Chronic Pain and CBT
advertisement

Chronic Pain Management with
Cognitive Behavioral Therapy
Definition of Chronic Pain
Chronic pain is often defined as
any pain lasting more than 12 weeks.
Whereas acute pain is a normal sensation
that alerts us to possible injury, chronic
pain is very different. Chronic
pain persists—often for months or even
longer.
Statistics
As of 2012, about half of all adults—117 million people—have one or more chronic health
conditions. One of four adults has two or more chronic health conditions.
Arthritis is the most common cause of disability (27%). In the United States each year 600,000 ppl
develop pain from arthritis for the first time
Other debilitating painful conditions are osteoporosis (21%), diabetes (17%), COPD and allied
conditions (15%), cancer (11%), and stroke (11%). More than 22 million say it causes them to have
trouble with their usual activities.
Low back pain disables approximately 7 million people and accounts for 8 million doctors visits
According to the American Pain Foundation, about 32 million people in the U.S. report having pain
lasting longer than one year.
From one-quarter to more than half of the population that complains of pain to their doctors are
depressed.
On average, 65% of depressed people also complain of pain
Pain Study
Percent of adults age 20 years and over
reporting pain lasting 24 hours or more in
the month prior to interview: Total 25.8%, Men
24.4%, Women 27.1%
(NHANES 1999-2002)
Duration of pain among adults reporting
pain in the month prior to interview: Less
than 1 month 32.0%, 1 month to less than 3 months
12.3%, 3 months to less than 1 year 13.7%, more
than 1 year 42.0%
(NHANES 1999-2002)
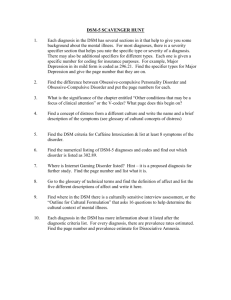
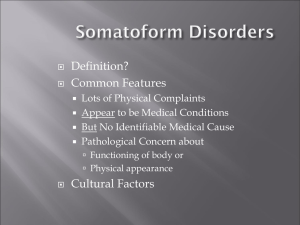
Diagnostic Criteria
Pain disorder is now classified as Somatic symptom
disorder (SSD) in DSM V. SSD is characterized by
somatic symptoms that are either very distressing
or result in significant disruption of functioning, as
well as excessive and disproportionate thoughts,
feelings and behaviors regarding those symptoms. To
be diagnosed with SSD, the individual must be
persistently symptomatic (typically at least for 6
months).
Changes from DSM IV to DSM V
Several important changes have been made from previous
editions of DSM. The DSM-IV disorders of somatization
disorder, hypochondriasis, pain disorder, and undifferentiated
somatoform disorder have been removed, and many, but not
all, of the individuals diagnosed with one of these disorders
could now be diagnosed with SSD.
Another key change in the DSM-5 criteria is that while
medically unexplained symptoms were a key feature in the
DSM IV it is not a key feature in an SSD diagnosis; symptoms
may or may not be associated with another medical
condition.
Reason for Changes in the DSM V
Overlapping previous diagnoses
Difficult for non
psychiatric physicians to apply
Reduction of stigma
Potential for mind body dualism
Implication that symptoms were not
“real”
Pain and Psychological Factors
DSM-5 looks at pain and psychological factors
conjointly . Based on research psychological
factor influence all forms of pain. Most
individuals with chronic pain attribute their
pain to a combination of factors, including
somatic, psychological, and environmental
influences.
Pain Cycle
Accept the reality of the pain for the
patient
When a patient presents pain
it is important that the
therapist or healthcare
professional accepts the
reality of the patient. Any
attempt to determine
whether pain is in excess of
what might be expected may
negate psychosocial factors
that influence the clinical pain
experience.
It is very tempting but dangerous to resort to concepts such as
“exaggerated pain” or “psychogenic pain” in patients which does
not correlate between their pain reports and the physical
findings.
Educate
Elicit how patients feel about their pain. What is their
knowledge and attitude about pain and its treatment.
Provide psychoeducation
◦ The physiology of pain: Pain results from a signal sent from
nerves to your brain. It can serve as an alarm, a warning -- that
you're stepping on a nail or touching a hot stove. But sometimes
the signals keep firing, and the pain continues. That’s when it
becomes chronic.
◦ Medical contradiction ( know what leads to increased harm not
just increased pain {talk to family doctor}) pain response and
signals aren’t always a sign of danger
Assess
Identify history and nature of persistent pain
◦ Frequency, intensity, duration, location
◦ Pain intensity scale
Identify the impact of pain on daily life
◦ Pain diary
◦ Pain assessment checklist
Compile a list of all medical dx, treatments, meds,
doctors
Assessing Problems and Concerns
Problem lists. These are a common and
useful strategy for identifying the
psychological, social, occupational, and
financial difficulties faced by patients.
Therapists who used problem lists typically
elicit a list of five to 10 difficulties from the
patient during the first part of session 1.
Problems are best identified using openended questions
Define the Problem
Problem
Frequency
Severity
Impact
Socially
Isolated
Stay at home
out of 7 days
Limited social contacts;
moderate-to-severe
isolation
Highly distressing; socially
debilitating; estranged
family/friends
Pain
Experience
pain each hour
Pain intensity is
when present
Pain leading to decreased
activity level, inability to
work
Feelings of
Worthlessness
Occur
days
3 out of 7
Very intense when
present;
sometimes involves
suicidal
Thoughts
Highly distressing;
work, social, and
relationships
influences
intimate
Fatigue
Occurs almost
Constantly
Fatigue not intense but
troublesome
Decreased activity level,
frequent naps, inability to
complete daily tasks
Devise Long Term Goals
Experience decreased feelings of intensity and/or
duration of pain episodes
Obtain needed skills to better manage pain
Better cope with pain to increase ability to
complete daily tasks and engage in social activities
Find a new sense of empowerment in ability to
manage pain
Devise Short Term Objectives
Identify and monitor particular pain
triggers
Learn and implement somatic skills
Identify negative pain related thoughts and
replace them with positive coping related
thoughts
Increase level and range of activity by
identifying and engaging in activities
Pain Triggers
Identify pain triggers by teaching the patient to
self-monitor their symptoms
Pain Diary thoughts, feelings, behaviors, people,
situations helps the client to identify how pain
impacts his/her daily activities social and leisure
involvement
Process the journal with the patient to increase
insight into the nature of the pain, cognition,
behavioral triggers, and the positive or negative
effect of the interventions they are currently
using
Germany – Patient ID15
Pain diary - experiences
Tell us how you were feeling at the beginning,
during and at the end of the day
When I woke up I felt…
During the course of the day I felt…
What impact did your pain have on you
today?
Impact on daily activities
Impact on your mood
Impact on your
relationship with others
In the evening I felt…
Somatic Skills
Teach relaxation techniques as a useful and quick
response to high stress or pain levels. This allows
patients in many circumstances to reduce stress
and pain and thus cope in an adaptive manner
with these unpleasant states.
Quantifying pain on a 5 point scale before and
after the relaxed state is a useful aid towards
showing its effectiveness, where 0 is no pain and 5
is excruciating pain.
Patients are encouraged to keep pain diaries
while on the course
Negative Pain Related Thoughts
Catastrophizing/Awfulizing – predicting the
worst case scenario.
Black and white thinking – forgetting that reality
is composed of many shades of gray.
Unrealistic expectations for the world - (should
statements).
Mind reading – believing we know what others are
thinking about us.
Emotional reasoning - believing our feelings
indicate truth. Believing that if we feel worried about
our pain that means our pain is causing harm.
Altered Mood
Fear of Injury
Anger
Physical
Deconditioning
Fatigue
Anxiety
Confused Thinking
Increase Activity Levels
PACING: Scheduling activities throughout a
period of time to ration energy (energy
conservation)
ENERGY CONSERVATION: Doing no more
on a good day, no less on a bad day and
therefore reducing the learning relationship
between pain and activity (time contingent
activity)
ACTIVITY PLANNING: Planning activity to
ensure a balance of pleasurable and less
pleasurable tasks
Activity: Working to Quota
Working to Quota is used to disrupt the learned relationship between
activity and pain levels, an opportunity to (1) reduce inadvertent
learned associations and (2) begin to use skills to help confront fear
of pain and take control can begin.
Establish a hierarchy of activities from least concerning to most
concerning. Identify exactly what the concerns are – do they need
to be addressed with information, or do they need to learn from
experiencing (testing) what happens if
Establish your baseline, and develop a ‘timetable’ for a week (or any
period of time) in collaboration with the person.
Review and reset the activity schedule – maintain or increase
activity level at this time
Relapse Prevention
Discuss the distinction between a lapse and
relapse, associating a lapse with a return of
pain or old habits (e.g. having a bad day) vs
relapse with a persistent return of pain and
previous behavioral habits and cognitions
Identify and rehearse the management of
future situations or circumstance in which
lapse could occur using the learned
strategies for self management
Quiz
In DSM IV –TR a patient with high levels of anxiety about having a disease and many associated somatic symptoms would be
given the diagnosis of hydrochondriasis. What DSM V diagnosis would apply to the patient?
◦
General anxiety disorder
◦
Somatoform disorder nos
◦
Somatic symptom disorder
What is the leading cause of debility in the United States
◦
COPD
◦
Stroke
◦
Arthritis
What do experiences such as keeping a pain diary reveal about a patient?
◦
Identifies pain triggers
◦
Shows avoidance areas
◦
Reveals the impact pain has at rested periods of the day
Which of the following has been removed from the DSM- IV?
◦
Hypochondrias
◦
Social Anxiety Disorder
◦
Nasopharyngitis
How does working to quota help disrupt the learned relationship between activity and pain
⁻
It shows how to reduce activities
⁻
Helps develop skills to confront and control pain
⁻
Gauges how to manage medication regimen
References
psychological factors affecting other medical conditions dsm 5
http://www.ucdmc.ucdavis.edu/psychiatry/calendar/DSM5_presentation_20130816.pdf
Assessment of the Patient With Pain www.medscape.com"lacks specificity" and could cause the
mislabelling of a sizeable proportion of the public as mentally ill./viewarticle/78 DSM-5 Somatic
Symptom Disorder Debate Rages On
http://www.health.am/psy/more/assessment_of_the_patient_with_pain/
Cognitive Behavioral Therapy for Managing Pain
http://www.apa.org/divisions/div12/rev_est/cbt_pain.html
Cognitive behavioral therapy for back pain
http://www.nlm.nih.gov/medlineplus/ency/patientinstructions/000415.htm
Managing Chronic Pain: A Cognitive-Behavioral Therapy Approach Workbook (Treatments That
Work) John Otis
Managing Chronic Pain 10 min CBT strategies http://www.youtube.com/watch?v=tiuZBndewbE
Cognitive Behavioural Therapy for Treatment of
Painhttp://www.youtube.com/watch?v=v6yLIqdLvNk