UTIslidescommunitypharmacists
advertisement
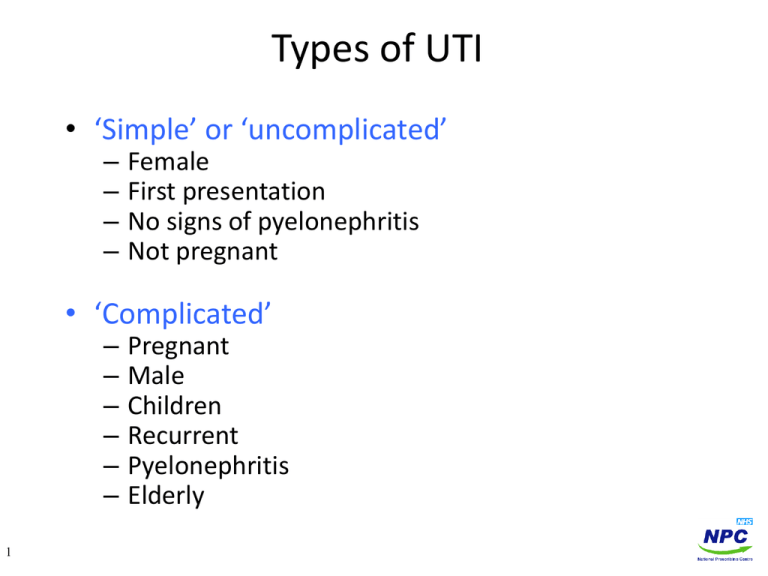
Types of UTI • ‘Simple’ or ‘uncomplicated’ – – – – Female First presentation No signs of pyelonephritis Not pregnant • ‘Complicated’ – – – – – – 1 Pregnant Male Children Recurrent Pyelonephritis Elderly So what could it be? Prodigy Urinary Tract Infection (cystitis) • Typical features include: – Dysuria, frequency, urgency, nocturia, haematuria, suprapubic pain, cloudy or smelly urine – Caused by bacteriuria, defined as >105 organisms/ml (102-104 if under sterile conditions) – ‘Simple’ UTIs are rarely associated with renal failure or sepsis (Hummers-Pradier. Br J Gen Pract 2002; 52: 752-761) Acute pyelonephritis • As above plus: – fever (>38.5oC), loin/flank pain/tenderness, rigors, nausea, vomiting and malaise – Can be life-threatening so requires urgent treatment ‘Urethral syndrome’ • As cystitis but no bacteriuria Sexually transmitted disease e.g. chlamydia, gonorrhoea, herpes simplex, Candida Other causes can include drugs (e.g. cyclophosphamide, NSAIDs), parasitic infection, female menopause 2 So what are the management options here? A 25 year old lady presents with a 48 hour history of needing to “go the toilet a lot to pee” and it hurts when she does. She also thinks she may have seen blood in her urine. If we diagnose a ‘simple’ UTI (assuming she is not pregnant and she has no history of UTI): • Prognosis is good: – Unlikely to cause serious complications – But symptoms are unpleasant (to say the least) • Up to 50% have no significant bacteriuria. • Up to 50% will self-resolve in a few days, even without treatment. – Giving antibiotics may cause more harm than good – May disturb natural gut/vaginal flora and encourage Candida growth. • Can we predict who is more likely to have a bacterial cause for their UTI? 3 Signs and symptoms to help predict a bacteriuria Bent S, et al. JAMA 2002; 287: 2701-2710 • The prevalence of a bacterial UTI in a young woman is around 12% • If she has certain signs and symptoms, this likelihood increases: – – – – – Dysuria (by about 1-2 times) Frequency (by about 1-2 times) Blood in urine (by about 2 times) No vaginal discharge (by about 3 times) No vaginal irritation (by about 3 times) • So if more than 3 of these are present, it is reasonable to assume a bacterial cause for the symptoms – >70 out of 100 women will have a bacterial cause 4 What do the guidelines recommend wrt dipstick testing? Prodigy • If the woman has several clinical features typical of lower UTI – Treat empirically without testing as urine dipstick test not helpful • If the woman has few clinical features typical of lower UTI – Dipstick test the urine: • Dipstick test positive (nitrite and LE both positive), diagnose UTI • Dipstick test equivocal or negative (either or both negative), consider other causes Our thinking: • If ‘barndoor’ symptoms (>3), don’t bother with the dipsticks – a negative test may mislead you • If diagnosis is unsure (1-2 symptoms) use them • But don’t expect them to tell you the ‘right’ answer each time 5 Dip-sticking • Urine dipsticks can be used when an uncomplicated UTI is suspected, but cannot be relied upon to definitely exclude or confirm a diagnosis. A positive nitrite test indicates bacteria in the urine (which have reduced nitrate to nitrite) and therefore suggests UTI. However, a negative test does not rule out UTI because some pathogens do not produce the enzyme needed for the reduction, and frequent urination reduces the time for the enzyme to act (morning specimens are most reliable [HPA]). • A leucocyte esterase (LE) test indicates white blood cells in the urine and also suggests that a UTI may be present, although contamination of the specimen can give a false-positive result. A negative test, does not rule out UTI since the test is insensitive and pyuria is not always present in UTI. 6 What does the PGD say? • • • • • • • Three or more of the following symptoms:Dysuria Frequency Blood in urine Absence of vaginal discharge And no exclusions consider treatment. Or one or two symptoms and a strong possibility of a UTI test with a dipstick- A nitrite and/or leucocyte dipstick must be positive • Patients may also have suprapubic pain, cloudy or foul smelling urine • Vaginal discharge reduces the likelihood of the woman having a bacteria urinary tract infection 7 What agent and for how long? Prodigy, SIGN: • A 3 day course of trimethoprim is effective for ‘simple’ UTI • Nitrofurantoin is an option, but may be less convenient for patients Cochrane Review – Milo G, et al. Date of last amendment 22 Feb 2005 • Compared the success of 3 day regimens with 5 days or more • For symptomatic failure rates, no differences were seen • For bacteriological failure rates, 3 days was slightly less effective • Adverse effects were more common with longer courses • Bottom line:- 3 days is fine for simple UTI, but not for those in whom bacteriological cure is important, such as pregnancy 8 Simple UTIs - conclusion • Look for ALARMS (temp>38.5oC, rigors, vomiting etc) • Simple UTIs are generally self-limiting, non-serious infections but can be very unpleasant • Use decision rules to help with diagnosis: – >3 symptoms (and self-reported) very likely to be bacterial cause – 1-2 symptoms only - test with dipsticks (but they can mislead) • Management options: – Empirical antibiotics • 3 days trimethoprim or nitrofurantoin – Delayed prescription – Symptomatic treatment ± delayed prescription 9 Case Study (npci.nhs.uk) Beccie is a 25 year old woman who presents with a 48 hour history of needing to urinate frequently, and it hurts when she does. She also thinks she may have seen blood in her urine but wasn't sure. What other information about her clinical history would you like to know? List all of the relevant pieces of information that would be useful in diagnosing a simple UTI. 10 Model answer • • • • • • • • • 11 What other information about her clinical history would you like to know? List all of the relevant pieces of information that would be useful in diagnosing a simple UTI. Sexual history Had a UTI before? Childhood history of bladder or kidney problems Likely risk of pregnancy Medication history (cyclophosphamide or NSAIDs can cause bladder irritation) Foreign travel (parasitic infection) Simple UTI is the diagnosis in young, sexually active, non-pregnant women where it is not recurrent. UTIs in pregnant women, in older women that are recurrent or in men, are not simple UTIs and need a different management approach. CKS guidance is very useful for these patients. • What other symptoms and signs would be useful? List all of the signs and symptoms you would need to ask the patient about to be able to diagnose a simple UTI. 12 Model Answer • Dysuria • Frequency • Vaginal discharge • Vaginal irritation • Loin or flank pain • Temperature • Rigours • Nausea and vomiting • General malaise If systemic symptoms such as loin/flank pain or rigours are present, a upper UTI or pyelonephritis should be considered. Again the management of this condition is very different to that of a simple UTI. 13 • Beccie reveals the following information: • She has never had a UTI before either as an adult or a child. • She has no back or loin pain as well as no vaginal irritation or discharge. • She takes the oral contraceptive pill and tells you it is extremely unlikely she is pregnant as she had her period last week. • She takes no other medication at all. • Her temperature is normal 14 • Which of the following tests, signs or symptoms are most strongly correlated to the presence of a bacterial UTI? Rank each item on your list with 10 meaning the diagnosis is very likely and 0.1 being extremely unlikely: • • • • • • • • • 15 0.1, 0.5, 1, 2, 5, 10. Dysuria Frequency Vaginal discharge Vaginal irritation Positive nitrite test Positive leucocyte esterase test No raised temperature Blood in urine Model answer Likelihood ratios for these signs and symptoms (number of times more likely they are to have a bacterial cause for UTI symptoms if they have this sign/symptom compared with those who do not have a bacterial cause) are: • • • • • • • 16 Dysuria 1.5 Frequency 1.8 Vaginal discharge 0.3 Vaginal irritation 0.2 Positive nitrite test* 6 Positive leucocyte esterase test* 1.5 Blood in urine 2.0