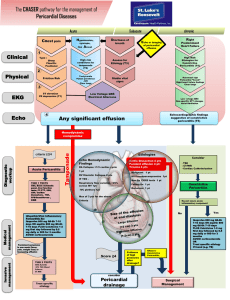
Pericardial Effusion
Case Presentation
45 year old male presents with SOB and dizziness for 2 days. He has a long smoking history, and has complained of a nonproductive cough for “weeks”
Initial VS are BP 88/palp, HR 140
PE: Neck veins are distended
Chest: Clear, muffled heart sounds
Bedside sonography was performed
Echo free space around the heart
Pericardial effusion
Pleural effusion
Epicardial fat (posterior and/or anterior)
Less common causes:
–
–
–
Aortic aneurysm
Pericardial cyst
Dilated pulmonary artery
Size of the Pericardial
Effusion
Not Precise
Small: confined to posterior space,
< 0.5cm
Moderate: anterior and posterior,
0.5-2cm (diastole)
Large: > 2cm
Pericardial Fluid: Subcostal
Clinical features of
Pericardial effusion
Pericardial fluid accumulation may be clinically silent
Symptoms are due to:
–
– mechanical compression of adjacent structures
Increased intrapericardial pressure
Pericardial
Effusion:Asymptomatic
Up to 40% of pregnant women
Chronic hemodialysis patients
– one study showed 11% incidence of pericardial effusion
AIDS
CHF
Hypoproteinemic states
Symptoms of Pericardial
Effusion
Chest discomfort (most common)
Large effusions:
–
–
–
–
–
–
Dyspnea
Cough
Fatigue
Hiccups
Hoarseness
Nausea and abdominal fullness
Cardiac Tamponade
Increased intracardiac pressures
Limitation of ventricular diastolic filling
Reduction of stroke volume and cardiac output
Ventricular collapse in diastole
Tamponade
Hypotension
Abnormal findings
Is the cause of hypotension cardiac in etiology?
Is it due to a pericardial effusion?
Is is due to pump failure?
Unexplained Hypotension
Cardiogenic shock
– Poor LV contractility
Hypovolemia
– Hyperdynamic ventricules
Right ventricular infarct/large pulmonary embolism
– Marked RV dilitation/hypokinesis
Tamponade
– RV diastolic collapse
Cardiogenic shock
Dilated left ventricle
Hypocontractile walls
Hypovolemia
Small chamber filling size
Aggressive wall motion
Flat IVC or exaggerated collapse with deep inspiration
Massive PE or RV infarct
Dilated Right ventricle
RV hypokinesis
Normal Left ventricle function
Stiff IVC
Case presentation ? overdose
27 yo f brought in with “passing out” after night of heavy drinking.
Complaining of inability to breathe!
PE: Obese f BP 88/60 HR 123 Ox
78%
Chest: clear
Ext: No edema
Bedside sonography was performed
Chest pain then code
55 yo male suffered witnessed Vfib arrest in the ED
ALS protocol - restoration of perfusing rhythm
Persistant hypotension
ED ECHO was performed
R sided leads
Non Traumatic
Resuscitation
Direct Visualization
Is there effective myocardial contractility?
– Asystole
–
–
Myocardial “twitch”
Hypokinesis
– Normal
Is there a pericardial effusion?
ECHO in PEA
Perform ECHO during “quick look” and in pulse checks
Change management based on
“positive” findings
Pericardial tamponade
– Pericardiocentesis
Hyperdynamic cardiac wall motion
– Volume resuscitate
ECHO in PEA
RV dilatation
–
–
Hypoxic?? – Likely PE
ECG – IMI with RV infarct?
Profound hypokinesis
– Inotropic support
Asystole
–
–
Follow ACLS protocols (for now)
Early data suggesting poor prognosis
ECHO in PEA
False positive cardiac motion
– Transthoracic pacemaker
– Positive pressure ventilation
Case presentation
Morbidly obese female with severe asthma
Intubated for respiratory failure
Subcutaneous emphysema developed
Bilateral chest tubes placed
Persistent hypotension at 90/palp
Dependent mottling noted
ECHO was performed
Ineffective cardiac contractions
Optimizing Performance
Assessing capture by transthoracic pacemaker
Pericardiocentesis
Transvenous pacemaker placement
Optimizing Performance
Assessment of capture by transthoracic pacemaker
Ettin D et al: Using ultrasound to determine external pacer capture JEM
1999
Case Presentation
70 yo f collapsed in lobby. She was brought into the ED apneic, hypotensive. She was quickly intubated and volume resuscitation begun.
VS: BP 80/50 HR 50 Afebrile
Physical exam : Thin, minimally responsive f.
Clear lungs, nl heart sounds, abdomen slightly distended with decreased bowel sounds. No
HSM, ? Pelvic mass
ECG: SB, LVH, no active ischemia
Clinical questions?
Why is she hypotensive?
Volume loss
?Ruptured AAA
Pump failure
Bedside sonography was performed while we were waiting for the “labs”
Increase HR with PM “on”
What did this tell us?
Normal wall motion
No pericardial/pleural effusion
Good capture with the transthoracic PM
Asystole w/ Transthoracic PM
Optimizing performance
Pericardiocentesis
– Standard of care by cardiology/CT surgery to use ECHO to guide aspiration
US Guided-
Pericardiocentesis
Subcostal approach
–
–
–
Traditional approach
Blind
Increased risk of injury to liver, heart
Echo guided
–
–
Left parasternal preferred for needle entry or…
Largest area of fluid collection adjacent to the chest wall
Large pericardial effusion
Technique
Optimizing performance
Placement of transvenous pacemaker
Aguilera P et al: Emergency transvenous cardiac pacing placement using ultrasound guidance. Ann Emerg
Med 2000
Untimely end
30 yo brought in after he “fell out”
Ashen m with no spontaneous respirations
VS: No pulse, agonal rhythm on monitor
Intubated/CPR
Transvenous pacemaker placed, no capture.
ECHO showed
Penetrating Chest Trauma
Penetrating Cardiac Trauma
Physician’s ability to determine whether there is a hemodynamically significant effusion is poor
Beck’s Triad
– Dependent on patient cardiovascular status
– Findings are often late
Determinants of hemodynamic compromise
– Size of the effusion
– Rate of formation
Penetrating Cardiac Injury
Emergency department echocardiography improves outcome in penetrating cardiac injury.
Plummer D et al. Ann Emerg Med. 1992
28 had ED echo c/w 21 without ED echo
Survival: 100% in echo, 57.1% in nonecho
Time to Dx: 15 min echo, 42 min nonecho
Penetrating Cardiac Injury
The role of ultrasound in patients with possible penetrating cardiac wounds: a prospective multicenter study.
Rozycki GS: J Trauma. 1999
Pericardial scans performed in 261 patients
Sensitivity 100%, specificity 96.9%
PPV: 81% NPV:100%
Time interval BUS to OR: 12.1 +/- 5.9 min
Penetrating Cardiac Trauma
Emergency Department Echocardiography
Improves Outcome in Penetrating Cardiac
Injury
Plummer D, et al. Ann Emerg Med 21:709-712, 1992.
“Since the introduction of immediate ED twodimensional echocardiography, the time to diagnosis of penetrating cardiac injury has decreased and both the survival rate and neurologic outcome of survivors has improved.”
Stab wound to the chest
Penetrating Cardiac Trauma
Echocardiographic signs of rising intrapericardial pressure
– Collapse of RV free walls
– Dilated IVC and hepatic veins
Goal: Early detection of pericardial effusion
–
–
Develops suddenly or discretely
May exist before clinical signs develop
Salvage rates better if detected before hypotension develops
Technical Problems
Subcutaneous air
Pneumopericardium
Mechanical ventilation
Scanning limited by:
– Pain/tenderness
– Spinal immobilization
– Ongoing procedures
Technical Problems
Narrow intercostal spaces
Obesity
Muscular chest
COPD
Calcified rib cartilages
Abdominal distention
Sonographic Pitfalls
Pericardial versus pleural fluid
Pericardial clot
Pericardial fat
Pericardial or Pleural Fluid
Left parasternal long axis:
– Pericardial fluid does not extend posterior to descending aorta or left atrium
Subcostal:
– No pleural reflection between liver and R sided chambers
– A pleural effusion will not extend between to RV free wall and the liver
Pleural and Pericardial fluid
Pleural effusion
Blunt Cardiac Trauma
Cardiac contusion
Cardiac rupture
Valvular disruption
Aortic disruption/dissection
Blunt Cardiac Trauma
Pericardial effusion
Assess for wall motion abnormality
– RV dyskinesis (takes the first hit)
Assess thoracic aorta:
– Hematoma
– Intimal flap
– Abnormal contour
Valvular dysfunction or septal rupture
Cardiac Contusion
Akinetic anterior RV wall
Small pericardial effusion
Diminished ejection fraction
RV Contusion
Blunt Cardiac Trauma
Assess thoracic aorta
– Hematoma
– Intimal flap
– Abnormal contour
– Requires TEE and expertise!
Valvular dysfunction or septal rupture
– Requires expertise beyond our scope
Summary
Bedside ECHO can help assess:
– Overall cardiac wall motion
– Identify clinically significant pericardial effusions
Useful in the assessment of the patient with:
– Unexplained hypotension
– Dyspnea
– Thoracic trauma