HEMATOLOGY
advertisement

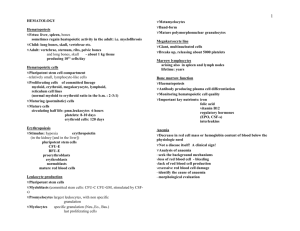
HEMATOLOGY Hematopoiesis Fetus: liver, spleen, bones sometimes regain heatopoietic activity in the adult: i.e. myelofibrosis Child: long bones, skull, vertebrae etc. Adult: vertebrae, sternum, ribs, pelvic bones and long bones, skull - about 1 kg tissue producing 1011 cells/day Hematopoietic cells Pluripotent stem cell compartment – relatively small, lymphocyte-like cells Proliferating cells of committed lineage myeloid, erythroid, megakaryocyte, lymphoid, reticulum cell lines Maturing (postmitotic) cells Mature cells circulating half life: pmn.leukocytes 6 hours platelets: 8-10 days erythroid cells: 120 days Erythropoiesis Stimulus: hypoxia erythropoietin (in the kidney [and liver]) pluripotent stem cells CFU-E BFU-E proerythroblasts erythroblasts normoblasts mature red blood cells Leukocyte production Pluripotent stem cells Myeloblasts Promyelocytes Myelocytes Leukocyte production Metamyelocyte Leukocyte production Band-form Leukocyte production Mature polymorphonuclear granulocyte Megakaryocyte line Giant, multinucleated cells Breaks up, releasing about 5000 platelets Marrow lymphocytes arising also in spleen and lymph nodes lifetime: years Bone marrow function Hematopoiesis Antibody producing plasma cell differentiation Monitoring hematopoietic cell quality Important key nutrients: iron folic acid vitamin B12 regulatory hormones (EPO, CSF-s) interleukins Hematological diseases Anemia Decrease in red cell mass or hemoglobin content of blood below the physiologic need Not a disease itself! A clinical sign! Analysis of anaemia – seek the background mechanisms loss of red blood cell - bleeding lack of red blood cell production excessive red blood cell damage History Family history: anemia, splenomegaly, jaundice Bleeding tendency in the family Diet, alcohol intake Menorrhagia Drugs Chronic diseases Malnutrition, malabsorption Transfusion, iron or other therapy against anemia Anemia Signs and symptoms vary with the rapidity of onset: Rapid (bleeding or brisk hemolysis) cardiovascular compensatory reactions: tachycardia, postural hypotension, vasoconstriction in the skin and extremities, dyspnea on exertion, faintness, even shock Slowly developing anemias (ie.nutritional deficiency, chr.bleeding, hemolysis etc.) – there is time for compensation – the patient remains asymptomatic for a long time – Anemia Mild: often asymptomatic Moderate: symptoms on exertion Severe: symptoms on rest heart failure Anemia - physical findings Non cause-specific Pallor of skin and mucous membranes – – causes: Hb and blood redistribution from the skin colors greyish: malignancy lemon-like: hemolysis, B12 deficiency Tachycardia Hyperkinetic precordium Systolic murmur (reversible) Anemia - physical findings Cause-related Jaundice hemolysis Hepatosplenomegaly - e.g.hemolysis Lymphadenopathy - lymphomas, autoimmune diseases Cheilosis (fissura) iron deficiency Koilonychia (spoon-shaped nails) iron def. Beefy red smooth tongue (Hunterglossitis) - pernicious anemia Neuropathy - pernicious anemia Rectal digital examination - bleeding Laboratory evaluation of anemia Complete blood picture Red cell indices red blood cell count F:3,9-5,6, M:4,5-6,5 G/l hemoglobin level F:115-155 M:135-175 g/l hematocrit F:36-48 M:40-52% MCV: mean corpuscular volume 80-95 fl MCH mean corpuscular hemoglobin 27-34 pg MCHC: mean corpuscular hemoglobin concentration 300-350 g/l Reticulocyte count (traces of endoplasmic reticulum) - good marker of erythropoiesis 0,5-1,5% MCV Microcytic anemia (MCV<80 fl) iron deficiency, thalassemia, sideroblastic anemia Normocytic anemia (MCV 80-100 fl) acute bleeding, renal failure, aplastic anemia Macrocytic anemia (MCV>100 fl) vitamin B12, folic acid deficiency, liver disease, alcoholism, hypothyroidism MCH Hypochromic (MCH<27 pg) – – Normochromic (MCH 27-34 pg) – Iron deficiency(i.e. chr. bleeding, malabsorption) chr. inflammation, malignancy, chr. infection, thalassemias, myelodysplastic sy. acute bleeding, hemolysis, aplastic anemia, renal anemia Hyperchromic (MCH>34 pg) – megaloblastic anemia (B12, folic acid deficiency) Clinical classification of anemias Decreased cell production – – – – – Aplastic anemia Myelodysplastic syndrome Deficiency anemias (iron, B12, folic acid) Erythropoietin deficiency (renal failure) Bone marrow suppression (malignancy, toxin,virus) Increased red blood cell destruction/elimination Extrinsic factors (immun, toxins, mechanic) – Membrane defects – Enzyme defects – Hemoglobinopathy Blood loss (genitourinary, gastrointestinal, pulmonary other bleeding) – Bone marrow investigation Bone marrow biopsy or aspiration bone marrow cellularity myeloid-erythroid ratio (norm: 2-3:1) cell maturation bone marrow infiltration stromal cells (fibroblasts etc.) Polycythemias Hyperviscosity – – – Increased cell turnover – – Decreased cerebral blood flow tinnitus, lightheadedness, dizziness, stroke Congestive heart failure Thrombosis Gout (due to hyperuricemia) Itching In polycythemia vera – – Thrombocytosis Hemorrhage Polycythemias Primary: polycythemia vera myeloproliferative disorder – – – other cell lines are affected (leukocytosis, thrombocytosis) hepatosplenomegaly EPO level: low Secondary: – hypoxia EPO production chr. pulmonary diseases morbid obesitiy (Pickwick’s syndrome) high altitude – EPO overproduction: tumors Leukocyte disorders 1. Benign alterations 2. Malignant diseases Neutrophil granulocytes Functions: chemotaxis phagocytosis microbial killing Disorders neutropenia, agranulocytosis: abs.count<1000 causes:drugs, autoimmun diseases, viral infections (e.g. EBV,HIV,hepatitis), B12 deficiency, leukemias,alcoholism increased risk of infection neutrophilia:infections, left stress, drugs (steroids) shift: bacterial infections Mononuclear phagocytes monoblasts, promonocytes, monocytes, tissue macrophages Functions chemotaxis ingestion and killing microorganisms secretion of several factors proteases, cytokines, reactive oxygen compounds, colony stimulating factors interaction with lymphocytes antigen processing and presentation Eosinophil granulocytes Eosinophilia: Parasitic infections Allergies Autoimmune diseases Hematologic malignancies (CML, Hodgkin’s disease etc.) Basophil granulocytes Important role in: – – inflammation hypersensitivity reactions Basophilia: malignant hematologic diseases Acute leukemias Agressive immature hemopoietic cell proliferation, without differentiation – (hiatus leucemicus in the blood smear) Subtypes: ALL (acute lymphoblastic leukemia) ANLL (acute non lymphoblastic leukemia) or AML (acute myeloblastic leukemia) Acute leukemia syndrome Susceptibility to infections - serious infections Anemia due to bone marrow infiltration and bleeding Thrombocytopenia - bleeding tendency purpuras, petechiae, mucosal bleeding Organ infiltration Chronic leukemias Uncontrolled expansion of premature hemopoietic cells which are able to differentiate Subtypes: – – Chronic myelogenous leukemia (CML or CGL) a myeloproliferative disorder Chronic lymphocytic leukemia (CLL) a malignant lymphoma CML Abnormal blood count Organomegaly (hepato)splenomegaly CLL Old patients Blood count abnormalities Leukocytosis Lymphocytosis (small, mature lymphocytes) In advanced disease: anemia, tct-penia Generalised lymphadenopathy Splenomegaly Susceptibility for infections (pneumonia) Sometimes hemolytic anemia Immundeficiency Evaluation of leukemias Complete blood picture Bone marrow investigation Cytochemistry Immunochemistry Genetic alterations chromosomal aberrations gene anomalies Chronic myeloproliferative disorders Polycythemia vera Myelofibrosis with myeloid metaplasia Essential thrombocythemia Chronic myelogenous leukemia Diseases of the lymphoid system Normal lymph nodes – – – – Non palpable or <1 cm, except in the inguinal region where can be 0,5-2 cm sized lymph nodes normally Small lymph nodes can be remain after infection Significant: one or more new nodes >1 cm (which can’t explain by a previously recognised cause) New lymph nodes in older age more significant children more likely respond with lymphoid hyperplasia lymphyadenopathy under 30 years: 80% benign over 50 years: 40% benign Causes of lymphadenopathy – – – – – (1) increase in the number of benign lymphocytes and macrophages during response to antigens (2) infiltration by inflammatory cells in infections (lymphadenitis) (3) in situ proliferation of malignant lymphocytes or macrophages (4) infiltration of nodes by metastatic malignant cells (5) infiltration of lymph nodes by metabolite-laden macrophages in lipid storage diseases Lymph node characteristics Location Number (single, multiple, matted together) Size Tenderness Consistency (hard, rubbery, soft) Mobility Skin reactions above the lymph node Lymphadenopathy- by region – – – – – – – Cervical in young adult: infectious mononucleosis Unilateral epitrochlear : hand infections Bilateral epitrochlear : sarcoidosis, tularemia, syphilis Unilateral axillary: breast carcinoma, lymphomas, infections of the upper extremities, cat-scratch disease, brucellosis Bilateral inguinal: venereal infections Unilateral inguinal: lymphogranuloma venereum, syphilis Progressive inguinal lymph node enlargement without obvious infection: malignant disease. Lymphadenopathy- by region – – – – – – Posterior cervical, occipital: scalp infections, toxoplasmosis, rubella Anterior auricular: infections of the eyelids and conjunctiva Lymphomas often involve cervical lymph nodes and occasionally involve posterior auricular and occipital nodes Enlarged suppurative cervical nodes: mycobacterial lymphadenitis (scrofula) Unilateral jugular or mandibular lymph node: lymphoma or head and neck malignancy Supraclavicular (always significant): metastasis from intrathoracic, breast, gastrointestinal malignancies (Virchow’s lymph node) or lymphoma Lymphadenopathy- by region Hilar or mediastinal – – – – Symptoms: cough,wheezing, hoarseness, paralysis of the diaphragm, dysphagia Bilateral mediastinal: lymphomas Unilateral hilar: metastatic carcinoma (usually lung) Bilateral hilar: sarcoidosis, tuberculosis, fungal infections, lymphomas Retroperitoneal, intraabdominal: lymphomas, metastases, rarely inflammatory (Tuberculosis can cause mesenteric lymphadenitis with large matted and sometimes calcified nodes) Generalised: lymphomas (CLL), systemic infections (tbc), autoimmune diseases Lymphadenomegaly Diagnostic evaluation Complete blood picture Chest x-ray Ultrasonography (abdominal, cervical, axillar etc.) CT-scan Fine needle biopsy- cytology Lymph node excision Splenomegaly - causes – (1) Reticuloendothelial or immune system hyperplasia infectious diseases immune diseases (Felty's syndrome - RA) abnormal red blood cell destruction: hereditary spherocytosis, thalassemia, sickle cell disease – – (2) Altered splenic blood flow (congestion): hepatic cirrhosis, splenic, hepatic, or portal vein thrombosis (3) Malignant neoplasms: primarily: lymphomas secondarily: leukemias, metastatic solid Splenomegaly – – – (4) Extramedullary hematopoiesis in the spleen: myeloid metaplasia (5) Infiltration of the spleen with abnormal material: amyloidosis, Gaucher's disease (6) Space-occupying lesions of the spleen: hemangiomas, cysts Splenomegaly – – – Mild: congestive heart failure, malaria, typhoid fever, bacterial endocarditis, systemic lupus erythematosus, rheumatoid arthritis, thalassemia minor Moderate: hepatitis, cirrhosis, lymphomas, infectious mononucleosis, hemolytic anemias, splenic abscesses and infarcts, amyloidosis Massive: chronic myelocytic leukemia, myeloid metaplasia with myelofibrosis, hairy cell leukemia, Gaucher's and Niemann-Pick diseases, sarcoidosis, thalassemia major, chronic malaria, congenital syphilis, leishmaniasis, portal vein obstruction Splenomegaly Diagnostic evaluation Complete blood picture Serology (infections, autoantibodies) Blood culture Imaging technics (chest x-ray, ultrasonography, Doppler US, CT, MR) Histology Malignant lymphomas Arise in lymph nodes or extranodal lymphoid tissue Subtypes: – – Hodgkin’s disease Non Hodgkin’s lymphomas Hodgkin’s disease Mostly young adults Asymptomatic lymphadenopathy – – – often cervical mediastinal abdominal Hepatomegaly, splenomegaly Fever, night sweats, loss of weight Diagnosis: lymph node histology (Reed-Sternberg cells) Staging Non Hodgkin’s lymphomas Older patients More diffuse lymph node involvement General symptoms:fever, weight loss, night sweat Frequent extralymphatic involvement (50%: bone marrowanemia, tct-penia) Special forms: CLL Skin infiltration (T-cells) MALT-lymphoma Multiple myeloma Multiple myeloma Plasma cell neoplasm Bone marrow infiltration Monoclonal immunglobulin production Osteolytic lesions, bone pain Renal lesion Coagulation disorders Bleeding tendency, thrombosis, embolism Factors platelets (number, function) coagulation factors (amount, function) surface of the blood vessels, circulation Bleeding - history History of common hemostatic stresses: gum extraction, minor surgeries menstruation, childbirth injuries Family history of bleeding tendency Bleeding Primary hemostatic defect (platelets) occurs immediately after trauma from superficial sites (skin, mucous membranes, nose, rarely from gastrointestinal, genitourinary tract) – – purpuras, petechiae ecchymoses bleeding time Secondary hemostatic defect (coagulation) delayed occurence (hours, days) from deep sites (joints, subcutaneous tissues, muscles, retroperitoneum, body cavities, cerebrum) – – hematomas hemarthroses coagulation time Bleeding - physical findings From capillaries: purpuras, petechiae small, superficial,dermal or mucosal pinpoint hemorrhages characteristic for platelet disorders From small arterioles and venules: – – – ecchymoses subcutaneous blood collections- bruises hematomas deeper, palpable in platelet and coagulation disorders Hemarthros - bleeding into joints characteristic for coagulation disorders (mostly hemophilia) leads to chronic joint deformity Thrombosis and embolism Virchow’s triad – – – Hypercoagulability Circulation disturbance- congestion Pathological endothelial surface http://medicine2.aok.pte.hu/download/ Hemato_Proped.ppt Hemato_Proped.doc