Is Herpes
advertisement

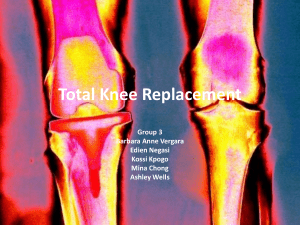
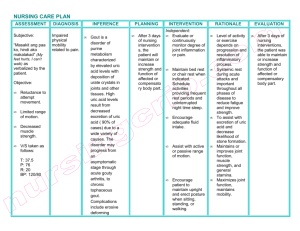
COMPREHENSIVE CLINICAL WRITEUP 1 Clinical Write-up: Comprehensive Health History II Advanced Health Assessment and Measurement Course Roshan Jan Muhammad The Johns Hopkins University School of Nursing “On my honor, I pledge that I have neither given or nor received any unauthorized assistance on this assignment”. RJM COMPREHENSIVE CLINICAL WRITEUP 2 Comprehensive Health History BIOGRAPHIC DATA Name: JR Date of Birth/Age: Dec 6th, 1928 Date of visit: 6th Nov, 2012 (1300) was in ER till 7th Nov History Number: One Gender: Male Birthplace: USA Social Security Number: 000-01-1111 Address: Baltimore Home phone: 410-002-9898 Employer: Retired Navy officer Religion: Christian Marital Status: Married Insurance (name and #): Medicare Primary Clinician: YR Date of Last Visit: One month ago SOURCE/RELIABILITY: Patient, who is reliable. CHIEF COMPLAINT: Patient is presented with the complaint of “knee pain”. HISTORY OF PRESENT ILLNESS: Patient arrived in ER at 1300, with the complaint of non-traumatic origin of throbbing pain in rt knee for 3 days. The intensity of pain gradually increased to 9/10 over 3 days, it radiates to the foot, is aggravated while weight bearing and flexion of the limb, and is associated with heavy feeling of the limb, swelling, and restricted motion of rt knee, took Tylenol 2 tablets twice a day for 3 days but did not significantly relieve the pain and is now seriously affecting his walking ability. Uses cane to walk. Had similar type of pain in Oct 2011 as well, which improved after colchanice. Denies joint stiffness, tingling, numbness, clumsiness, weakness, crepitation, bone deformity, cyanosis, pallor, hypothermia/hyperthermia, decreased sensation, ulceration, edema, calf tenderness, varicosities, and abnormal pigmentation. Pain at the time of assessment was 2/10 after administration of cap acetaminophen 650 mg, oxycodone 5 mg PO, and prednisolone 40 mg PO OD. Knee x-ray (Dec 6th, 2012) reveals joint effusion with anterior displacement of patella (ballotable). PAST MEDICAL HISTORY General health: According to patient he had a very healthy life upto age of 60 and despite current medical ailments he considers himself in a good state for his age. COMPREHENSIVE CLINICAL WRITEUP 3 Childhood illnesses: Patient had measles and pertussis in his childhood. Age and course of illness could not be recalled. (-) chickenpox, mumps, rheumatic fever, otitis media, sinusitis, tonsillitis, asthma, congenital conditions. Adult Medical illnesses and hospitalizations: Known case of HTN since 15 years, Gout (diagnosed in Oct 2011). Was hospitalized for coronary artery bypass grafting (CABG) in (1995). Prostat Ca was diagnosed in (1987), he was admitted then to receive radiation and Lupron, is in remission ever since, PSA and testicular exam done in April 2012 which is normal as per patient (official report not available). Patient had also been hospitalized for non-traumatic severe epistaxis x 1, dehydration x 2 , GI bleed x1, urinary tract infection x1, appendectomy. Data gap (year and course of treatment). Reports intermittent breathing problem for last 3 years with wheeze and dry cough but denies asthma, COPD or bronchitis (Refer respiratory system review of system for details). Denies diabetes, tuberculosis and hepatitis. Immunization: Childhood immunization status is not known. Had Influenza shot last week, pneumococcal pneumonia (2011), denies any reaction to the immunization. Had several vaccination during navy service but do not know the names. (-) Hep A & B, varicella, meningococcal meningitis, herpes zoster, cholera, typhus, typhoid. Psychiatric illnesses: (-) for depression, anxiety, attention/hyperactivity disorder, schizophrenia and suicide attempt, has never received any related emergent treatment or psychotherapy. Medications Patient is on following prescribed medications. Metoprolol, Norvasc, cozar for HTN, compliance is inconsistent. (data gap) year of start and dose. Aspirin 81 mg OD was started post CABG, takes it regularly. Protonix PRN. (Data gap) dose. Combivent (INH) and albuterol (INH) was prescribed 3 years back when he had acute breathing problem. He was prescribed to take it routinely, but he only takes in case of acute wheeze and breathing problem. (Data gap) dose. Procit shot once a week for anemia. Takes is regularly. Colchicine was started last year with onset of joint pain but he does not take it regularly. (Data gap) dose. Allergies: No known allergies to medications, chemicals, environmental factors and food. Transfusion: Received blood product during CABG, type of product not known. (-) transfusion reaction. Health maintenance screening: Hb (see lab results section), lipid profile, testicular exam and PSA done in April 2012; colonoscopy (2010); dental and ear exam (data gap, year); eye exam (2010). (Data gap) official results are not available. (-) HIV, Chlamydia, Syphilis, Gonorrhea, PPD. FAMILY HISTORY Mother had diabetes and his brother has HTH and had a stroke He does not know the cause of death of his parents and most of the family members. Family history (-) asthma; allergies; tuberculosis; hepatitis; kidney or respiratory diseases; blood dyscrasias; rheumatologic, or autoimmune illnesses; thyroid problem; cancer; addiction; violence. PERSONAL/SOCIAL HISTORY COMPREHENSIVE CLINICAL WRITEUP 4 Cultural and family constellation: Was born and raised in Baltimore. He is eldest among 4 siblings. Is married, has 2 sons and three daughters, all healthy and alive, live outside Baltimore. He lives with her wife in Baltimore. Reports satisfied relationship with her family. (Data gap) (hobbies, interest, proscriptions concerning medical care). Education and occupation: Worked in navy service for 30 years, is now retired for last 28 years. (-) exposure to infectious diseases and industrial toxins in recent years. Economic condition and Environment: He is financially dependent on his children and on Medicare benefit. Lives with his wife in his own house in Baltimore. House is equipped with smoke detectors and has fluoridated water source. Stress and Abuse: Reports that navy service was stressful but current abuse screen is negative. Does not report major stressors in life at present that is beyond his ability to manage. (Data gap) coping strategies. Travel history: Negative travel history in last 10 years. CURRENT HEALTH HABITS AND RISKS FACTORS Exercise/activity: Stays home most of the time, does not exercise but goes for a walk every day for 30-45 minutes accompanied by his friend or a wife, with an exception when he has acute joint pain. Cannot do brisk walk, uses cane and takes at least 1-2 breaks in between due to fatigue. Seldom develops shortness of breath that is relieved with 2 puffs of albuterol. Diet/nutrition: Negative eating disorder screening. Reports good appetite; and denies recent weight changes, use of supplementary pills and is not on restricted diet. (Data gap) dietary intake for last 24 to 48 hours and typical fluid consumption. Sleep: Easily falls into sleep and takes 6-7 hours and takes 1hour afternoon nap. Pain never interfered with sleeping until last 3 days. Substance Abuse: Occasionally drinks beer that is less than a glass with seafood only. Smoked cigarette for 40 years (1-2 packs per week), quit in 1987 after diagnosis of prostat cancer. (Data gap) coffee use. Safety measures: Uses cane and glasses. (Data gap) seatbelts, and other safety measures based on sensory impairment. Typical day: (Data gap) usual daily activities. REVIEW OF SYSTEMS (ROS) General constitutional symptoms: (-) fever, chills, malaise, fatigability (other than while daily walk), weakness or night sweats. Diet: Appetite good. (-) anorexia, hyporexia, hyperexia. Skin, hair and nails: Takes bath every 2 days and maintains good hygiene of hair and nails. (-) rash, itching, pigmentation, cyanosis, abnormal hair or nail growth or loss (other than age related) Head and neck: (-) headache, dizziness, syncope, head trauma, period of loss of consciousness. Eyes: Reports blurred vision bilateral (more in rt eyes) for 6 years to the extend that he cannot read or recognize features of individuals, uses glasses but is not helpful for lt eye in particular. (-) diplopia, photophobia, pain, discharge, floaters, strabismus, glaucoma, history of trauma or eye infection. Data gap (date and report of eye exam) COMPREHENSIVE CLINICAL WRITEUP 5 Ears: Reports slightly diminished hearing in both ears for 5years but does not use any hearing aids. (-) pain, discharge, vertigo, tinnitus. (Data gap) hearing test and results. Nose (-) sense of smell, frequency of colds, obstruction, congestion, epistaxis, post nasal discharge, sinus pain and snoring. Throat and mouth: wears removable upper and lower jaw dentures, cleans it daily. Denies frequent sore throat, hoarseness or change in voice; halitosis, bleeding or swelling of gums; soreness of tongue of buccal mucosa, ulcer, disturbance of taste. Endocrine: (-) thyroid enlargement or tenderness; heat or cold intolerance; unexplained weight change; lethargy; polydipsia or polyuria, changes in facial or body hair, increased glove size or skin striae. Chest and Lung: Reports sporadic onset of breathing difficulty that is usually provoked by exertion while walking and is associated with dry cough and wheezing and is relieved with albuterol inhaler (2 puffs) and rest.(-) pleurisy, hiccups, exposure to TB. Chest x-ray, PFT done few years back (report not available) Heart: (-) chest pain or distress, palpitations, orthopnea at rest or exertion. CABG details, ECG, ECHO, blood cholesterol and other lab report findings are not available. Peripheral vascular: Refer HPI. Hematologic: Reports to have low hemoglobin for a long time. Denies tendency to bruise or bleed easily, thromboses, thrombophlebitis. Lymph nodes: Denies palpable nodular swelling of glands at any part of the body. Gastrointestinal: Passes normal stool every 1-2 days. Reports infrequent sporadic heart burn that usually relieves with Protonix. Denies dysphagia, odynophagia, reflux, nausea, vomiting, hematemesis, melena, constipation, diarrhea, jaundice, dark urine, abdominal fullness, distension, swelling and pain. (Data gap) hemorrhoids. Colonoscopy report not available, no other GI related studies performed. Urinary: Denies dysuria, flanks or suprapubic pain, urgency, frequency, nocturia, hematuria, polyuria, hesitancy, dribbling, passage of stone, edema of face, incontinence, hernia. (Data gap) loss in force of stream. Male GU: Denies STI and pain in scrotum or testes. (Data gap) age @ puberty; sexual function/ sexual orientation; penis: circumcised; adhesions, lesions, ulcerations, discharge from penis; pain, edema, rashes, emissions; ejaculation painful/incapacity. Number of lifetime partners. Musculoskeletal: Refer HPI. Neurologic: Reports forgetfulness (senile). (-) syncope, seizures, weakness, paralysis, loss of sphincter control, abnormalities of sensation or coordination, tremors, behavior change. Psychiatric: Reports difficulty in concentrating. (-) mood changes, sadness, nervousness, tension, irritability, change in social interactions or personality, depression/mania, suicidal/homicidal thoughts. PHYSICIAL EXAMINATION Vital signs: Temperature 35.8C; Pulse 63/min; Respiration 18/min; Blood pressure trend in the ER was systolic blood pressure (206-180), diastolic blood pressure (81-69), last blood pressure in supine position 180/69 post hydralazine 50mg OD in ER; O2 saturation 98% on room air. Growth and measurement: (Data gap) Height, weight and BMI. However, inspection does not reveal truncal or abdominal obesity or muscle wasting. General survey: 84 years old African American male, lying comfortably on bed without any distress. COMPREHENSIVE CLINICAL WRITEUP 6 Skin: Skin is smooth, dry (particularly in lower limb), warm to touch, no signs of central or peripheral cyanosis, turgor normal. Onychogryphotic nails of lower extremities. Upper extremities have thick pale nails with irregular surface but no clubbing. (-) capillary refill, excessive perspiration. Head: Normocephalic head, facial expressions relaxed and symmetrical. Scalp clean; black and grey, hair with male pattern baldness. (-) edema or puffiness. Ears: Whisper negative in rt ear, could hear me ok otherwise in both ears. Ears normally aligned. (Data gap) weber and rinne’s test, assessment of ear cannal, tympanic membrane and other landmarks deferred because of nonfunctional otoscope at bedside. Eyes: Eye brows symmetrical, mild bilateral ptosis, conjunctiva pink and moist, sclera white, has bilateral senile arcus, extraoccular movement smooth in all direction except nystagmus during extreme lateral movement. Pupils rt 3.0 lt 4.0, round and reactive to light and accommodation, corneal reflex positive. (-) orbital edema, crusting, discharge from eyes. Peripheral vision loss both sides. (Data gap) visual acuity, visual field, cover uncover test. Fundoscopic and retinal examination deferred because of non functional opthalmoscope. Nose: Septum midline, no discharge or flaring, maxillary or frontal sinus tenderness, nostril patent. (Data gap) turbinate examination deferred because equipment at bed side not working. Mouth and throat: Tongue, gums, oral and buccal mucosa moist, clean and light pick in color. Posterior hard palate has painless, white, linear oral thrush measuring 1x 0.25 inches, rest of the palate was pale. Posterior pharynx light pink, tonsils grade 1 bilateral, uvula rises on phonation, tonsils grade I (-) erythema, petechiae, exudate. Neck: Neck supple, trachea centered, thyroid non-palpable, carotid artery +2 bilateral. Chest: Anterior posterior to transverse diameter is 1:2. Breathing regularly and comfortably at rate of 18 breaths/min without using accessory muscles. Thoracic expansion and tactile fremitus equal bilateral had resonance all over lung field. Breath sounds equal bilateral, bronchial sound over trachea, bronchovesicular sound between 2nd and 3rd ICS, vesicular sound on rest of the lung field, mild expiratory wheeze in rt lower lobe. (-) friction rub. (Data gap) diaphragmatic excursion. Voice sounds not indicated. Heart: Regular sinus rhythm (63/min); PMI, around 1 cm at 5th ICS mid clavicular line. No abnormal pulsation, thrills, heaves or lift. S1 and S2 heard in all precordial areas. S2 louder in aortic and pulmonic area, S1 louder in tricuspid and bicuspid area. No split sound, murmurs, clicks, snaps, S3 and S4 gallop heard. Blood vessels:. JVP 2cm at approximately 30 head of bed. Temporal, posterior tibial and dorsalis pedis (+1 bliteral), radial and brachial pulse (+2 bilateral), femoral (+2 bilateral). Grade I pitting edema on rt foot and swelling on rt knee. (-) venous distension or tenderness in lower extremities, bruit over temporal or carotid artery. (Data gap) popliteal pulse. Abdomen: Round, symmetrical abdomen, umbilicus centered, no abnormal pulsation, peristalsis or bulges. Gurgling bowel sounds +ve in all 4 quadrants no bruit over renal, iliac and femoral artery. Tympany heard over stomach, dullness on liver. Abdomen soft on palpation, spleen and kidneys non-palpable. Liver span 6 cm at mid clavicular line. (-) guarding, direct or indirect rebound tenderness. Femoral lymph nodes non-palpable, no CVA tenderness. Genitalia, anus and rectum: Examination deferred. Lymphatic: (-) lt femoral, inguinal, occipital, pre auricular, post auricular, superficial, anterior and posterior cervical, tonsillar, parotid, submental, submandibular, supraclavicular and epitrochlear nodes. (Data gap) axillary nodes. COMPREHENSIVE CLINICAL WRITEUP 7 Musculoskeletal: Body parts normally alignment, muscle mass symmetrical, tone normal and equal bilateral. Rt knee is swollen, warm and tender to touch with restricted knee flexion upto 120 and strength 3/5. Knee circumference rt 17.5 inches lt 16 inches. (-) deformity and crepitus over joints; unrestricted and pain free active ROM of neck, upper and lower extremities (except rt knee joint) against gravity and full resistance, strength 5/5. Neurological: Oriented to time, place and person (GCS 15/15), coherent mood and affect, speech fluent and clear, good comprehension and appropriate judgment. Light touch, pain, point localization equal bilateral. Thumb to finger and finger to nose movement was sluggish but to the point. Cranial nerve (CN) III, IV, V, VI (refer eyes section). Cranial nerve VII, IX, X, XI, XII intact. CN XIII (refer ear exam). Biceps, triceps reflex, brachioradialis and Achilles reflex +1 bilateral; planter reflex normal. (Data gap) vibration, position sense, two point discrimination patella reflex, rennies and weber’s test, CN I and II, gait and balance, graphesthesia, stereognosis, extinction. LAB TEST Lab test WBC RBC HB/HCT MCV MCHC RDW PLT Neutrophils % Lymphocyte % Monocyte % Basophil % Eosinophil % Absolute Neutrophil count Monocytes Lymphocyte Eosinophil Nov 6th, 2012 7970 2.94 (Low) 8.7/27.5 (Low) 93.5 31.6 20.5 (High) 203 51.7% 23.6 (Low) 23.2 (High) 0.1 1.1 4120 Lab test Na K CL CO2 Urea Cr Glucose Ca Mg CRP ESR Lab test Uric acid Nov 6th, 2012 142 4.2 108 20 17 1.2 120 (High) 8.0 (Low) 1.2 (Low) 8.2 (High) 123 (High) Feb, 2012 7.0 mg/dl (High) 1850 (High) 1880 90 (Low) DIAGNOSIS/PROBLEM LIST Potential problems from chief complain Based on clinical presentation and history, following are the differentials diagnosis for this patient. 1. Crystal arthritis (Gout) According to Burrows et al (2012) hot swollen knee with acute non-traumatic knee effusion is common manifestation of crystal arthritis. It is an acute inflammation due to crystallization in the joint, and is associated with erythematous, warm, tender, swollen joint. Even minimal range of motion is exquisitely painful. It also involves fever, malaise, COMPREHENSIVE CLINICAL WRITEUP 2. 3. 4. 8 elevated WBC, CRP and other inflammatory reactants. And is usually common in patients with gout. Osteoarthritis According to Calmbach (2007), osteoarthritis is non-inflammatory condition in which patient presents with knee pain and swelling that is aggravated by weight-bearing activities and relieved by rest. The patient has no systemic symptoms but usually awakens with morning stiffness that dissipates somewhat with activity. In addition to chronic joint stiffness and pain, the patient may report episodes of acute synovitis and effusion. Subcutaneous Prepatellar Bursitis Aoron, (2011) and Allen (2012) reports that pre patellar bursitis is one of the causes of knee pain. It is the inflammation of subcutaneous prepatellar bursa and the superficial infrapatellar bursa that is manifested as knee swelling and pain, erythema, warmth, local tenderness to palpation, pain with flexion, crepitation and bursal effusion. Pain is usually relieved with rest. The etiologies mainly include inoculation of organism, particularly staphylococcus and streptococcus species; and due to noninfectious etiologies like trauma, repeated motion of joint, gout. Septic arthritis (infectious arthritis or bacterial arthritis) PubMed Health (2011) defines it as an inflammation of a joint that's caused by infection that is spread from another areas of the body or wound. Typically, septic arthritis affects one large joint in the body, such as the knee or hip. It is presented with chills fatigue and generalized weakness, fever, inability to move the limb with the infected joint, severe pain in the affected joint, especially with movement, swelling (increased fluid within the joint), warmth (the joint is red and warm to touch because of increased blood flow. COMPREHENSIVE CLINICAL WRITEUP Differential Crystal arthritis (Gout arthritis) Supporting evidence Hot, swollen knee Knee pain that worsens with movement Elevated CRP , ESR High serum uric acid Knee effusion Patient is known case of gout Osteoarthritis (noninflammatory arthritis) Knee pain Swelling Joint effusion Pre patellar bursitis Knee swelling Pain and local tenderness Warmth Pain with flexion Septic arthritis Severe pain in joint, especially with movement Swelling Warmth Effusion 9 Negating evidence Malaise Fever Erythema Patient’s pain was same throughout the day unlike osteoarthritis pain that is worse in the morning. Elevated CRP and ESR does not support this diagnose because osteoarthritis is noninflammatory condition. Patient did not have joint stiffness. Patients’ pain worsens with activity whereas, osteoarthritis pain dissipates with activity. Negative history of repetitive motion or kneeling, trauma. Erythema Crepitation Pain did not relieved with rest Bursal effusion Chills Fatigue and generalized weakness Fever PLAN Diagnostic studies: Synovial fluid aspirate and analysis Burrows (2012) reports that as per orthopedic association guidelines, synovial aspirate does not only help diagnosis in patient with knee pain but it also reduces the pain caused by joint COMPREHENSIVE CLINICAL WRITEUP 10 swelling. According to Courtney (2009) identification of monosodium urate (MSU) crystals in synovial fluid or in an aspirate of a tophus is considered the gold standard for definitive diagnosis of crystal (gout) arthritis. According to ClinLab, following are the key findings pertinent to different types of effusion to guide the diagnosis. Test Non inflammatory Septic arthritis Crystal arthritis (Osteoarthritis) (Gout) Color Yellow Gray-green Yellow-milky WBC 0-2000 50,000-200,000 50-10,000 Crystal Absent Absent Present Culture Sterile Positive Sterile Uric acid levels According to ClinLab, elevated serum urate level > 6.8mg/dl is associated with gouty arthritis. In lieu of patient’s inconsistent compliance to colchicine, I would like to repeat the uric acid level as the last level was done in Feb 2012. Treatment: Following treatment regimen is proposed on the basis of strong clinical presumption of gout arthritis. However, if synovial fluid analysis results and serum uric acid level redirects the medical attention to any other differential diagnoses listed above, treatment plan would be modified accordingly. Acute management According to Gonzalez (2012), during the acute attack, nonsteroidal anti-inflammatory drugs (NSAIDs) and colchicine are considered as first-line treatment for relief of acute pain. Among the NSAIDs, indomethacin and naproxen (1,000–1,500 mg/day) have been approved for acute gouty arthritis. However, considering the gastroenterological effects (bleeding) of NSAIDs and the risk of renal dysfunction in elderly, Gonzalez (2012) proposes that that the use of nonselective NSAIDs in patients over the age of 65 years be avoided. Thus, colchicine would be prescribed to the patient with dose ranging from 1.8 mg to 4.8 mg/24hours in divided doses every 6 hourly. He also suggests that systemic corticosteroid (eg., prednisolone) is a treatment option for patients who have contraindications to NSAIDs and colchicine. Initial dose of 50–60 mg/day is advised which can be readjusted later to maintain satisfactory response. Intraarticular injection of a long acting steroid is another potential therapeutic approach that may be effective at alleviating pain associated with an acute monoarticular attack. Chronic management Long term management is also critical in these patients to prevent the reoccurrence of acute symptoms. Allopurinol, probenecid or febuxostat have been recommended for chronic gouty arthritis. Allopurinol, a xanthine oxidase inhibitor acts by blocking the production of uric acid through a reduction in purine catabolism. (Gonzalvez, 2012) Patient education Patient would be educated to reduce the intake of foods that are high in purine, such as animal products, which helps control your body's production of uric acid. Fluid intake would be also encouraged to help flush uric acid from your body (Mayoclinic). Patient education would also include the effects, purpose and side effects of the medications and the procedure “synovial fluid aspirate”. COMPREHENSIVE CLINICAL WRITEUP 11 Follow-up: The patient would be kept in ER till the synovial fluid analysis and serum uric acid results are back and patient’s acute pain is settled. Thereafter, patient would be discharged on the treatment plan listed above. Follow up with primary doctor would only be needed if symptoms aggravate to affect other joints, pain is refractory to the prescribed regimen, quality of life is affected due to pain or restricted joint movement, and/or patient develops adverse effects to the treatment. However, patient would be advised to see the primary physician as soon as possible for his blood pressure concern. Problems from preexisting medical conditions and signs and symptoms Uncontrolled systolic HTN (Unresolved) Hyperglycemia (Unresolved) Dyspnea and wheeze Vision and hearing impairment (Unresolved) Anemia (Unresolved) Electrolyte imbalance (hypomagnesemia). Treated in ER Oral thrush (Unresolved) Follow up for prostat (On going ) Reference Aaron, D.L., Patel, A., Kayiaros, S.,& Ryan Calfee, R. (2011). Four Common Types of Bursitis:Diagnosis and Management. Journal of the American Academy of Orthopaedic Surgeons, Vol 19 (6),pp. 359-367 Allen, K.L. (2012). Prepatellar Bursitis Clinical Presentation. Retrieved from http://emedicine.medscape.com/article/309014-clinical#a0217 Burrow, V., Murray, J.R., Smitham, P., et. Al (2012). Are we managing acute knee effusion well? British Journal of Medical Practitioners, vol 5(1). Calmbach, W. L.,& Hutchens, M. (2007). Evaluation of Patients Presenting with Knee Pain: Part II. Differential Diagnosis. American Family Physician, 68(5), pp 917-922. Courtney, P.,& Doherty, M. (2009). Joint aspiration and injection and synovial fluid analysis. Best Practice & Research Clinical Rheumatology , 23, 161–192 ClinLab Navigator. Test interpretation. Retrieved from: http://www.clinlabnavigator.com/testInterpretations.html. Gonzalez, E. (2012). An update on the pathology and clinical management of gouty arthritis. Clinical Rheumatol, vol 31:13–21, DOI 10.1007/s10067-011-1877-0 COMPREHENSIVE CLINICAL WRITEUP Mayoclinic. Gout diet. What’s allowed and what is not?. Retrieved from http://www.mayoclinic.com/health/gout-diet/MY01137 PubMed health. (2011). Septic arthritis. Retrieved from http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001466/ 12