The Overactive Bladder - Oklahoma State University Center for
advertisement
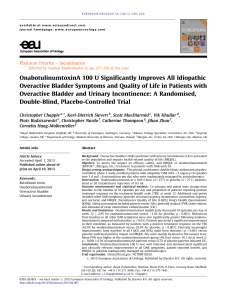
The Overactive Bladder Raji Gill, D.O., M.Sc. Clinical Assistant Professor of Surgery Division of Urology Tulsa Regional Medical Center & Cancer Treatment Centers of America 2002 ICS Terminology: Overactive Bladder OAB defined based on symptoms Urgency, with or without urge incontinence, usually with frequency and nocturia In the absence of pathologic or metabolic conditions that might explain these symptoms ICS = International Continence Society (www.icsoffice.org) OAB Symptoms Frequency • 8 or more visits to the toilet per 24 hours Urination at night • 2 or more visits to toilet during sleeping hours Urgency Urge Incontinence • Sudden, strong desire to urinate • Sudden & involuntary loss of urine OAB Urge Types of Urinary Incontinence urine loss accompanied by urgency resulting from abnormal bladder contractions Stress urine loss resulting from sudden increased intra-abdominal pressure (eg, laugh, cough, sneeze) Mixed symptoms – combination of stress and urge incontinence Sudden increase in intra-abdominal pressure Uninhibited detrusor contractions Urethral pressure Differential Diagnosis: OABMedical andHistory Stress Incontinence and Physical Examination Symptom Assessment Overactive bladder Yes Stress incontinence Frequency with urgency (>8 times/24 h) Yes No Leaking during physical activity; eg, coughing, sneezing, lifting No Yes Amount of urinary leakage with each episode of incontinence Ability to reach the toilet in time following an urge to void Waking to pass urine at night Large (if present) Small Often no Yes Usually Seldom Symptoms Urgency (strong, sudden desire to void) Abrams P, Wein AJ. The Overactive Bladder: A Widespread and Treatable Condition. Erik Sparre Medical AB; 1998. No Estimated Prevalence of OAB in Comparison With Other Selected Chronic Conditions: 1990s Data Condition Millions of Americans Chronic Sinusitis 37 Arthritis 33 Heart Conditions* 21 OAB 17 Asthma 15 Osteoporosis 10 Diabetes 9 Alzheimer’s Disease 5 * Excludes hypertension Payne CK. Campbell’s Urology Updates. 1999;1:1-20. Evans DA et al. Milbank Q. 1990;68:267-289. Bureau of the Census, Population Estimate Data, 1995. National Institutes of Health. Osteoporosis and Related Bone Diseases National Resource Center. Osteoporosis Overview. National Center for Health Statistics. Vital Health Stat. 10(199):1998. Prevalence of OAB in the US 40 Men Women • Overall, 16.6% had symptoms of OAB • Prevalence of OAB increased with age Prevalence (%) 35 30 25 20 15 10 5 0 18–24 25–34 35–44 45–54 55–64 65–74 Age (years) Adapted from Stewart W et al. WHO/ICI 2001. Poster. 75+ Prevalence of OAB: Wet versus Dry 12.2 million (6.1% of the population) Wet (37% of OAB) OAB Dry (63% of OAB) 21.2 million (10.5% of the population) Adapted from Stewart W et al. WHO/ICI 2001. Poster. Diagnosis of OAB A presumptive diagnosis of OAB can be based on – patient history, symptom assessment – physical examination – urinalysis Initiation of noninvasive treatment may not require an extensive further workup Fantl JA et al. Urinary Incontinence in Adults: Acute and Chronic Management. Clinical Practice Guideline No. 2, 1996 Update. Rockville, MD: Agency for Health Care Policy and Research; March 1996. AHCPR publication 96-0682. A Hidden Condition* Many patients self-manage by voiding frequently, reducing fluid intake, and wearing pads Nearly two-thirds of patients are symptomatic for 2 years before seeking treatment 30% of patients who seek treatment receive no assessment Nearly 80% are not examined * Survey conducted by Gallup Group (European Study). Barriers to Treatment Patient misconceptions and fears: “Part of normal aging or everyday life” “Not severe or frequent enough to treat” “Too embarrassing to discuss” “Treatment won't help” Screening and Diagnosing OAB “Do you have bladder problems that are troublesome, or do you ever leak urine?” YES Assess history, symptoms, and test results Establish a diagnosis OAB Screening Can Help Diagnose Other Causes of Bladder Symptoms Local pathology – infection – – – – – diuretics – antidepressants bladder stones bladder tumors interstitial cystitis outlet obstruction Metabolic factors – diabetes – polydipsia Medications – antihypertensives – hypnotics & sedatives – narcotics & analgesics Other factors – pregnancy – psychological issues Fantl JA et al. Urinary Incontinence in Adults: Acute and Chronic Management. Clinical Practice Guideline No. 2, 1996 Update. Rockville, MD: Agency for Health Care Policy and Research; March 1996. AHCPR publication 96-0682. Differential Diagnosis: Physical Examination Perform general, abdominal (including bladder palpation), and neurologic exams Perform pelvic and/or rectal exam in females and rectal exam in males Observe for urine loss with vigorous cough Fantl JA et al. Managing Acute and Chronic Urinary Incontinence. Clinical Practice Guideline. Quick Reference Guide for Clinicians, No. 2, 1996 Update. Rockville, MD: Agency for Health Care Policy and Research; January 1996. AHCPR publication 96-0686. Differential Diagnosis: Laboratory Tests Urinalysis – to rule out hematuria, pyuria, bacteriuria, glucosuria, proteinuria Blood work if compromised renal function is suspected or if polyuria (in the absence of diuretics) is present Fantl JA et al. Managing Acute and Chronic Urinary Incontinence. Clinical Practice Guideline. Quick Reference Guide for Clinicians, No. 2, 1996 Update. Rockville, MD: Agency for Health Care Policy and Research; January 1996. AHCPR publication 96-0686. Care Pathway Working diagnosis? Yes OAB? Yes No Treat if: Consider referral to specialist >8 weeks tx Failed Frequency and urgency, with or without urge incontinence, and normal urinalysis Abrams P. Wein AJ. The Overactive Bladder – A Widespread and Treatable Condition. 1998. Suggested Reasons for Referral Symptoms do not respond to initial treatment within 2 to 3 months Hematuria without infection on urinalysis Recurrent symptomatic UTI Symptoms suggestive of poor bladder emptying Pelvic bladder, vaginal, or urethral pain Evidence of complicated neurologic or metabolic disease Failed previous incontinence surgery Elevated PVR volume Radical pelvic surgery Symptomatic prolapse Prostate problems Surgery planned (2nd opinion) Abrams P. Wein AJ. The Overactive Bladder – A Widespread and Treatable Condition. 1998. Treatment Options Behavioral therapy Medication Combined therapy: behavioral and pharmacologic therapy Minimally invasive therapies – Botulinum A-toxin – Neuromodulation Surgery So when the Drug Rep. visits, which drug do I use? Pharmacotherapy Anticholinergic Agents – – – – – – Oxybutynin (Ditropan) Oxybutynin transdermal (Oxytrol) Tolterodine (Detrol) Solifenacin (Vesicare) Trospium chloride (Sanctura) Darifenacin (Enablex) Oxybutynin (Ditropan) Immediate and long acting form Immediate – TID dosing Long acting XL – once a day, 5 or 10 mg. Side effects – dry mouth, constipation, headache Approved for pediatric use (age 6 or older) Oxybutynin Transdermal (Oxytrol) 3.9 mg patch, twice weekly Similar in effects to po Side effects – less dry mouth but erythema/pruitis Tolterodine (Detrol) Immediate 2 mg. and long acting LA 4 mg dosing Side effects profile similar to oxybutynin Solifenacin (Vesicare) 5 – 10 mg daily dose Side effects – dry mouth, constipation Trospium Chloride (Sanctura) Quaternary amine as opposed to tertiary amine 20 mg BID dose Theoretically harder to pass through blood/brain barrier with less side effects Not metabolized by liver 60% excreted in the urine unchanged Darifenacin (Enablex) M3 selective anticholinergic 7.5 mg or 15 mg once a day Side effects – constipation and dry mouth