Chapter 13: Patient Assessment

Chapter 13
Patient Assessment
National EMS Education
Standard Competencies
Assessment
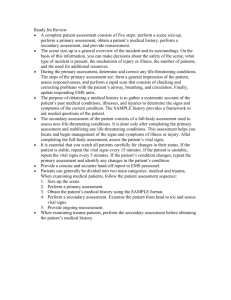
Integrate scene and patient assessment findings with knowledge of epidemiology and pathophysiology to form a field impression.
This includes developing a list of differential diagnoses through clinical reasoning to modify the assessment and formulate a treatment plan.
National EMS Education
Standard Competencies
Scene Size-up
• Scene safety
• Scene management
− Impact of the environment on patient care
− Addressing hazards
− Violence
− Need for additional or specialized resources
− Standard precautions
− Multiple patient situations
National EMS Education
Standard Competencies
Primary Assessment
• Primary assessment for all patient situations
− Initial general impression
− Level of consciousness
− ABCs
− Identifying life threats
− Assessment of vital functions
National EMS Education
Standard Competencies
Primary Assessment (cont ’ d)
• Begin interventions needed to preserve life.
• Integration of treatment/procedures needed to preserve life
National EMS Education
Standard Competencies
History Taking
• Determining the chief complaint
• Investigation of the chief complaint
• Mechanism of injury/nature of illness
• Past medical history
• Associated signs and symptoms
• Pertinent negatives
National EMS Education
Standard Competencies
History Taking (cont ’ d)
• Components of the patient history
• Interviewing techniques
• How to integrate therapeutic communication techniques and adapt the line of inquiry based on findings and presentation
National EMS Education
Standard Competencies
Secondary Assessment
• Performing a rapid full-body exam
• Focused assessment of pain
• Assessment of vital signs
• Techniques of physical examination
• Respiratory system
− Presence of breath sounds
National EMS Education
Standard Competencies
Secondary Assessment (cont ’ d)
• Cardiovascular system
• Neurologic system
• Musculoskeletal system
National EMS Education
Standard Competencies
Secondary Assessment (cont ’ d)
• Techniques of physical examination for all major
− Body systems
− Anatomic regions
• Assessment of
− Lung sounds
National EMS Education
Standard Competencies
Monitoring Devices
• Obtaining and using information from patient monitoring devices including (but not limited to):
− Pulse oximetry
− Noninvasive blood pressure
− Blood glucose determination
− Continuous ECG monitoring
− 12-lead ECG interpretation
− Carbon dioxide monitoring
− Basic blood chemistry
National EMS Education
Standard Competencies
Reassessment
• How an when to reassess patients
• How and when to perform a reassessment for all patient situations
National EMS Education
Standard Competencies
Medicine
Integrates assessment findings with principles of epidemiology and pathophysiology to formulate a field impression and implement a comprehensive treatment/disposition plan for a patient with a medical complaint.
National EMS Education
Standard Competencies
Medical Overview
• Assessment and management of a
− Medical complaint
• Pathophysiology, assessment, and management of medical complaints to include:
− Transport mode
− Destination decisions
Introduction
• One of the most important skills you will develop is the ability to assess a patient.
− Identify your patient ’ s problem(s).
− Set your care priorities.
− Develop a patient care plan.
− Execute your plan.
Sick Versus Not Sick
• Determine whether the patient is sick or not sick.
− If the patient is sick, determine how sick.
• Every time you assess a patient:
− Qualify whether your patient is sick or not sick
− Quantify how sick the patient is
Establishing the Field
Impression
• A determination of what you think is the patient ’ s current problem
− You must be able to communicate and ask the right questions.
• Be a “ detective.
”
Establishing the Field
Impression
• The process must be organized and systematic but still flexible.
− Know when to expand your questioning.
− Know when to focus your questioning.
Medical Versus Trauma
• Medical patients
− Identify chief complaint and sift through medical history.
• Trauma patients
− Medical history may have less impact
− Requires a modified approach
Scene Size-Up
• Involves evaluating the overall safety and stability of the scene
− Safe and secure access into the scene
− Ready egress out of the scene
− Specialty resources needed
Scene Safety
• Ensure the safety and well-being of your
EMS team and any other responders.
− If the scene is not safe, do what is necessary to make it safe.
− Requires constant reassessment
Scene Safety
• Crash-and-rescue scenes often include multiple risks.
− Wear a highvisibility public safety vest.
− Consider specialty reflective gloves, coats, and boots.
Scene Safety
• Ensure that your team can safely gain access to the scene and the patient.
− Consider a snatch and grab.
• Establish a safe perimeter to keep bystanders out of harm ’ s way.
Courtesy of Tempe Fire Department
Scene Safety
• Be wary of toxic substances and toxic environments.
− Proper body and respiratory protection is a must.
Scene Safety
• Potential crime scenes
− Law enforcement should enter first.
− Formulate an escape plan.
− Be aware of violence from bystanders.
− Patients who abuse methamphetamines can be a large threat.
© Paul Chiasson, CP/AP Photos
Scene Safety
• Risks related to the environment include:
− Unstable surfaces
− Snow and ice
− Rain
• Consider the stability of the structures around you.
Courtesy of James Tourtellotte/U.S. Customs & Border Control
Scene Safety
• Ensure safety of the patient and bystanders next.
• When the environment is unfriendly perform assessment, address threats, and move the patient as quickly as possible.
Mechanism of Injury or Nature of Illness
• Mechanism of injury (MOI)
− Forces that act on the body to cause damage
• Nature of illness (NOI)
− General type of illness a patient is experiencing
Mechanism of Injury or Nature of Illness
• Multiple patients or obese patient may warrant additional resources.
− Multiple patients must be triaged.
− Be familiar with specialized resources.
− Assess the need for spinal motion restriction.
Standard Precautions
• Your first priority is your own safety and the safety of other EMS team members.
Standard Precautions
• Treat all patients as potentially infectious.
− Wear properly sized gloves.
− Wear eye protection.
− Wear a HEPA or N95 mask.
− Wear a gown.
− Wash your hands after removing gloves.
Standard Precautions
• Personal protective equipment (PPE)
− Clothing or equipment that provides protection from substances that pose a health/safety risk
• Steel-toe boots
• Helmets
• Heat-resistant outerwear
• Self-contained breathing apparatus
• Leather gloves
Primary Assessment: Form a
General Impression
• Based on initial presentation and chief complaint
• Make conscious, objective, and systematic observations
− Is the patient in stable or unstable condition?
− Is the patient sick or not sick?
Primary Assessment: Form a
General Impression
• Observe level of consciousness.
• Decide whether to implement spinal motion restriction procedures.
• Determine your priorities of care.
• Identify age and sex of the patient.
Primary Assessment: Form a
General Impression
• Treat life threats as you find them
− What additional care is needed?
− What needs to be done on scene?
− When to initiate transport?
− Which facility is most appropriate?
• Assess mental status by using AVPU process
Assess the Airway
• Is airway open and patent?
• Listen for noisy breathing.
• Move from simple to complex:
− Position
− Obstruction
Assess the Airway
• For all unresponsive patients:
− Establish responsiveness.
− Assess breathing.
• If ineffective or absent, open the airway.
• Mechanical means requires an airway adjunct
Assess Breathing
• Is the patient breathing?
− If not, you must breathe for him or her.
− If so, is he or she breathing adequately?
• Consider minute volume.
− Respiratory rate multiplied by the tidal volume inspired with each breath
Assess Breathing
• Assess breathing rate.
− Too fast: greater than 24 breaths/min
− Too slow: 8 –20 breaths/min
• Assess for chest rise and fall.
• Assess for breath sounds.
• Assess for air movement.
Assess Circulation
• Palpate the pulse.
− Count the number of beats in 15 seconds and multiply times four.
• Normal pulse rate for adults is 60 –100 beats/min.
• Bradycardia — rate less than 60 beats/min.
• Tachycardia — rate higher than 100 beats/min.
Assess Circulation
• Force: Normal pulse feels “ full.
”
• Rhythm: Normal rhythm is regular.
• Report your findings:
− Rate
− Force
− Rhythm
• Inspect skin for obvious signs of bleeding.
Assess Circulation
• Capillary refill evaluates ability to restore blood
− To test:
• Place thumb on patient ’ s finger and compress.
• Remove pressure.
• Adequate perfusion: color restored within two seconds.
Assess Circulation
• Assess the skin to evaluate perfusion.
− Color
− Temperature
− Moisture
Assess Circulation
Restoring Circulation
• If a patient has inadequate circulation:
− Restore or improve circulation.
− Control severe bleeding.
− Improve oxygen delivery to the tissues.
Restoring Circulation
• If you cannot feel a pulse, begin CPR until an AED or manual defibrillator is available.
− Follow standard precautions.
− Evaluate cardiac rhythm of any patient in cardiac arrest.
− Oxygen delivery is improved through the administration of 100% supplemental oxygen.
Assess and Control External
Bleeding
• Perform a rapid exam.
− Venous bleeding: steady blood flow
− Arterial bleeding: spurting flow of blood
• Evaluate unresponsive patients by running your gloved hands from head to toe.
Identify and Treat Life Threats
• Determine if a life threat is present and, if so, immediately address it.
− A patient who is dying will:
• Become less aware of surroundings
• Stop making attempts to communicate
• Lose consciousness
• Become unresponsive to external stimuli
• Muscles of the jaw will become slack
Identify and Treat Life Threats
• Conditions that cause sudden death:
− Airway obstruction
− Respiratory arrest
− Severe bleeding
Assess the Patient for
Disability
• Perform a neurologic evaluation.
− Have the patient move all extremities.
• Assess for motor strength and weakness.
• Assess grip strength.
• Assess for loss of sensation.
• Be mindful of exposure concerns.
Perform a Rapid Exam
• Observe for asymmetry/obvious defects.
• Palpate the entire surface of the skull, then down to C7 of the spine.
• Squeeze and roll the shoulder girdles.
• Palate the abdomen and rock the pelvis.
Perform a Rapid Exam
• Grasp each arm at the shoulder girdle and slide your hands down to the wrist.
• Palpate the legs.
• Ask the patient to wiggle fingers and toes.
• Ask the patient if they are bleeding.
Perform a Rapid Exam
• Guidelines:
− Inspect.
− Palpate.
− Auscultate.
− See Skill Drill 13-1 .
• DCAP-BTLS:
− Deformities
− Contusions
− Abrasions
− Punctures/penetration/ paradoxical movement
− Burns
− Tenderness
− Lacerations
− Swelling
Make a Transport Decision
• Identify priority patients.
− Do only what is necessary at the scene and handle everything else en route.
Priority Patients
• Hypoperfusion or shock
• Complicated childbirth
• Chest pain w/systolic
BP < 100 mm Hg
• Uncontrolled bleeding
• Severe pain anywhere
• Multiple injuries
• Poor general impression
• Unresponsive patients
• Responsive but does not or cannot follow commands
• Difficulty breathing
History Taking
• Gain information about the patient and the events surrounding the incident.
• Ask open-ended questions.
• Avoid leading questions.
• Ask age-appropriate questions.
• Be patient.
Patient Information
• Name and chief complaint
• Data required by local EMS system
• Who called 911 and why
• Medical ID jewelry
• Information from medical responders
Techniques for History Taking
• Appearance and demeanor
− Clean, neat, and professional
− Good attitude
− Identify your service and certification level.
− Try to interview in a private setting.
Techniques for History Taking
• Confidentiality
− Be familiar with relevant laws.
• How to address the patient
− Ask how he or she would like to be addressed.
− Err on the side of formality.
− Be familiar with the cultural groups in area.
Techniques for History Taking
© Glen E. Ellman
• Note taking
− Let the patient know that you will be writing information down.
− Position yourself at eye level.
− Maintain good eye contact.
Techniques for History Taking
• Reviewing medical history and information reliability
− Document the source of all information.
− During routine transfers, look over paperwork.
− Evaluate your sources for reliability.
Responsive Medical Patients
• Chief complaint
− Should be recorded in patient ’ s own words
− Should include:
• What is wrong
• Why treatment is being sought
Responsive Medical Patients
• History of illness
− OPQRST
• Onset
• Provocation
• Quality
• Region/radiation/ referral
• Severity
• Time
− SAMPLE
• Signs and symptoms
• Allergies
• Medications
• Pertinent past history
• Last oral intake
• Events that led to injury or illness
Responsive Medical Patients
• “ What made you call 9-1-1?
”
• Patient may have multiple complaints.
• Flesh out history of chief complaint
• Signs and symptoms: what happened and when
• Look for medical ID tags or cards.
Responsive Medical Patients
• Past medical history
− Should include:
• Current medications and dosages
• Allergies
• Childhood illnesses
• Adult illnesses
• Past surgeries
• Past hospitalizations and disabilities
Responsive Medical Patients
• Past medical history (cont ’ d)
− Patient ’ s emotional affect provides insight into overall mental health.
− Determine whether the patient has ever experienced the problem.
• A new problem or condition is best considered serious until proven otherwise.
Responsive Medical Patients
• Current health status
− Made up of unrelated pieces of information
− Ties together past history with history of current event
− Decide which items you want to explore and which you do not
Responsive Medical Patients
• Family history
− Helps establish patterned and risk factors for potential diseases
− Information should be related to the patient ’ s current medical condition.
Responsive Medical Patients
• Social history
− Smoking habits
− Alcohol consumption and drug use
− Sexual habits
− Diet
− Occupation
− Environment
− Travel history
Unresponsive Patients
• Rely on:
− Head-to-toe physical examination
− Normal diagnostic tools
− Family and friends
• Look for clues.
− Pill containers
− Medical jewelry
Trauma Patients
• Life-threatening MOIs
− Ejection from a vehicle
− Death of another patient in same vehicle
− Falls of greater than
15 ′ to 20′ or three times patient ’ s height
− Vehicle rollover
− High-speed vehicle crash
− Vehicle-pedestrian collision
− Motorcycle crash
− Penetrating wounds to head, chest, or abdomen
© Mark C. Ide
Trauma Patients
© Jones & Bartlett Learning.
Photographed by Kimberly Potvin
© Corbis © Dan Myers, Figure
© Jack Dagley
Photography/ShutterStock, Inc.
© Larry St. Pierre/ShutterStock, Inc., © micheal ledray/ShutterStock, Inc.
Trauma Patients
• High-priority infant or child MOIs:
− Falls from more than
10 ′ or two to three times the child ’ s height
− Fall of less than 10 ′ with loss of consciousness
− Medium- to highspeed vehicle crash
− Bicycle collision
Trauma Patients
• Two or more serious
MOIs increase the chance of a serious or fatal injury.
• In an MVC, determine whether seat belts and/or air bags were involved.
− Improperly installed child seats can be useless.
© Thinkstock/Getty Images
Patients with Minor Injuries or
No Significant MOI
• If a patient shows signs of systemic involvement, continue with assessment.
Review of Body Systems
• General symptoms
− Ask questions regarding:
• Fever
• Chills
• Malaise
• Fatigue
• Night sweats
• Weight variations
Review of Body Systems
• Skin, hair, and nails
− Rash, itching, hives, or sweating
• Musculoskeletal
− Joint pain, loss of range of motion, swelling, redness, erythema, and localized heat or deformity
Review of Body Systems
• Head and neck
− Severe headache or loss of consciousness
− Eyes
• Visual acuity, blurred vision, diplopia, photophobia, pain, changes in vision, and flashes of light
Review of Body Systems
• Head and neck (cont ’ d)
− Nose
• Sense of smell, rhinorrhea, obstruction, epistaxis, postnasal discharge, and sinus pain
− Throat and mouth
• Sore throat, bleeding, pain, dental issues, ulcers, and changes to taste sensation
Review of Body Systems
• Endocrine
− Enlargement of the thyroid gland
− Temperature intolerance
− Skin changes
− Swelling of hands and feet
− Weight changes
− Polyuria, polydipsia, polyphagia
− Changes in body and facial hair
Review of Body Systems
• Chest and lungs
− Dyspnea and chest pain
− Coughing, wheezing, hemoptysis, and tuberculosis status
− Previous cardiac events
− Pain or discomfort
− Orthopnea, edema, and past cardiac testing
Review of Body Systems
• Hematology
− History of anemia, bruising, and fatigue
• Lymph nodes
− Tender and enlarged lymph nodes
Review of Body Systems
• Gastrointestinal
− Appetite and general digestion
− Food allergies and intolerances
− Heartburn, nausea and vomiting, diarrhea
− Hematemesis
− Bowel regularity, changes in stool, flatulence,
− Jaundice
− Past GI evaluations and tests
Review of Body Systems
• Genitourinary
− Dysuria
− Increased frequency of urination, urgency
− Nocturia
− Hematuria
− Polyuria
− Pain to the flank and suprapubic region
Review of Body Systems
• Genitourinary (cont ’ d)
− Men
• Erectile dysfunction, fluid discharge, and testicular pain
− Females
• Menstrual regularity, last menstrual period, dysmenorrhea, vaginal discharge, abnormal bleeding, pregnancies, and contraception use
Review of Body Systems
• Neurologic
− Seizures or syncope, loss of sensation, weakness in extremities, paralysis, loss of coordination or memory, and muscle twitches
− Facial asymmetry
− If you suspect stroke or TIA, use Cincinnati
Stroke Scale.
Review of Body Systems
• Psychiatric
− Depression, mood changes
− Difficulty concentrating
− Anxiety, irritability
− Sleep disturbances, fatigue
− Suicidal or homicidal tendencies
Clinical Reasoning
• Combines knowledge of anatomy, physiology, pathophysiology, and patient ’ s complaints
• Pay attention to signs or symptoms that are inconsistent with working diagnosis.
− Differential diagnosis – a working hypothesis of the nature of the problem
Communication Techniques
• Encourage dialogue.
− Use layperson terminology.
Communication Techniques
Communication Techniques
• Empathetic response
− Put yourself in the patient ’ s shoes.
− Do not hesitate to communicate your feelings.
Communication Techniques
• Ask about feelings.
− Tired, depressed, etc.
− Validate the patient ’ s feelings.
− Be empathetic but effective.
Communication Techniques
• Getting more information
− Question region or location of pain.
− Question quality of abdominal pain.
− Add, delete, and modify questions.
− Avoid close-ended and leading questions.
− Try to be orderly and systematic.
Communication Techniques
• Asking direct questions
− If you need a date, time, etc., ask for it.
• Applying clinical reasoning
− Critical thinking consists of:
• Concept formation
• Data interpretation
• Application of principles
• Reflection in action
• Reflection on action
Communication Techniques
• Applying clinical reasoning (cont ’ d)
− Think and perform well under pressure.
− Be a patient listener.
− Communicate with patients.
− Look for nonverbal communication.
Getting a History on Sensitive
Topics
• Alcohol and drug abuse
− Patients may give an unreliable history.
− Alcohol can mask signs and symptoms.
− Keep a professional attitude.
© Jack Dagley Photography/ShutterStock, Inc.
Getting a History on Sensitive
Topics
• Physical abuse, domestic abuse, and sexual assault
− Required to report
− Look for clues.
− Always call law enforcement.
− Maintain evidence per protocol.
Getting a History on Sensitive
Topics
• Sexual history
− Talk to the patient in private.
− Keep your questions focused.
− Do not interject opinions or biases.
− Treat with compassion and respect.
Cultural Competence
• Common barriers to communication:
− Race
− Ethnicity
− Age
− Gender
− Language
− Education
− Religion
− Geography
− Economic status
Cultural Competence
• Respect ideas and beliefs.
• Consider dietary practices.
• Obtain consent.
• Provide best possible care for all patients.
• Research prevalent groups in your area.
• Remember the importance of manners.
Special Challenges in History
Taking
• Silence
• Overly talkative patients
• Patients with multiple symptoms
• Anxious patients
• Reassurance
• Anger and hostility
• Intoxication
• Crying
• Depression
• Sexually attractive patients
• Confusing behaviors or histories
Special Challenges in History
Taking
• Limited education or intelligence
• Language barriers
• Hearing problems
• Visual impairment/ blindness
• Family and friends
Age-Related Considerations
• Pediatric patients
− Include child in the history-taking process.
− Be sensitive to the fears of the parents.
− Pay attention to the parent-child relationship.
Age-Related Considerations
• Pediatric patients (cont ’ d)
− Tailor your questions to the age of the child.
• Neonates/infants: maternal history and birth history
• 3 to 5 years: performance in school
• Adolescent: risk-taking behaviors, self-esteem issues, rebelliousness, drug and alcohol use, and sexual activity
− Gather an accurate family history.
Age-Related Considerations
• Geriatric patients
− Accommodate sensory losses.
− Patients tend to have multiple problems.
• May have multiple chief complaints
• May take a multitude of medications
Age-Related Considerations
• Geriatric patients (cont ’ d)
− Symptoms may be less dramatic.
− Consider including a functional assessment.
• Assessment of mobility
• Upper extremity function
• Activities of daily living
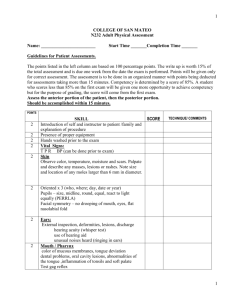
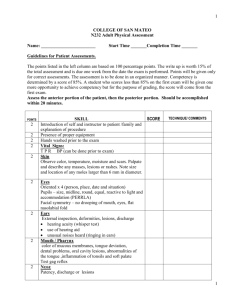
Secondary Assessment
• Process by which quantifiable, objective information is obtained from a patient about his or her overall state of health
− Consists of two elements:
• Obtaining vital signs
• Performing a head-to-toe survey
Secondary Assessment
• Not every aspect will be completed in every patient.
− Factors to consider:
• Location
• Positioning of the patient
• The patient ’ s point of view
• Maintaining professionalism
Assessment Techniques
Inspection
− Looking at the patient
• Palpation
− Touching to obtain information
• Pulses: use finger
• Skull: use palms
• Skin: use back of hand
Assessment Techniques
• Percussion
− Striking surface of the body, typically where it overlies various body cavities
− Detects changes in the densities of the underlying structures
− See Skill Drill 13-2 .
Assessment Techniques
• Auscultation
− Listening with a stethoscope
− Requires:
• Keen attention
• Understanding of what “ normal ” sounds like
• Lots of practice
Vital Signs
• Pulse
− Assess rate, presence, location, quality, regularity
− To palpate, gently compress an artery against a bony prominence.
• Count for 15 minutes and multiply by four.
• Check for central pulse in unresponsive patients.
Vital Signs
Vital Signs
• Respiration
− Assess rate by inspecting the patient ’ s chest
− Quality
• Pathologic respiratory patterns or rhythms
• Tripod positioning, accessory muscle use, retractions
− Rate should be measured for 30 seconds and multiplied by two for pediatric patients.
Vital Signs
• Blood pressure
− Product of cardiac output and peripheral vascular resistance
• Systolic pressure
• Diastolic pressure
− Measured using a cuff
− Ideally should be auscultated
Vital Signs
• Temperature
− When measuring the tympanic membrane temperature:
• External auditory canal must be free of cerumen.
• Position the probe so the infrared beam is aimed at the tympanic membrane.
• Wait 2-3 seconds until temperature appears.
Vital Signs
• Pulse oximetry
− Should never be used as an absolute indicator of the need for oxygen
− Measures percentage of hemoglobin saturation
Equipment Used in the
Secondary Assessment
• Stethoscope
• Blood pressure cuff
(sphygmomanometer)
• Capnography
• Glucometry
• Ophthalmoscope
• Otoscope
• Scissors
• Reliable light source
• Gloves
• Sheet or blanket
Equipment Used in the
Secondary Assessment
• Stethoscope
− Acoustic: blocks out ambient sounds
− Electronic: converts sound waves into electronic signal and amplifies them
© Denis Pepin/ShutterStock, Inc.
Equipment Used in the
Secondary Assessment
• Blood pressure cuff
− Measurement of blood pressure
− Consists of inflatable cuff and manometer
(pressure meter)
− Use the appropriate size!
© WizData, Inc./ShutterStock, Inc.
Equipment Used in the
Secondary Assessment
• Ophthalmoscope
− Allows you to look into patient ’ s eyes
− Consists of concave mirror and battery-powered light
− Requires dilation of pupils and diagnostic expertise
© Kenneth Chelette/ShutterStock, Inc.
Equipment Used in the
Secondary Assessment
• Otoscope
− Evaluates ears of a patient
− Consists of head and handle
Physical Examination
• Look for signs of significant distress
• Other aspects:
− Dress
− Hygiene
− Expression
− Overall size
− Posture
− Untoward odors
− Overall state of health
© Jones & Bartlett Learning. Courtesy of MIEMSS.
Physical Examination
• Terms to describe the degree of distress:
− No apparent distress
− Mild
− Moderate
− Acute
− Severe
• Terms to describe the general state of a patient ’ s health:
− Chronically ill
− Frail
− Feeble
− Robust
− Vigorous
Full-Body Scan
• A systematic head-to-toe examination
• Patients who should receive:
− Sustained a significant MOI
− Unresponsive
− Critical condition
• See Skill Drill 13-3 .
Focused Assessment
• Performed on patients who have sustained nonsignificant
MOIs and are responsive
• Focus on the immediate problem.
Mental Status
• For any patient with a “ head ” problem, assess and palpate for signs of trauma.
− Assess the patient in four areas:
• Person
• Place
• Day of week
• The event
Mental Status
• Use the
Glasgow
Coma Scale
− Assigns point value for eye opening, verbal response, and motor response
Mental Status
• Mental status examination
− General appearance
− Speech and language patterns
− Mood
− Thoughts and perceptions
− Information relevant to thought content
− Insight and judgment
− Cognitive function (attention and memory)
Skin
• Serves three major functions
− Regulates the temperature of the body
− Transmits information from the environment to the brain
− Protects the body from the environment
Skin
• Epidermis (outermost layer)
− Barrier against water, dust, microorganisms, and mechanical stress
• Dermis
− Composed of collagen and elastic fibers, and a mucopolysaccharide gel
− Divided into: Papillary dermis and reticular layer
Skin
Skin
• Examine:
− Color
− Moisture
− Temperature
− Texture
− Turgor
− Significant lesions
• Evidence of diminished perfusion:
− Pallor
− Cyanosis
− Diaphoresis
− Vasodilation
(flushing)
Skin
• Pallor: poor red blood cell perfusion to the capillary beds
• Vasoconstriction: indicated by pale skin
• Cyanosis: low arterial oxygen saturation
• Mottling: severe hypoperfusion and shock
Skin
• Ecchymosis: localized bruising or blood collection within or under the skin
• Turgor: relates to hydration
• Skin lesions: may be only external evidence of a serious internal injury
Hair
• Examine by inspection and palpation.
− Note:
• Quantity
• Distribution
• Texture
• Note:
− Color
− Shape
− Texture
− Presence or absence of lesions
− Normal nail should be firm and smooth.
Nails
Head
• Cranium: contains the brain
− Occiput: posterior portion
− Temporal regions: each side of the cranium
− Parietal regions: between temporal regions and occiput
− Frontal region: forehead
Head
• The scalp covers the cranium.
• Meninges: suspend the brain and spinal cord (dura matter, arachnoid, pia matter)
• Cerebrospinal fluid: fills between meninges
Head
• Inspect and feel the entire cranium.
− Deformity
− Asymmetry
− Warm, wet areas
− Tenderness
− Shape and contour
− Scars or shunts
© E. M. Singletary, M.D. Used with permission.
Head
• Evaluate the face.
− Color
− Moisture
− Expression
− Symmetry and contour
− Swelling or apparent areas of injury
− DCAP-BTLS
− See Skill Drill 13-4 .
Eyes
• Assess functions of CNS.
• Anterior chamber
• Posterior chamber
• Inspect and palpate the upper and lower orbits.
Eyes
Eyes
• Note periorbital ecchymosis
(raccoon eyes).
• Assess visual acuity
− Snellen ( “ E ” ) chart
− Light/dark discrimination
− Finger counting
Eyes
• Assess pupils.
− Normally round and equal size
− Pupils should react instantly to change in light level.
− Check for size, shape, and symmetry, and reaction to light.
Ears
• Involved with hearing, sound perception, and balance control
• Includes:
− External ear
− Middle ear
− Inner ear
Ears
Ears
• Assess for changes in hearing perception, wounds, swelling, and drainage.
− Assess mastoid process of the skull for discoloration and tenderness.
− Examine by using an otoscope
(see Skill Drill 13-7 ).
• Nasal cavity is divided into two chambers
− Each chamber contains three layers of bone.
− Assess anteriorly and inferiorly.
Nose
Nose
• Look for:
− Asymmetry
− Deformity
− Wounds
− Foreign bodies
− Discharge or bleeding
− Tenderness
− Evidence of respiratory distress
Throat
• Evaluate mouth, pharynx, and neck
− Prompt assessment is mandatory in patients with altered mental status.
− Assess for a foreign body or aspiration.
• Be prepared to assist with manual techniques and suction.
Throat
• Mouth
− Lips
− Symmetry
− Gums
− Look for cyanosis around the lips.
• Inspect airway for obstruction.
• Tongue
− Size
− Color
− Moisture
• Maxilla and mandible
− Integrity
− Symmetry
Throat
• Oropharynx
− Discoloration
− Pustules
− Unusual odors on the breath
− Fluids that might need suctioning
− Edema and redness
Throat
• Neck
− Symmetry
− Masses
− Venous distention
− Palpate carotid pulses.
− Palpate the suprasternal notch .
− See Skill Drill 13-8 .
Cervical Spine
• Consider MOI
− Evaluate for:
• Pain
• Altered mental status
• Loss of consciousness at the time of the event
Cervical Spine
• Inspect and palpate.
− Stop exam if pain, tenderness, or tingling results.
− Assess range of motion when there is no potential for serious injury.
• Passive exam
• Active exam
Chest
• Contains lungs, heart, and great vessels
• Three phases of exam
− Chest wall exam
− Pulmonary evaluation
− Cardiovascular assessment
− See Skill Drill 13-9 .
Chest
• Check for:
− Symmetry
− Respiratory effort
− Signs of obstruction
− General shape of the chest wall
− Signs of abnormal breathing
− Chest deformities
− Tenderness or crepitus
Chest
• Auscultate breath sounds.
− Normal
− Tracheal
− Bronchial
− Bronchovesicular
− Vesicular
− Adventitious
• Wheezing, rales, rhonci, stridor, pleural friction rubs
Chest
• Are sounds:
− Dry or moist?
− Continuous or intermittent?
− Course or fine?
• Are breath sounds diminished or absent?
− In a portion of one lung or entire chest?
− If localized, assess transmitted voice sounds.
Chest
• Assess respiratory rate, depth, and effort.
− Check for accessory muscle use, retractions, or ventilatory fatigue.
− Check for jugular venous distention (JVD).
Cardiovascular System
• Circulates blood throughout the body
− Plasma
− Red blood cells
− White blood cells
− Platelets
Cardiovascular System
• System of tubes:
− Arteries
− Aterioles
− Capillaries
− Venules
− Veins
• Two circuits:
− Systemic circulation
• Carries oxygenrich blood
− Pulmonary circulation
• Carries oxygenpoor blood
Cardiovascular System
• Cardiac cycles involves:
− Cardiac relaxation (diastole)
− Filling
− Contraction (systole)
• Heart consists of four chambers
− Two atria
− Two ventricles
Cardiovascular System
Cardiovascular System
• The contraction and relaxation of the heart generates heart sounds.
Cardiovascular System
Cardiovascular System
• Splitting: events on the right of the heart usually occur later than those on the left
− Creates two discernible sounds
• Heart sounds can be heard in:
− Parasternal areas
− Region superior to the left nipple
− Refer to Skill Drill 13-10 .
Cardiovascular System
• Korotkoff sounds: related to blood pressure
− There are 5 (1st and 5th are significant)
• First: thumping of the systolic
• Fifth: disappears as the diastolic pressure drops below that created by the blood pressure cuff
Cardiovascular System
• Bruit: abnormal “ whoosh ” -like sound
− Turbulent blood flow through narrowed artery
• Murmur: abnormal “ whoosh ” -like sound
− Turbulent blood flow around a cardiac valve
− Graded by range of intensity from 1 to 6
Cardiovascular System
• Arterial pulses are an expression of systolic blood pressure.
− Palpable where artery crosses bony prominence
• Venous pressure tends to be low.
− Assess extremities for signs of obstruction or insufficiency.
Cardiovascular System
• Jugular venous distention (JVD)
− With penetrating left chest trauma, may indicate cardiac tamponade
− With pedal edema, consider heart failure.
− Note how much distention is present.
Cardiovascular System
• Pay attention to arterial pulses.
• Obtain blood pressure and repeat.
− Note history and class of hypertension.
Cardiovascular System
• Palpate and auscultate carotid arteries.
• Listen where cardiac valves are located:
− Aortic valve: right of the sternum
− Pulmonic valve: left of the sternum
− Tricuspid valve: lower left sternal border
− Mitral valve: lateral to the lower left sternal border
Cardiovascular System
• For a suspected heart problem, assess:
− Pulse
− Skin
− Breath sounds
− Baseline vital signs
− Extremities
Cardiovascular System
• The definition of normal and abnormal findings is different in a neonate or infant.
− Neonates often have cyanosis following birth.
− “ Abnormal ” heart sounds may be a normal variant.
Abdomen
• Divided into imaginary quadrants
• Contains:
− Organs of digestion
− Organs of urogenital system
− Significant neurovascular structures
Abdomen
• Peritoneum: a well-defined layer of fascia made up of the parietal and visceral peritoneum
− Intraperitoneal organs
− Extraperitoneal organs
Abdomen
• Organs are organized by viewing the abdominal wall in a subdivided fashion.
− Quadrants
• Left upper quadrant
• Right upper quadrant
• Left lower quadrant
• Right lower quadrant
Abdomen
• Abdomen can also be divided by ninths.
Abdomen
• Three basic mechanisms produce pain:
− Visceral pain
− Inflammation
− Referred pain
• Appropriate and relevant history is critical.
Abdomen
• Inspect and palpate the abdomen.
− Tightness: internal bleeding or inflamed organ
− Upper left pain: ruptured spleen
− Lower left pain: diverticulitis
− Lower right pain: appendicitis
− Generalized pain in women: obstetric or gynecologic problem
Abdomen
• Orthostatic vital signs (tilt test)
− Blood pressure and pulse are taken in the supine and sitting or standing positions.
− Determines extent of volume depletion
• If volume-depleted, there is not enough circulating blood to push into core circulation
Abdomen
• Orthostatic vital signs (tilt test) (cont ’ d)
− Generally considered positive if:
• Decrease in systolic pressure
• Increase in diastolic pressure of 10 mm Hg
• Increase in pulse rate by 20 beats/min
Abdomen
• Examine the area of complaint last.
− Work slowly.
− Avoid quick movements.
− Proceed in a systematic fashion.
− Refer to Skill Drill 13-11 .
Abdomen
• Inspect:
− Skin
− Contour and appearance
− Symmetry
− Swelling/bruising
− Discoloration in periumbilical area or along the flanks
− Rash or signs of allergic reaction
− Scars
− Wounds
− Striae
− Dilated veins
− Distention
− Localized masses
Abdomen
• Abdomen can be described as:
− Flat
− Rounded
− Protuberant (bulging out)
− Distinguish from obesity
− Scaphoid
− Pulsatile
Abdomen
• Auscultation
− Setting must be quiet.
− Note bowel sounds.
• Hyperactive, hypoactive, increased, decreased, absent
− Bruits
Abdomen
• Palpation
− Palpate each quadrant gently but firmly.
• Should appear soft without tenderness or masses.
− Guarding: contraction of abdominal muscles
− Rebound tenderness: pain upon release
− Abdominal rigidity: peritoneal irritation and guarding
Abdomen
• Palpation (cont ’ d)
− To palpate the liver:
• Place left hand behind patient, parallel to right 11th and 12th ribs
• Place right hand on right abdomen below rib cage.
• Ask patient to take a deep breath.
• Try to feel the liver edge.
Abdomen
• Palpation (cont ’ d)
− To palpate the gallbladder:
• Use same technique as for liver
• Response indicating pain may mean possible inflammation
• When patient takes deep breath, move fingers under liver edge
Abdomen
• Palpation (cont ’ d)
− To palpate the spleen:
• With left hand, reach over and around patient
• Press forward lower left rib cage and adjacent soft tissues.
• With right hand below costal margin, press toward the spleen.
Abdomen
• Aortic aneurysm
− May be seen pulsating in the upper midline
− Do not palpate an obvious pulsatile mass.
• Hernia
− Place patient in supine position and raise the head and shoulders.
• Bulge of hernia will usually appear.
Female Genitalia
• Consists of:
− External genitalia
− Ovaries
− Fallopian tubes
− Uterus
− Vagina
Female Genitalia
• Limited and discreet assessment
− Reasons to examine include:
• Life-threatening hemorrhage
• Imminent delivery in childbirth
− Assessment includes:
• Palpating the bilateral inguinal regions
• Palpating the hypogastric region
Female Genitalia
• Reasons for pain on palpation include:
− Ectopic pregnancy
− Complications of third trimester pregnancy
− Nonpregnant ovarian problems
− Pelvic infections
Male Genitalia
• Consists of:
− Reproductive ducts
− Testes
− Urethra
− Prostate
− Penis
Male Genitalia
• Limited exam with partner present.
− Assess for bleeding, injury, or fracture.
− Note inflammation, discharge, swelling, or lesions.
− Priapism: prolonged erection
− Look for evidence of urinary incontinence.
Musculoskeletal System
• Joints: areas where bone ends abut each other and form a kind of hinge
• Skeletal muscles: used to flex and extend joints
− Joints become more vulnerable to injury, stress, and trauma as they age.
Musculoskeletal System
• Common injuries:
− Fractures
− Sprains
− Strains
− Dislocations
− Contusions
− Hematomas
− Open wounds
Musculoskeletal System
• Note:
− Structure and function
− Limitation or pain in range of motion
− Bony crepitance
− Inflammation or injury
− Obvious deformity
− Diminished strength
− Atrophy
− Asymmetry
− Pain
− Refer to Skill Drill
13-12 .
Musculoskeletal System
• Problems with the shoulders can often be determined by noting posture.
− Assess:
• Sternoclavicular joint
• Acromioclavicular joint
• Subacromial area
• Bicipital groove
Musculoskeletal System
• Assess range of motion:
− Ask patient to raise arms above the head.
− Have patient demonstrate external rotation and abduction.
− Perform internal rotation.
Musculoskeletal System
• Inspect elbows.
− Palpate between the epicondyles and olecranon.
− Range of motion:
• Flex and extend passively and actively.
• Pronate the forearms while the elbows are flexed.
Musculoskeletal System
• Inspect hands and wrists.
− Palpate the hands.
− Palpate the carpal bones.
− Range of motion:
• Make fists, then extend fingers
• Flex/extend wrists
• Move hands laterally and medially
Musculoskeletal System
• Inspect knees and hips.
− Range of motion:
• Ask patient to bend each knee and raise toward chest.
• Assess for rotation and abduction of hips.
− Palpate each hip.
− Palpate pelvis.
Musculoskeletal System
• Observe ankles and feet.
− Palpate feet and ankles.
− Assess range of motion:
• Have patient plantar flex, dorsiflex, and invert and evert ankles and feet.
• Inspect, palpate, and check forefoot and toes.
Peripheral Vascular System
• Comprises aspects of circulatory system
− Lymphatic system: network of nodes and ducts dispersed throughout the body
− Lymph nodes: larger accumulations of lymphatic tissues
Peripheral Vascular System
• Perfusion occurs in the peripheral circulation.
− Diseases of the peripheral vascular system are often seen in patients with other underlying medical conditions.
Peripheral Vascular System
• During assessment, pay attention to upper and lower extremities.
− Signs of acute or chronic vascular problems
− Refer to Skill Drill 13-13 .
Peripheral Vascular System
• Assessment
− Inspect upper extremities.
− Five P s of acute arterial insufficiency:
• Pain
• Pallor
• Parasthesias/Paresis
• Poikilothermia
• Pulselessness
Peripheral Vascular System
• Assessment (cont ’ d)
− Palpate epitrochlear and axillary lymph nodes.
− Inspect lower extremities.
− Palpate lower extremities.
− Note temperature of feet and legs.
− Attempt to palpate edema.
− Palpate superficial inguinal lymph nodes.
Spine
• Consists of 33 individual vertebrae
• Anchoring point for the skull, shoulders, ribs, and pelvis
• Protects the spinal cord
• Inspect the back.
− Lordosis
− Kyphosis
− Scoliosis
Spine
Spine
© Wellcome Trust Library/National Medical Slide
Bank/Custom Medical Stock Photo
© Dr. P. Marazzi/Photo Researchers, Inc.
© Southern Illinois University/Photo Researchers,
Inc.GA5323
Spine
• Palpate the spine.
• Check back for any other findings.
− Tap over costovertebral angles.
− Palpate scapulae, paraspinal areas, and base of neck.
− Check the buttocks.
Spine
• Range of motion:
− Check passively first, then actively.
• See Skill Drill 13-14 .
Nervous System
• Central nervous system: brain and spinal cord
• Peripheral nervous system: remaining motor and sensory nerves
Nervous System
• Brain comprises cerebrum, cerebellum, and medulla
• Except for cranial nerves, nerves are channeled to the brain via the spinal cord.
− Motor nerves control motion or movement.
− Sensory nerves send external signals to the brain.
Nervous System
• Cranial nerves go directly to and from the brain.
Nervous System
• Voluntary nervous system
• Involuntary (autonomic) nervous system
− Sympathetic
− Parasympathetic
− Reflexes
− Primitive reflexes
Nervous System
• Neurologic exam
− Mental status (AVPU)
− Cranial nerve function
− Distal motor function
− Distal sensory function
− Deep tendon reflexes
• Mental status exam
(COASTMAP)
− Consciousness
− Orientation
− Activity
− Speech
− Thought
− Memory
− Affect (mood)
− Perception
Nervous System
• Glasgow Coma Scale may also be used to assess people with alterations in mental status.
• See Skill Drill 13-15 .
Nervous System
• Cranial nerve examination
− Determines presence and degree of disability
− Can be performed in less than 3 minutes
Nervous System
• Evaluation of the motor system
− Posture and body position
− Involuntary movements
− Muscle strength
− Coordination
− Proprioception
Nervous System
• Check sensory function.
− Assess primary and cortical sensory functions.
− Evaluate deep tendon reflexes.
• See Skill Drill 13-16 .
Nervous System
• Results of the neurologic exam
− Delirium
• Consistent with an acute sudden change in mental status
− Dementia
• Representative of deterioration of cognitive cortical functions
Secondary Assessment of
Unresponsive Patients
• After ruling out trauma, position in recovery position.
− If trauma, position in neutral alignment
• Perform a thorough assessment of the body and look for signs of illness.
Secondary Assessment of
Unresponsive Patients
• Perform at least two sets of vital signs.
− Should include:
• Auscultated blood pressure
• Accurate pulse and respiratory rates
• Patient ’ s temperature
• Consider unresponsive patients to be in unstable condition.
Secondary Assessment of
Trauma Patients
• Two classifications of trauma patients:
− Isolated injury
− Multisystem trauma
• “ High visibility factor ”
− Do not become distracted by obvious but nonlife-threatening injuries.
Secondary Assessment of
Trauma Patients
• Patient who is unresponsive or has altered mentation is considered high risk.
• Perform rapid exam.
− When time and condition permit, perform physical examination.
Secondary Assessment of
Infants and Children
• Attempt to elicit information from the patient before parents.
• Obtain permission of a parent before examining if possible.
• Examine from toe to head.
Secondary Assessment of
Infants and Children
• When examining a newborn or neonate, be aware of normal variants:
− Vernix
− Edema
− Mongolian spots
− Jaundice
− Asymmetry of the head
Secondary Assessment of
Infants and Children
• Provide support of the head and neck.
• Examine eyes for irregularities.
• Inspect the umbilical cord.
• Children are prone to dehydration and infection.
Secondary Assessment of
Infants and Children
• Ages 1 to 3 years
− Will object to being touched or manipulated
− Use toe-to-head approach.
• Ages 4 to 5 years
− Usually cooperative and helpful
• School-age
− Be sure to explain what you are doing.
• Adolescents
− Concerned with bodily integrity
Secondary Assessment of
Infants and Children
• General principles:
− Remain calm.
− Be patient, gentle, and honest.
− Attempt to keep children with their parents.
− Do not neglect a child ’ s pain.
Secondary Assessment of
Infants and Children
• Exam techniques can vary slightly:
− Auscultation of a quiet infant ’ s abdomen is simple.
− Active tinkling bowel sounds may be heard.
− A more tympanic sound might be heard on percussion of an infant ’ s abdomen.
− Palpation techniques will vary with age.
Recording Secondary
Assessment Findings
• Should be orderly and concise
• Document using the forms recommended by your medical director.
− Note:
• Objective signs
• Pertinent negatives
• Similar relevant information
Limits of the Secondary
Assessment
• Evaluation by a trained physician, laboratory testing, and radiographic studies may be needed for a definitive diagnosis.
Monitoring Devices
• Continuous ECG monitoring
− Purpose is to establish a baseline
− Electrodes must be placed properly.
• The leads are usually colored and labeled to help with placement.
Monitoring Devices
• Continuous ECG monitoring (cont ’ d)
− Bipolar leads consist of two electrodes.
• Placed on different limbs
• Einthoven triangle
Monitoring Devices
• 12-lead ECG monitoring
− Patient should be supine.
− Prepare the skin.
− Connect electrodes.
− Connect and apply the precordial leads.
− Record the ECG.
Monitoring Devices
• Carbon dioxide monitoring
− Capnometry
• Measures carbon dioxide output
− Capnography
• Measures carbon dioxide output and provides a waveform
Monitoring Devices
Courtesy of Physio-Control, Inc.
Courtesy of Physio-Control, Inc.
Monitoring Devices
• Blood glucometer
− Can obtain reading in two ways in the field:
• From the hub of an IV catheter
• From a finger stick
− Most take only a few seconds.
− Should be calibrated regularly
Monitoring Devices
• Cardiac biomarkers
− Used to assess presence of damage to cardiac muscle
− May take several hours following a myocardial infarction for the cardiac biomarkers to become elevated
Monitoring Devices
• Other blood tests
− Basic and complete metabolic profile (CHEM 7 and CHEM 12)
− Brain natriuretic peptide (BNP) test
− Arterial blood gases
Reassessment
• Stable patients should be reassessed every
15 minutes.
• Unstable patients should be reassessed every 5 minutes.
Reassessment of Mental
Status and the ABCs
• Compare LOC with baseline assessment.
• Review the airway.
• Reassess breathing, circulation, pulse
Reassessment of Mental
Status and the ABCs
• Response of pediatric and geriatric patients may differ.
− Children decompensate very quickly.
− Geriatric patients may not show signs of deterioration.
Reassessment of Patient Care and Transport Priorities
• Have you addressed all life threats?
• Do priorities need to be revised?
• Is initial transport decision appropriate?
• Obtain another complete set of vital signs and compare with expected outcomes.
− Priority patients: minimum three sets
Reassessment of Patient Care and Transport Priorities
• Look for trends.
• Revisit patient complaints.
• Document all of your findings.
Summary
• Patient assessment is the most important skill a paramedic has.
• Patient assessment has five components:
− Scene size-up
− Primary assessment
− History taking
− Secondary assessment
− Reassessment
Summary
• The first step of the patient assessment process is the scene size-up.
• During the size-up, you also make a determination of the mechanism of injury or nature of the patient ’ s illness.
• Another important step in protecting yourself is to take standard precautions.
Summary
• The first step in the primary assessment is to form a general impression of the patient ’ s condition.
• During the primary assessment, you should be able to identify threats to the ABCs; these life threats should be addressed immediately.
Summary
• After assessing the patient for disability, you must make a transport decision and, if the patient has sustained trauma, perform a rapid exam.
• Once the primary assessment is complete and all life threats have been addressed, you can move into the history-taking phase of patient assessment.
Summary
• Patient history is a primary means of diagnosing the chief complaint in the field.
• The first part of a patient ’ s history also serves as a good mental status examination: ask for the patient ’ s name; the date, time, and location; the chief complaint; and the events leading up to the request for EMS assistance.
Summary
• After clarifying the history of the present illness, ask the patient about his or her past medical history, the state of his or her health, and any pertinent family history.
• For responsive patients, the history may generally be obtained directly from the patient; for unresponsive medical patients and trauma patients, it may be necessary to obtain the history from family.
Summary
• Use constructive communications skills as you talk with patients.
• At times you will need to ask patients about sensitive topics. Be familiar with techniques for successfully asking patients about these topics.
• Obtaining a history from a geriatric patient may involve challenges.
Summary
• Work on strategies within your service and with your partner for positive communications with patients.
• Secondary assessment is the process by which quantifiable, objective information is obtained from a patient about his or her overall state of health.
Summary
• There are times when you may not have time to perform a secondary assessment.
The two types of physical examinations are the full-body exam and the focused assessment.
Summary
• The secondary assessment includes obtaining vital signs and performing a headto-toe survey.
• The techniques of inspection, palpation, percussion, and auscultation allow you to use your physical senses to obtain physical information and to understand the normal functions of a patient ’ s body.
Summary
• Vital signs consist of a measurement of blood pressure; pulse rate, rhythm, and quality; respiratory rate, rhythm, and quality; temperature; and pulse oximetry.
• Monitoring devices used by the paramedic include continuous ECG monitoring, 12-lead
ECG, carbon dioxide monitoring, blood chemistry analyses, and cardiac biomarkers, among others.
Summary
• You need to alter your approach to patient assessment when dealing with infants and children.
• After the primary assessment, the reassessment is the single most important assessment process you will perform.
Summary
• The reassessment is performed on all patients. It gives you an opportunity to reevaluate the chief complaint and to reassess interventions to ensure that they are still effective.
• A patient in stable condition should be reassessed every 15 minutes, whereas a patient in unstable condition should be reassessed every 5 minutes.
Credits
• Chapter opener : Courtesy of Rhonda Beck
• Backgrounds : Green —Jones & Bartlett Learning;
Purple —Jones & Bartlett Learning. Courtesy of
MIEMSS; Blue —Courtesy of Rhonda Beck; Red—
© Margo Harrison/ShutterStock, Inc.
• Unless otherwise indicated, all photographs and illustrations are under copyright of Jones & Bartlett
Learning, courtesy of Maryland Institute for
Emergency Medical Services Systems, or have been provided by the American Academy of
Orthopaedic Surgeons.