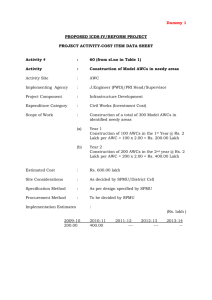
Presentation by Dr Alok Shukla Former Secretary Health
advertisement
Greetings From Chhattisgarh KORIA SARGUJA JASHPUR KORBA BILASPUR DURG RAIGARH JANJGIR RAIPUR MAHASAMUND NAN DGA O N KAWARDHA RAJ A new state Chhattisgarh is born on 1st November 2000 with 16 districts DHAMTARI KANKER BASTAR DANTEWADA GENERAL INFORAMTION Area : Population : Sex ratio : No. of districts : IMR : 146361 Sq. Km. (6 times of Kerala State) 20795956(Census 2001) Rural-80% , Urban-20% SC- 12%, ST-33% 990 female per 1000 male 16 Blocks-146(Tribal –85) 79 per 1000 live births Sex Ratio: 990/1000 Decadal Growth Rate: 18.06 Literacy Persons: 65.18 Male: 77.86 Female: 52.4 SRS 2001 (Released by RGI in October 2002) Item Birth rate (total) Birth Rate (rural) Birth Rate (urban) Death Rate (total) Death Rate (rural) Death Rate (urban) IMR (Total) IMR (Rural) IMR (Urban) Chhattisgarh 26.7 29.2 22.8 9.6 11.2 7.1 79 95 49 MP 31.2 33.2 23.5 10.2 11 7.5 88 94 54 Some Important Indicators of NFHS-2 Fertility Indicators Median age at mariage among women age 20-49 Total Fertility Rate (for the past 3 years) Percent of women with 2 living children wanting another child Current contraceptive use Any method Any modern method Pill IUD Condom Female Sterilization Male Sterilization Any traditional method Unmet need of family planning Percent with unmet need of family planning Percent with unmet need for spacing Quality of family planning services Percent told about side effects of method Percent who recieved follow up services 15.4 2.79 42.6 45 42.3 0.8 1 2.1 35.1 3.3 2.3 13.5 8 15 82.3 Some Important Indicators of NFHS-2 Maternal Health Indicators Antenatal checkup from a health professional 57.5 Antenatal checkup in the first trimester 26.7 Two or more tetanus toxoid injections Iron and folic acid tablets or syrup Percent of births whose mothers were assisted at delivery by a: Doctor ANM/Nurse/midwife/LHV Traditional birth attendant Percent reporting at least one reproductive health problem 58.2 54.9 22.3 9.7 42.7 37.4 Some Important Indicators of NFHS-2 Child Health Indicators Percent of children who received vaccination: BCG DPT(3doses) Polio (3doses) Measles All vaccinations Percent of children with diarrhoea in the past 2 weeks who received oral rehydration salts (ORS) (children under 3 years) Percent of children with acute respiratory infections in the past 2 weeks taken to a health facility or provider (children under 3 years) 74.3 40.9 57.1 40.0 21.8 29.7 61.6 Infrastructure Particulars Area (Sq Kms) Districts Medical Colleges Cities with more than 1 lakh Population Cities with 50000 to 100000 Population Blocks CHC Sub Centers Villages Panchayats Habitations Number 135194 16 2 8 4 146 150 3818 20379 9129 54000 Infrastructur e Gaps •Only 2 Medical Colleges •No District Hospital in 10 out of 16 Districts (Sanctioned in all) •No CHC in 54 out of 146 Blocks Manpower Gaps •Deficiency of over 500 doctors in Public Sector •Major deficiency of paramedics •Very few doctors, and paramedics in Private Sector in rural areas Other Gaps •Poor Monitoring •Poor Managerial and other related skills •Difficult Geographical area, and poor communication The new Strategy •Health Systems Improvement •Improve Routine Programme Monitoring •Capacity Building at all levels Improve Training Infrastructure and Manpower •Community Health Volunteers ("Mitanins') - New Scheme of Community Participation •Improve Infrastructure •Better MIS based on IT •Involve PRIs and ULBs •Mobile Hospitals Important Areas of Reforms Strengthening health intelligence, surveillance, epidemiology and planning Rational Drug Use Policy Uniform Treatment Clinical Protocols Improving internal systems of the Department of Public Health Workforce management and transfer policy Management Information System Mainstreaming of Indian Systems of Medicine esp. tribal medicines into the state health system The Real CNAA Item Estimated in CNAA Last Years Performance Surveyed Target Couples 36,55,371 34,54,248 Protected 21,29,336 17,47,376 58.25 50.58 CPR Need Assesment CVT 4,849 2,629 5,852 NSVT 4,015 795 4,381 CTT 28,711 33,449 38,759 LTT 62,589 50,215 79,215 IUD 1,05,247 86,852 1,05,280 CC 3,64,107 3,50,104 2,78,646 OP 4,52,644 4,16,219 1,80,736 The New Plan of Action - Contraception Uneven distribution of LTT surgeon (reallocation needed) – 63 trained but only 23 working – No LTT surgeon in 2 districts 18 NSVT trained surgeons but only 5 are working - Need to train in large number Skill training in IUD needed for ANMs Training of ANMs needed in counselling skills Days of week fixed in each hospital for Contraceptive Services Requirement of Equipment for Family Planning Laproscopes - 20 are irrepairable IUD Insertion instrument kit - 3841 (3818 rural, 41 urban) NSVT instruments kit (146-18=128) Contraceptives – 23,49,568 OP Cycles – 2,11,77,096 CC pieces The New Plan of Action - Mother and Child Health Microplanning of immunization and ANC sessions Plan to improve outreach Intersectoral coordination Better Logistics including cold chain Out of 146 blocks 66 do not have a vehicle Community Midwifery Improvement in FRUs Requirement of Cold Chain Equipment Walk in Freezer - 1 Walk in Cooler in Bilaspur and Raipur need Replacement Cold Chain Equipment beyond repair – ILR, Deep Freezer 140 L - 78 – ILR, Deep Freezer 300 L -88 Vaccine Vans - 6 Refrigerated Vaccine Van - 1 Vaccine Carriers -1000 The " Indira Swasthya Mitanin" Scheme This is an innovative scheme in which the village people will select a Community Health Volunteer called "Mitanin" to help them in developing a "Village Health Plan" and for "Community Action in Health" "Mitanin" in Chhattisgarhi means a Female Friend Basics of the “Mitanin” Scheme Empowerment Participation Sharing Caring Gender Equity Self Sufficiency Selection Selection by the Community Help by trained Facilitators Approval by Gram Sabha Training by Government Who Can be a “Mitanin” A woman from the same habitation Preferably a married woman Acceptable to the Community Not necessarily educated Role of Mitanin Health Education Leadership in Community Action for Health First Aid & OTC Drugs Treatment of Minor Ailments Timely referral Chief Minister on the "Mitanin" Scheme Relationship with ANM Role of ANM Support to Mitanin Give refresher training every fortnight Visit the Mitanin often Give the Mitanin Legitimacy and Confidence Help her in referral Role of “Mitanin” Be a link between ANM and community Help in National Programmes Provide basic information Relationship with PRIs Role of PRIs Role of “Mitanin” Facilitate approval of Selection by Gram Sabha Provide all inputs' support incl. irrigation of “Mitanin Land” Monitor activities of “Mitanin” Send “Mitanin” for training Ensure supplies of essential medicines Seek help from “Mitanin” for other social sector programmes PRIs may seek information about health status of people Help PRIs in developing a Health Plan Bridge between Gram Panchayat and the community Help PRIs in other Social Sector Programmes Training: Method Participative, Gradual, Repetitive, Fun filled, Practical with field experience, at the pace of learning of “Mitanins” Initiation training: Mainly on attitudes, behavior, communication, working in groups, community participation, concepts in Public Health Refresher training: mainly for knowledge and skills of diagnosis and treatment of common ailments Responsibilities will be increased gradually with “On the Job Training” Achievement so far A group of NGOs and GOs Constituted as a State Advisory Committee Work already started in 16 blocks More than 2000 Mitanins already selected Facilitators manual and the first two Mitanin Training manuals ready Training of Mitanins to begin soon Requirements under Existing RCH Programme Training of at least 20 more surgeons in NSVT Training of ANMs in counselling skills, and IUD insertion Large Scale TBA training IUD insertion kits for ANMs Equipping of FRUs with blood storage and emergency obstetric surgery facilities The proposal for EAG funds Improvement of Training Infrastructure Mobile Hospitals - to improve Outreach Telemedicine - at Pendra Community Midwifery Course Training of Doctors in Anesthesia and money for their insurance coverage Gaps in Training Infrastructure Only 5 out of 16 Districts have DTCs No SIHFW RHFWTC Bilaspur not well equipped 5 AMNTCs, 3 MPW(M)TCs, 4 GNTCs - all buildings need repairs All Centers need Training equipment Capacity building of training faculty needed Requirement of funds for Training Infrastructure SN Item Amount (in lakhs) 1 2 Repair and renovation of existing buildings Construction of new buildings 364 3 Providing modern training aids 165 4 TOT (from money in the Danida Project) Total 70 0 599 Mobile Hospitals Initially 3 mobile hospitals proposed Each mobile hospital will be fully equipped and cost approximately 30 lakh Public - Pvt -NGO partnership – Provided by Govt., managed by Pvt/NGO – Pvt/NGO to provide for recurring expen. – Govt. to give Medicines under National Programmes, and for BPL Run on Predefined routes in Hat-Bazars Telemedicine To begin with Link Medical College Raipur with Pendra Video-conferencing link through VSAT Total Cost 40 lakh Provide good secondary level care at remote locations Community Midwifery Course The "Paramedical Council Act" already passed Affiliation and examination by Chhattisgarh Paramedical Council Course design workshop - cost Rs 1 lakh Equipping all ANMTCs - Rs 30 lakh Stipend to 50% reserved category students - Rs 5.40 lakh Aneshthesia Training of Doctors Course design workshop - Rs 1 lakh Equipping Medical College Raipur for Training - Rs 15 lakh Cost of training of 40 doctors for 3 months - 6.20 lakh Cost of Insurance of Anesthesia trained MBBS doctors - Rs 10 lakh The Proposal for EAG funds S.No. Scheme Cost 1 59900000 2 Improvement in Training Infrastructure Mobile Hospitals 3 Telemedicine 4000000 4 Community Midwifery 3640000 5 Anesthesia Training 3220000 Total 9000000 79760000