The BACJAC
advertisement

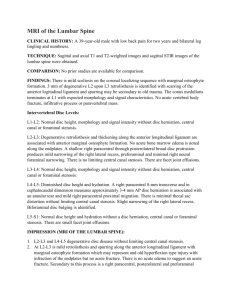
Treatment of Lumbo-sacral steno-instability (esperienza col sistema interspinoso BacJac) Dott. RAFFAELE MANGIALARDI raffaele.mangialardi@tin.it (CBH Bari - S. Camillo Taranto) VERTEBRAL STENOSIS It is a pathological narrowing of the neural channel and/ or the conjugation foramen (caused by bone, arthrosis, and joint changes with: COMPRESSION OF THE NERVOUS STRUCTURES. Two biomechanical types of stenosis: -Dynamic stenosis (manifests itself at spine movements) -Fixed stenosis (in advanced stage) DYNAMIC STENOSIS INSTABILITY PHASE with SPINAL FIXED STENOSIS As the degeneration progresses, it becomes a fixed stenosis. The dimensions of the central and lateral channels reduce because of facet hypertrophy, thickening of yellow ligaments with their bulging in the channel. MECHANICAL PRESSURE on the SPINAL NEUROSTENOSIS STRUCTURES Mechanical irritation (traction compression) Chemical irritation (nucleus) Intra-neural inflammation (ischemia, edema, demyelinization) Functional alterations Lost nervous function Hyperexcitability (pain) (generation of ectopic impulses) Establishing of causes and areas of the DEGENERATIVE STENOSIS No We should consider further anatomic pathological conditions!!! …Clinical recovery becomes impossible. Advanced degenerative changes Severe degenerative disc disease at L5-S1 Severe STENOSIS Stenosis at L4-5 Severe STENOSIS Severe STENOSIS Impact of stenosis on nervous and vascular structures TREATMENT OPTIONS DEPENDING ON THE CASE: 1) Conservative treatment 2) “Major” SURGICAL TREATMENT Between the two: Use of INTERSPINOUS IMPLANTS CONSERVATIVE TREATMENTS Peri-epidural infiltrations NSAID Calcitonin Long-term bed rest Physical therapy (Magnetotherapy, Ionophoresis, TENS, etc) Kineti therapy(postural training, swimming, etc..) Corseta and orthoses “Major” surgical treatments Laminectomy or Laminotomy Laminectomy and/ or foraminotomy Laminectomy + foraminotomy completed by partial arthrectomy plus fusion (in case of severe instability) with intersomatic arthrodesis (screws, plates) Difference between interspinous surgery versus laminectomy Incision 4-6 cm 10-13 cm Surgery above the lamina under the lamina EBL 0 cc few, but present Surgery time 40-60 min 120-150 min Complications 3,3 % 9,7 % Patient is soon able to stand bed rest: minimum 2-3 days Return to activity 7-10 days after approximately 30 days Patient favors this treatment Patient does not favor this treatment Why an interspinous intervention is performed The idea of a device positioned between the spinous processes in order to improve symptomatology of the lumbar stenosis, it stems out of a simple clinical observation: The patients’ symptoms improve while flexion of the spine and they become worse while they hyperextend it: This is where comes the idea of an implant, which would limit the extension, at the same time restricting the channel and lateral formamina, to be inserted during a mini-invasive intervention. Why Interspinous Decompression CLINICAL MOTIVATIONS The symptoms worsen at spine extension and subside in flexion. The patients are feeling better while seated with upper limbs on a table in orthostatic position in slight flexion Why Interspinous Decompression Biomechanical studies confirm the effect: • The in situ load on spinous processes is only 12 – 16% • The implant, inserted into the interspinous space, remains very stable. Why Interspinous Decompression ANATOMICAL MOTIVATION The following happens during extension of the spine: 1) Worsening of the bulging disc 2) Worsening of the recess stenosis 3) Worsening of the minimal listhesis 4) Worsening of local lack of stability Why Interspinous Decompression Dynamic Tests Revealed that the interspinous device Limits extension of the affected area and does not limit the axial rotation and the lateral movement of the spine. Why Interspinous Decompression Studies of the therapeutic mechanism revealed that: – In extension, the channel area, its diameter and subjoint diameter increased by: 18%,10%,48% – The foraminal area and the linear surfca increased, respectively, by 25% and 41% Why Interspinous Decompression Pressure on the disc and load on the facet joints diminish at the treated level. In extension, the pressure on the posterior part of the anulus diminish by 63% The pressure in the nucleus diminishes by 41% The pressure on the facet diminishes by 58% There are no pressure changes in the levels adjacent to the treated one. PATHOLOGIES TREATABLE with interspinous devices • • • • • • • • • • • Lumbar spinal stenosis Degenerative spondylolisthesis (up to Grade I) Baastrups’ syndrome Disc degeneration (also post-operative) Instability and facet syndromes Modic I degeneration, associated with stenosis Disc protrusion, associated with stenosis and recess stenosis Lumbar pain induced by axial load Disc unloading, adjacent to the arthrodesis site Post-discectomy disc assistance Internal lesion of the disc CONTRAINDICATIONS Scoliosis greater than 25° (Cobb) Cauda equina syndrome Isthmic spondylolisthesis Pthological or multiple vertebral fractures Severe obesitas Paget disaese or vertebral metastases Active infection Anatomic conditions that do not allow for a stable implantation of the device. New interspinous approach The B A C J A C Following test using other interspinous devices, which are still ongoing, we started using the BacJac. The BacJac KINEMATICS OF BACJAC Reduces the extension of the treated are in flexion-extension Maintains the range of motion in rotation and lateral bending Does not have any impact on the range of motion of the adjacent segments. Indications for BacJac Intermittent neurogenic claudication (INC) Spondylolisthesis up to grade 1.5 (out of 4, approximately 35%) with INC Baastrup syndrome/ Disc lowering Back pain caused by axial load Facet syndrome Degenerative and/ or iatrogenic disc syndrome Contained herniation of the nucleus Shift of disc adjacent to lumbar arthrodesis BacJac impact on the canal dimensions In extension, it decompresses the nervous structures at the treated level, increasing Spinal canal area by 18%; Diameter of the spinal canal by9%; Sub-articular diameter by 50%; Foraminal area by 25%; Foramen width by 41%. There is no impact on the adjacent levels. BacJac : Action on the disc pressure In extension, it reduces the pressure of the posterior anulus by 63% and of the nucleus by 41% Does not increase pressure on the adjacent discs. BacJac: Impact on the disc height It increase the posterior height of the vertebral disc (at the level of the implant) by 1,5 mm BacJac: Pressure on the adjacent facet In extension, at the implant level, it reduces the pressure on the articular facets by 61%. It does not increase the pressure on the facet of the adjacent segments. BacJac: sagittal balance In neutral position, implants at 1 level or 2 levels, do not change the lumbar curvature, considering the initial pathological curve. Indications/ contraindications for BacJac Indications: – Motor deficit – Lumbar instability – Previous spine surgery Contraindications: – Major low back pain – Symptoms that increase in flexion Surgery details Vertical incision of 3 m, at 1 cm from the median line. No supraspinal ligament damage. At BacJac insertion, remove any anatomic obstacles (such as hypertrophic facets). BacJac instruments Small dilator (5 mm) Big dilator (8 mm) Interspinous divaricator and sizer BacJac inserter with pusher Removal tool BacJac characteristics Load resistant Biocompatibility No MRI and CT artifacts Large contact area Minimal risk of dislocation Biomechanical modules similar to physiological ones BacJac characteristics Unilateral approach Preservation of ligaments Minimal invasive It “positions itself” suring insertion Surgical Technique(BacJac) Lateral or knee-pectoral decubitus Adjusts to the space (lateral X-ray) General, local or peridural anaesthesia Median incision of approximately 3 – 5 cm Partial exposure of the lamina, only on one side, exposure of interspinous ligament. Perforate the interspinous ligament, leaving intact the supraspinal ligament (this way avoiding any possible dislocation of the prosthesis) Post operative Each surgeon follows his own post-op routines, based on age and general conditions. Generally: The patient returns to his activities WHEN HE CAN TOLERATE THEM. For 6 weeks: Do not lift weights. After 20 days: Muscle strengthening exercises, if tolerated. Personal cases Usage of inclusion and exclusion criteria. Clinical examination. Instrument-assisted examinations: X-Rays (standard and dynamic)MRI, CT, EMG. Clinical study: Inclusion criteria Clinical and radiological inclusion criteria: Patients with pain in the lower limbs, gluteus, inguinal pain, with or without lumbar pain. In order to qualify for the study, the patients must be able to sit for 50 minutes without pain, walk for 50 minutes without pain, and have followed conservative treatment for six months. The diagnosis of spinal stenosis (LSS) or lateral stenosis must be confirmed using CT or MRI at 1 or 2 levels. Clinical Study: Exclusion Criteria Clinical and radiological exclusion criteria: Permanent neurological deficit Cauda equina syndrome Major lumbar instability following a previous surgical intervention Major peripheral neuropathy or acute secondary and radicular enervation Spondylolisthesis at more than 1.5 (on a scel from 1 to 4) Systemic infections Paget disease Contraindiations BacJac Constant pain, not related to the dorsal spine position Cauda equina syndrome caused by neural compression, which causes neurogenic intestinal dysfunction (fecal incontinence) or neurogenic urinary dysfunction (urinary retention or incontinence) Major scoliosis(Cobb angle of more than 25°) Isthmic or degenerative spondylolisthesis at the level exceeding 1.5 (on a scale from 1 to 4) at the affected level Pathological or multiple fractures of vertebra and/ or hips Contraindications BacJac Obesity (with the body mass index exceeding 40 kg/ m2); Paget disease of the affected segment or vertebral metastases Active infection Abnormal spinal anatomy, which would prevent from implanting of the device, or anatomy that would cause lack of implant’s stability follwoing the implant Personal cases Average age: Levels: Pathologies: Single level: Double level: 58 years L2-3, L3-4, L4-5, L5-S1 steno-instability, facet stenosis 60 % of cases 40 % of cases Implants (status October 2008): 60 Pre-op MRI: Stenosis, especially at L4-5 Post-op X-ray with 2 BacJacs Results 70% : Improvementas of the first post-op day (the patients can even sleep in prone position, increased walking autonomy, etc). 20%: Partial, but fast improvements * As of now: no patient underwent subsequent surgery (in order to repair the supraspinal ligament or for posterior dislocation of BacJac, or for a subsequent decompression laminectomy). 10%: There is no improvement, but no subsequent surgeries either. Results All patients could stand the day following the surgery (and in 25 cases, the evening of the surgery). Most of the patients (following a control X-ray of the L-S spine in orthostatic position with AP and LL projections) were dsicharged home before the scheduled time (maximal stay: 3 days). CONCLUSIONS REGARDING THE USE OF BACJAC “Minimal” surgical intervention, which is simple and efficient, indicated for patient suffering from claudication secondary to the lumbar canal and/ or conjugation foraminal stenosis. Valid alternative to the traditional surgical treatment. Preserves the anatomical structures. Does not change the situation of the metamers above and below the treated area. CONCLUSIONS REGARDING THE USE OF BACJAC It is a rigid interspinous device, which limits extension of the spine. It does not limit the axial rotation and antero-lateral flexion. It decreases the pressure on the disc and the articular facet and increase the foramina at the affected area. The insertion of the device does not modify the conditions at the adjacent metamers, located above and below. Please do not hesitate to contact us for further information raffaele.mangialardi@tin.it