Drugs & Blood
advertisement

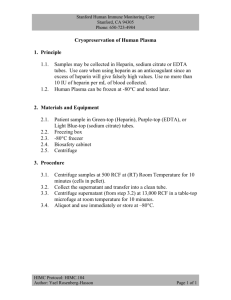
Pharmacology 301.6 Module 6 DRUGS & BLOOD Anticoagulants, anti-platelet & fibrinolytics Treatment of anemia Causes of death in Canada 1997: 661 deaths/100,000 http://www.statcan.ca/english/Pgdb/health30b.htm stroke injuries liver cancer lung other heart disease Heart disease and stroke = 1 of 3 deaths, due to clotting Blood fluidity The endothelial lining is non-thrombogenic Balance between procoagulants (thromboxane, thrombin, activated platelets, platelet factor 4) and anticoagulants (heparan sulfate, prostacyclin, nitric oxide, antithrombin) 1. heparin & derivatives – stimulate natural inhibitors of coagulant proteases (antithrombin) 2. coumarin anticoagulants – block multiple steps in the coagulation cascade 3. fibrinolytic agents – lyse pathological thrombi 4. antiplatelet agents – aspirin The Hemostatic System Accidental injury vs. pathological injury hypercholesterolemia, diabets, hypertension Coagulation cascade – platelet activation and coagulation vasospasm platelet plug fibrin plug Recanalization platelets (5HT, TXA2) adhesion, activation, aggregation extrinsic, intrinsic (humoral) fibrinolysis Platelet function disruption of endothelium platelet adhesion agonist binding • thrombin platelet activation platelet release platelet aggregation • serotonin • ADP • TXA2 Platelet adhesion and aggregation Platelet activation Antiplatelet drugs Arachidonic acid Aspirin ADP stimulates Thromboxane (from activated platelets) Clopidogrel ticlopidine inhibit P2Y receptor TXA2 recep clotting Ca2+ Lowers cAMP Increased cAMP clotting Prevents clotting GpIIb-IIIa Receptor for Eptifibatide fibrinogen and Abciximab platelet adhesion Tirofiban Dipyridamole (prevents breakdown by phosphodiesterase) How does it work? Aspirin efficacy Aspirin irreversibly inhibits platelet COX enzyme Platelets cannot synthesize new COX (no nucleus) No thromboxane (procoagulant, vasoconstrictor) synthesis Low dose aspirin (80-160 mg) does not inhibit endothelial COX Prostacyclin (anticoagulant, vasodilator) formation not affected Aspirin reduces clots by 15%, on average. 2% have a bleed, that is serious each year. Use in high risk clotters. Antiplatelet drugs Ticlopidine (TICLID)- is a prodrug Blocks platelet ADP receptor and prevents activation and aggregation Is often used in combination with aspirin (synergistic action), for angioplasty and stenting surgery To prevent secondary strokes and in unstable angina Severe neutropenia – 1% of patients Clopidogrel (PLAVIX) Similar to ticlopidine and used same way Less incidence of neutropenia or thrombocytopenia Used in combination with aspirin Blood coagulation cascade See the figure in textbook Brenner’s Factor IIa Activated partial thromboplastin time (aPTT) & prothrombin time (PT) Blood clots in 4-8 min in a glass tube Chelation of ca2+ prevents clotting Recalcified plasma clots in 2-4 min Addition of negatively charged phospholipids and kaolin (aluminium silicate) shortens clotting time to 26-33 sec – aPTT Addition of ‘thromboplastin’ (a saline extract of brain – tissue factor and phospholipids) shortens clotting time to 12-14 sec – prothrombin time (PT) Anticoagulants - Heparin Heparin is a glycoasminoglycan – alternating glucuronic acid and N-acetyl-D-glucosamine residues – sulfate and acetyl groups. Avg mol. wt - 12,000 daltons Heparin is negatively charged Heparin HEPALEAN Heparin – Source and function Heparin - originally isolated from the liver Found in mast cells -storage of histamine & proteases Rapidly destroyed by macrophages Normally not detected in the blood Heparan sulfate - similar to heparin but less polymerized - contains fewer sulfate groups Found on the surface of endothelial cells and in the extracellular matrix Interacts with circulating antithrombin to provide a natural antithrombotic mechanism Heparin & LMW Heparins difference in action Heparin ~ 45 saccaharide units MW ~ 13,500 This reaction goes 1000 to 3000 times faster with heparin. Antithrombin inhibits thrombin, Xa, IXa and to a lesser extent VIIa Low Mol. Wt. Heparin ~ 15 saccaharide units MW ~ 4,500 circulates in the plasma rapidly inhibits thrombin only in the presence of heparin Heparin – Toxicity - Hemorrhage Hemorrhage – recent surgery, trauma, peptic ulcer disease, platelet dysfunction Life-threatening bleeding can be reversed by protamine sulfate - 1 mg of protamine sulfate for every 100 U of heparin - slow iv infusion – 50 mg over 10 min) Protamine sulfate interacts with platelets, fibrinogen, and other clotting factors - an anticoagulant effect – at higher doses Anaphylactic reactions to protamine (a basic protein isolated from Salmon sperm) Heparin-induced Thrombocytopenia 50% decrease in platelet count - <150,000/μl) Antibodies against complexes of heparin with platelet factor 4 In 3-5% of patients 5 to 10 days after initiation of heparin therapy Lower incidence with low mol wt heparin In 1/3 of pts is preceded by thrombosis Can be life-threatening Stop heparin immediately Alternative anticoagulants – lepirudin or danaparoid Low Molecular Weight Heparins Avg mol. wt 4,500 daltons - 15 monosaccharide units Better absorbed - higher bioavailability Longer biological half-life More predictable dose-response - does not bind to plasma proteins, macrophages, or endothelial cells Can be given s.c. without lab monitoring in an outpatient setting Cleared unchanged by kidney (do not use in renal failure!) rather than by the reticuloendothelial system Lower risks of thrombocytopenia and bleeding Safety and use during pregnancy not evaluated LMW heparins Dalteparin (FRAGMIN) Enoxaparin (LOVENOX) Uses: 1. prevention of venous thromboembolism 2. Treatment of venous thrombosis, pulmonary embolism and unstable angina 3. prophylaxis following total knee arthroplasty Other parenteral anticoagulants Danaparoid (ORGARAN) nonheparin glycosaminoglycans (84% heparan sulfate) Promotes inhibition of Xa by antithrombin Prophylaxis of deep vein thrombosis In patients with heparin-induced thrombocytopenia Lepirudin (REFLUDAN) recombinant derivative of hirudin (a direct thrombin inhibitor in leech) In patients with heparin-induced thrombocytopenia Oral anticoagulants – 4-hydroxycoumarins Gamma glutamic acid residues of clotting factors must be carboxylated for enzyme activity factors II, VII, IX, X, Prots C and S Vitamin K Vit.K epoxide Coumarins reductase Coumarins are act here competitive inhibitors Warfarin COUMADIN Coumarins (warfarin) • inhibits vitamin K reduction • efficacy measured by INR (International Normalized Ratio), the patient’s PT divided by the PT in pooled plasma • takes 4-5 days to become effective – active carboxylated factors in plasma need to be cleared • small Vd, steep D-R curve, metabolized by CYP1A and CYP2C9 (interactions) • Warfarin crosses placenta – is teratogenic – birth defects and abortion • major indications: DVT, PE and atrial fibrillation Warfarin – drug & other interactions Any substance or condition is dangerous if it alters: 1. the uptake or metabolism of oral anticoagulant or vitamin K 2. the synthesis function or clearance of any factor or cell involved in hemostasis or fibrinolysis 3. the integrity of any epithelial surface Warfarin - Clinical uses Prevent acute deep vein thrombosis or pulmonary embolism Prevent venous throboembolism in patients undergoing orthopedic or gynecological surgery Prevent systemic embolization in patients with myocardial infarction, prosthetic heart valves or chronic atrial fibrillation Warfarin - Antidote Vitamin K (oral or parenteral) INR = (PTpt / PTref)ISI Target 2.0 to 3.0 Fibrinolytic process Streptokinase binds here – generalized action t-PA has to bind here – localized ation Efficacy of thromobolytics 1.8% have serious bleeding; 0.7% have IC haemorrhage Streptokinase (STREPTASE) Binds plasminogen- coverts to plasmin Dissolve clots after myocardial infarction, deep vein thrombosis, massive pulmonary emboli Side effects: Bleeding, allergic reactions, hypotension, fever. Tissue plasminogen activator (t-PA) – (alteplase, ACTIVASE) activates fibrin bound plasminogen (less systemic plasmin formation) More expensive than streptokinase Summary • we have lots of drugs that affect hemostasis • they can inhibit platelet function, fibrin formation, or fibrinolysis. • using combinations prevents more clots, but causes more bleeding. • look at the risk/benefit ratio. Anemia a reduction in the hemoglobin, hematocrit ( % of whole blood that is comprised of red blood cells) or red cell number Erythropoiesis - Pluripotent stem cells differentiate under the influence of growth factors (erythropoietin) to form erythrocytes controlled by a feedback system in the kidney - responds to changes in oxygen delivery - secretes erythropoietin (a glycoprotein) from peritubular interstitial cells - stimulates the marrow cells Feedback - disrupted by kidney disease, marrow damage or a deficiency in iron or an essential vitamin. Anemia Iron deficiency is the most common cause of anemia Results in microcytic hypochromic anemia Iron deficiency also affects iron-dependent enzymes such as cytochromes, catalase, peroxidase, xanthine oxidase and mitochondrial enzyme α-glycerophosphate oxidase Iron deficiency has also been associated with learning problems in children Iron in the body mg/kg of body weight Essential iron Male Female Hemoglobin 31 28 Myoglobin 6 and enzymes Storage iron 13 5 Total 37 50 4 Treatment of Iron Deficiency The ability of the patient to tolerate and absorb medicinal iron is important Gastrointestinal tolerance to oral iron is limited Mainly absorbed only in the upper small intestinal (delayed-release preparations ?) Parenteral iron Iron dextran injection (INFED, DEXFERRUM) Acute hypersensitivity, including anaphylactic reactions, can occur in from 0.2% to 3% of patients. Iv is preferred – more reliable response Im route – more local side effects – skin discoloration, long-term discomfort, concern about malignant change at injection site Megaloblastic (macrocytic) anemias Due to lack of folic acid or vitamin B12 Deficiency more common in older adults Folate – food fortification – masks cobalamin deficiency (neurologic damage) In pregnancy - prevention of folate deficiency and permanent neural tube defects in children minimized Folate and Vitamin B12 Interaction Tetrahydrofolate is necessary for DNA synthesis Cobalamin and folate are cofactors for tetrahydrofolate production Deficiency of either impairs cell division in the bone marrow while RNA and protein synthesis continues – enlarged erythrocytes Cobalamin deficiency – impairs synthesis of S-adenosylmethionine – necessary for proper nervous system functioning Pernicious anemia Lack of intrinsic factor – Vit. B12 not absorbed Injury to parietal cells or autoantibodies Vitamin B12 - must be administered– is not synthesized in body Treating deficiencies Distinguishing B12 deficiency from folic acid deficiency Folic acid will supply folate needed for DNA synthesis Anemia corrected It DOES NOT correct the lack of methionine and succinyl Co-A synthesis – this will cause neurological deficits Folic acid therapy Rule out underlying cobalamin deficiency Folinic acid (leucovorin calcium, citrovorum factor) – 5-formyl derivative of tetrahydrofolic acid To circumvent the inhibition of dihydrofolate reductase as a part of highdose methotrexate therapy To counteract the toxicity of folate antagonists such as pyrimethamine or trimethoprim More expensive