Understanding and Responding to your Ancillary Care Weaknesses
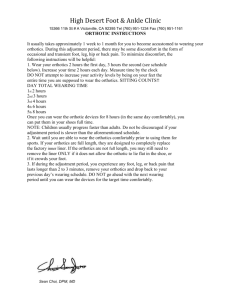
advertisement

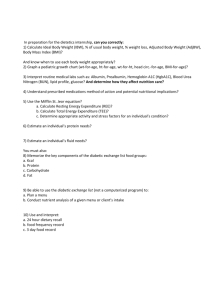
Cindy Pezza, PMAC What is Considered Ancillary Care? Any service or treatment above and beyond the diagnosis and statement of treatment plan. . Which Type of Care do you Provide? Addressing the immediate problem or conditionderiving a diagnosis and suggesting treatment options? Or. . . Do you strive to provide your patients with the highest quality comprehensive care, utilizing your expertise, modern technologies and the best possible products and services available? Either way, your Patients Improve, Right? Possibly. . . However, physicians who provide much needed ancillary services to their patients, see improved results, in less time. Improved compliance= improved outcome They Also See. . . Happier patients A greater referral base An improved reputation AND. . . The reward of increased practice revenue. Beware of Tunnel Vision DPMs are too busy “seeing” patients, and may overlook what is truly needed. Which Services are you Offering? Digital X-ray Vascular Testing ENFD testing (for neuropathic patients) Medical Supplements Prescription and medical grade orthotics Diabetic Prevention/Treatment plans Fall Prevention programs In-Office dispensing products Laser treatment (nails, skin, warts, pain) The advantages of being a Doctor of Podiatric Medicine: DPMs act as the Prescriber and the Supplier for many of the much needed items and services that patients require. A WIN, WIN for the practice and the Patient! The Infamous and Misunderstood CDFE By taking the time to perform and document the findings of the “Comprehensive Diabetic Foot Exam” you can determine a patient’s need for many different ancillary services. The Diabetic Shoe Program Yes, the compliance regulations are becoming more taxing and it seems as if it’s not worth the trouble. Don’t Go it Alone Train your staff to assist with (or run) these types of programs. Once they understand the rules and become confident in their ability, staff becomes invaluable . Consider This: You have 200 Diabetic Patients in the Practice. 150 of them qualify for therapeutic shoes and inserts. You fit only 100 (who wants to chase all that paperwork?). . . Numbers Don’t Lie Your average profit from A5500 (2 units) and 3 pairs of A5512 (pre-fabricated inserts) (6 units) is about $200. 100 patients x $200 = $20,000 Imagine if you fit nearly ALL of your patients who qualified? So Start Looking Train Staff to look ahead in the schedule and make sure each diabetic patient has been scheduled for an annual (more frequently if they are at higher risk) CDFE. Measure and Manage Have staff assist with the exam, the documentation (including PQRS qualifying measures), procurement of compliance paperwork, measuring shoe size, selecting the appropriate shoe style and proper dispensing technique. But, That’s Not All If you find that during the CDFE, the patient has increasing neuropathic symptoms, diminished pulses, discoloration of the lower legs and feet, they may need: ENFD testing (biopsy) Vascular testing Medical supplements Compression stockings And Then. . . Your Medical Assistant (trained in performing a fall risk assessment and casting for custom braces) notices that it took Mr. Greene 3 tries to get out of her chair in the reception area, and that she had to hold on to the wall as she shuffled towards the treatment room? Mr. Greene May Need: An Assessment to determine his risk of falling A referral to Physical Therapy (within your practice or to a mutual referral source) Casting and dispensing of B/L balance devices . . . By NOT Addressing the Issues: You provide a dis-service to your patients And become. . . Just another doctor who says: “You’re just getting older, these things happen.” Or (the worst one of all) “It’s just arthritis, no need to worry.” You have the Knowledge and Resources You have the elderly population that is unsteady (and falling or that is afraid of falling) Set a goal to perform just ONE Fall Risk Assessment (FRA) per day Again, the numbers. . . Perform 4-5 (FRA) per week (1 per clinic day) Cast (and dispense) ONE high or extreme fall risk patient for bilateral balance braces Custom balance devices - *cost to the practice = $600-700/pair Reimbursement averages$2100 per pair (a little over $1000 per brace) Profit of $1400-$1500 per pair (patient) Okay, Take a Vacation Do the Math $1400/week x 50 weeks = $70,000 Worth a little paperwork, and the ability to keep our patients off the floor and enjoying their quality of life! What about This Patient? Are you Just Cutting her Nails? Or, are you giving options? 1. Do nothing and the condition gets worse 2. Have surgery and use a fixation device to stabilize the ankle? 3. Offer a low profile, custom brace that will allow her to stay active and comfortable and slow the progression of the condition What would you Choose? Staff can be your Eyes and Ears If they are trained to understand all that you can offer patients and how easy it is to help. Teach Them The appropriate questions to ask during initial evaluation and follow-ups, to allow you to quickly diagnose and develop a treatment plan. The more they know, the more value they add to patient care and practice revenue. Let’s Talk Cash Increased copayments, enormous deductibles, and other out of pocket expenses, make it an ideal opportunity to offer cash products and services to your patients. The Wave of the Future is Here Now! Become a One Stop Shop Carry items that you recommend the most: Antifungals Shoe Sprays Diabetic Safe lotions Proper Footwear Drying agents Medical Grade orthotics Only if You are a Believer If you do not truly believe in the quality and efficacy of the products, get out your dust rags. Expensive, Shiny Things The same concept applies to lasers, and other modern technologies with lights and buzzers. If you Invest the Money Train your staff on: How it works How to use it properly (if allowable) The benefits of use The cost of the machine The cost to patients The importance of compliance Take a Closer Look. . . If you do your research and find the right ancillary services to meet the needs of your patients and they don’t produce the desired effect. Choose Wisely Select the appropriate products, services and treatments to fit the needs of your patients. Train your staff Market your services within and outside of your practice Educate your patients And reap the benefits of improved outcomes Measure and Manage To increase compliance, outcome and revenue. . . All through the proper utilization of Ancillary Services Plantar Fasciitis/heel pain Classic Presentation Assistant questions/evaluation Where is the pain (ask patient to point to where the pain is located and if it radiates)? How long ago did you notice this pain (days, weeks, months, longer)? Describe the pain (aching, burning, throbbing, stabbing, sharp, dull, constant, intermittent) Can you recall an injury or change in routine that may have caused this pain (trauma, increased or more strenuous exercise, different or new shoes, etc.)? Evaluation continued. . . Is your pain at its worst in the morning (upon your first steps) or upon standing after you have been sitting or driving for an extended period of time? What have you tried at home to relieve the pain (icing, stretching, rest, OTC pain relievers or antiinflammatories)? Do you wear or have you ever worn any type of insert in your shoe? Yes/No • Do not use verbiage like “orthotics” on the first visit, most patients do not know what an orthotic device is or what it does Have you ever experienced a similar condition in the past? Actions/treatment plan Post Evaluation: by DPM or MA=Medical Assistant 3 views of the foot and 2 calcaneal views are taken [MA] Diagnostic ultrasound is performed to measure the thickness of the plantar fasciia: (LT or RT or B/L to compare “normal” foot) [MA or DPM] • It is important to relay that ligament in its “normal” state measures between 2-3mm/compared to their measurement Injection w/cortisone: [DPM] Dispensing Dispense Air Heel, PF strap or similar: L1902 (LT or RT) • Instructions for use and wear reviewed by Assistant Or. . . Strapping (if not dispensing Air Heel/PF strap): 29540 (LT or RT); use -59 modifier on this w/ injection Educate your patients Discuss the importance of proper arch support and Dispense Footsteps (segway to custom devices or as stand alone) • Break in instructions reviewed by Assistant to include: Wearing devices 1-2 hours per day initially and increasing wear time gradually until comfort is achieved Proper verbiage Some fatigue of the feet or legs is common (be careful not to use verbiage like “ You may be in pain at first.” Better to say; “You may experience discomfort or mild achiness in the feet or legs while your body adjusts to wearing the devices. These are medical grade and much more substantial than OTC arch supports. This is completely normal and you should not be concerned.”) Be confident in your approach With any item dispensed (Self Pay or Billable), maintaining a high level of confidence with introduction, education, and instruction are essential (for both DPMs and staff). . . Encourage your staff to stay in the treatment room and listen to your “spiels” once they are perfected. Avoid phrases such as: “You may want to try” or “You can go to the pharmacy and look for something topical to use, that might help” Remember. . . You are the foot and ankle EXPERT. . . Believe in what you dispense and your patients will too! If yes to A.m. Pain . . . A Nightsplint is prepared to be dispensed Assistant to review instructions for use with patient L4397 **DME acknowledgement (receipt is signed by patient and copied for chart. Patient receives original receipt along with 30 Supplier Standards)** In addition Consider physical therapy if condition is of extended duration Assistant to prepare patient education (best to link commonly used Dx codes to URL and pull from Patient Education within EHR (for MU requirements) Examples: • Heel pain handout • Stretching exercises/icing/rest instructions • Instructions for proper break in of orthotics A complete treatment plan Rx for NSAIDs (if no contraindications or allergies) Biofreeze or other Topical Analgesic is Dispensed – instructions for use provided by MA Theraband Foot Roller (Kit) – instead of frozen water bottle, can of soup and dishtowel by the nightstand Follow-up Appointment is made - RTO in 2 weeks (to monitor compliance and improvement and to cast for orthotics (if amendable) Follow up visit If little or NO improvement: • Consider immobilization with cam walker (L4361) • • • • • Non-Pneumatic walker- does NOT inflate Consider serial injections Consider CT scan or MRI Consider labs for rheumatologic etiologies Consider TENS/ESWT Continue to monitor condition closely • Follow up in 1-2 weeks to review CT or MRI results (patient to remain in boot until improvement is noted) • With any condition, consider less conservative (invasive) methods of treatment (surgery, PRP, etc.) only after traditional treatment plans have been exhausted and thoroughly documented condition improved Continue with R.I.C.E. Consider serial injections to assist with healing process Cast for custom orthotics Follow up in 2 weeks to dispense orthotics and monitor continued progression Integrating protocols To integrate protocols for all common conditions in your practice, it is important that doctors and staff are “on the same page” and understand the measurable benefits of following them. These include: • Increased patient compliance • Increased referrals (patients will refer friends and family a comprehensive treatment plan is clear and they feel better in a shorter amount of time) • Increased revenue (PVV) A win-win situation Questions If you need help with implementing or improving the Ancillary Services in your practice. . cindy@pinnaclepa.com THANK YOU!