AHCA/NCAL Slide Template - Missouri Health Care Association
advertisement

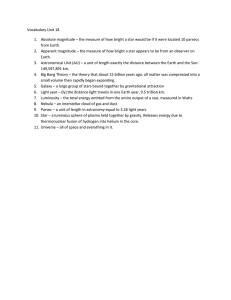
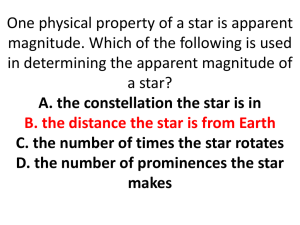
Value of your AHCA/NCAL Membership Presented by: Peggy Connorton & Urvi Patel Session Overview AHCA/NCAL Quality Initiative 2015-2018 AHCA/NCAL National Quality Award Program LTC Trend Tracker Questions? 2015- 2018 Cornerstones for AHCA Quality Initiative 2015-2018 Aligning with national priorities Build on previous efforts Quality Initiative 2012-2015 Inclusive of post-acute care and long term care National Priorities Systems Outlook Model based on Baldrige and QAPI Philosophy Systems Orientation utilized to accomplish goals Organizational Success Increase Staff Stability Target: Decrease turnover rates among nursing staff (RN, LPN/LVN, CNA/LNA) by 15% or achieve/ maintain at or less than 40% by March 2018 Increase Customer Satisfaction Target: At least 25% of members will measure and report long-stay resident and family satisfaction and/or short-stay satisfaction using the Core-Q survey by March 2018 Reduce the Number of Unintended Health Care Outcomes by March 2018 Improve Short Stay/Post-Acute Care Safely Reduce Hospital Readmissions Target: Safely reduce the number of hospital readmissions within 30 days during a skilled nursing center stay by an additional 15% or achieve and maintain a low rate of 10% by March 2018 Improve Discharge Back to the Community Target: Improve discharge back to the community by 10% or achieve and maintain a high rate of at least 70% by March 2018 Adopt Functional Outcome Measures Target: 25% of members will adopt the use of the mobility and self-care sections of the CARE tool and report functional outcome measures Improve Long-Stay/Dementia Care Safely Reduce the Off-Label Use of Antipsychotics Target: Safely reduce the off-label use of antipsychotics in long-stay nursing center residents by 25% by Dec. 15 and by 30% by Dec. 2016 Safely Reduce Hospitalizations Target: Safely reduce hospitalizations among long-stay residents by 15% or achieve/ maintain a low rate of 10% or less by March 2018 Cornerstones for NCAL Quality Initiative 2015-2018 Set goals that are achievable and meaningful Consider what data is available through the Patient Safety Organization Alignment with AHCA goals NCAL Quality Initiative Goals (by March 2018) Keep nursing and direct care staff turnover below 40% At least 90% of customer (residents and/or families) are satisfied with their experience Safely reduce hospital readmissions within 30 days of hospital discharges by 15% Or reach (and maintain) a low rate of ≤5% rate Safely reduce the off-label use of antipsychotics by 15% Or reach (and maintain) a low rate of ≤5% rate How to Measure LTC Trend TrackerSM – AHCA/NCAL’s Turnover and Retention Upload CoreQ satisfaction questions National Patient Safety Organization for Assisted Living (PSO) National Patient Safety Organization for Assisted Living (PSO) Key Resource The Staff Stability Toolkit via AHCA/NCAL Bookstore Learn more at QualityInitiative.ncal.org Turning Complaints into Compliments INTERACT for Assisted Living Consumer Fact Sheet on Antipsychotic Drugs for Persons Living with Dementia Goal Tracking AHCA LTC Trend Tracker (staffing, Rehospitalization, antipsychotics, discharge to community) NCAL LTC Trend Tracker (staffing) PSO (antipsychotics and Rehospitalization) Soon to come CoreQ Quality Initiative Tracking Report AHCA/NCAL National Quality Award Program Background Launched in 1996 Approx. 10,000 applications and 4,000 awards Criteria based on the Baldrige Performance Excellence Program The mission of the AHCA/NCAL National Quality Award program is to promote and support the application of continuous quality improvement in AHCA/NCAL member organizations Three Levels of Distinction Organizations must achieve the award at each level to continue to the next level 1. Bronze – Commitment to Quality 2. Silver – Achievement in Quality 3. Gold – Excellence in Quality Number of Recipients 3,405 495 24 Number of Recipients in MO 39 7 1 Who is succeeding? Organization A Organization B Morning Stand-Up Morning Stand-Up Issues of the day: hostile family Issues of the day: hostile family member and no food delivery for the kitchen In the past, had the same issue with the produce delivery system member and no food delivery for the kitchen In the past, had the same issue with produce delivery system "Green Code" Reactive to Proactive Market Skilled Nursing Care Center Integrated Management System Mission, Vision and Values Workforce Customers Leadership & Strategy Results Operations Measurement, Analysis and Knowledge Management *Adopted from Quantum Performance Group Baldrige Core Values Visionary leadership Focus on the future Patient-focused excellence Managing for innovation Organizational and personal Management by fact learning Societal responsibility and Valuing workforce members and community health partners Focus on results and creating value Agility Systems perspective Baldrige and QAPI Baldrige Organizational Profile Leadership Strategy Customers Measurement, Analysis, and Knowledge Management Workforce Operations Results QAPI Design and Scope Governance and Leadership Feedback, Data systems, and Monitoring Performance Improvement Projects Systematic and Systemic Action Value Proposition Silver and Gold Quality Award recipients have better performance outcomes o Five Star Performance o Patient Health Care o Financial Five Star Off-Label use of Antipsychotics 30 Day Hospital Readmissions Occupancy Rate 2016 Program Cycle Event/Deadline Date Intent to Apply Launch Mid-September Intent to Apply Deadline November 19, 2015 Application Submission Launch December 7, 2015 Application Deadline January 28, 2016 Survey History Your Member Resource Resident Characteristics Staffing Information Cost Report & Medicare Utilization CMS Five Star Rating www.ltctrendtracker.com If you hear the word “data” and it makes you want to run just r it with the word “candy” Who Collects Data on LTC? Government Accountability Office (GAO) Office of Inspector General (OIG) Centers for Medicare and Medicaid Services (CMS) Centers for Disease Control – National Center for Health Statistics (NCHS) Trade Associations (NCAL, ALFA, Leading Age, ASHA, NIC) Hospital and Healthcare Compensation Why Data Matters Must manage by facts, not feelings Shows how well you are performing and areas for improvement Without we function in an atmosphere of blame problems are hidden results are excused people are blamed It’s a team effort! All staff are important in quality improvement. What People Know About You Hospitals track your data Five Star Yelp Google Facebook Twitter State Surveys Health Grades Word of mouth/reputation The Future of LTC Trend Tracker Fall 2015 Customer satisfaction questions aka “CoreQ”: Hospitalization report Five Star download Spring 2016 – Additional AL measures: o o o o 30-day hospital readmission rates Off-label use of antipsychotics Occupancy rates Lengths of stay Quality Initiative tracking report www.LTCTrendTracker.com What is Risk Adjustment Risk adjustment is a corrective tool used to level the playing field regarding the reporting of patient outcomes by adjusting for the differences in risk among specific patients. Risk adjustment also makes it possible to compare hospital and doctor performance fairly. Comparing unadjusted event rates for different hospitals would unfairly penalize those performing operations on higher risk patients (those who are sicker or have more comorbidities). Source: http://www.sts.org/patient-information/what-risk-adjustment Risk Adjustment Building A Building B Low Acuity High Acuity Admissions 100/year Admissions 100/year Rehospitalization Rate Rehospitalization Rate 15% 10%/month month Expected Rate 10% Expected Rate 15% Ratio 1 Ratio 1 Benefits of LTC Trend Tracker AHCA member resource Benchmarking against your peers Increases efficiency – saves you time Data in one central place – pulled using Medicare number AHCA Quality Metrics Rehospitalization Discharge to Community Length of Stay Data Source MDS 3.0 Over a 12-month period Based on admission assessment (5 day or OBRA) Discharge assessment Rehospitalization Measures National measures based on claims Excludes ER visits & observation stays Excludes Medicare Advantage & private insurance Most measures Fail to risk adjust for differences in patients Claims allow for limited clinical information to risk adjust Rehospitalization Data MDS 3.0-based measure Adjusted rate Expected rate Actual rate Use in telling your story to hospitals Benchmark your Rehospitalization to your peers Rehospitalization How to interpret your results How do I compare to others? – look at risk adjusted results Are you getting better? – look at your actual results Are you admitting sicker patients? – look at your expected Are you admitting more or less than expected? – look at your actual to expected ratio How to interpret your results Risk adjusted is getting better but your actual & expected have not - Means you are doing better compared to others but you are not improving much - Your admissions have about the same acuity over time (e.g. they are not sicker in Jun 2014 compared to Jun 2013 – based on expected rate) - Your ratio is 1.0 or less meaning you send fewer patients back to the hospital than expected (this is why your risk adjusted value is 3-4% points less than your actual (21% vs 18%)- however you still have room to do better since your ratio is close to 1.0 most of the time. Rehospitalization Report Actual Rehospitalization Risk Adjusted Trend How to talk to hospitals How to display for a hospital Expected VS Actual 25.00% 20.00% 15.00% 10.00% 5.00% 0.00% act Org Dec-12 17.60% Mar-13 12.50% Jun-13 12.70% Sep-13 14.40% Dec-13 16.10% Mar-14 16.50% Jun-14 16.20% Sep-14 15.00% act Peer 20.40% 20.30% 20.20% 20.10% 19.80% 19.80% 19.80% 19.60% Exp Org 22.30% 21.90% 22.80% 23.50% 23.50% 23.70% 23.60% 23.50% exp peer 20.50% 20.50% 20.50% 20.40% 20.30% 20.20% 20.10% 20.10% Show how your patients differ In this example the expected return is higher than the actual This means that this center is sending fewer patients back to the hospital they are expected They are doing better then their peers You could then show your correlation to other metrics such as five star and LOS Discharge to Community Determine how you compare in your d/c to community rate Private home, apartment, board/care, assisted living, or group home as indicated on MDS discharge assessment Uses MDS Data from the d/c assessment Discharge to Community Report How to use DC to Community See how you are doing on your dc rate to home and other nonclinical settings It can also tell you if you are sending more or fewer than expected individuals back to the community given the clinical characteristics of the population of individuals admitted to your center Use negotiations with hospitals, Manage Care organizations and others. Five Star Rating Reports 3 Reports Overall, Staffing and QM Report QM-- Identify focus QMs for quality improvement Predict impact of QM improvements on Five-Star QM Rating Predict Staffing Five Star Rating Five Star QM Report Look at your current QM Five Star Rating Determine QMs to focus from the Five Star QM Report Look at your current resident population Enter your scores and see the affect on your overall QM score Members use this report to see if they will maintain their five star rating Sample Five Star Overall Changes with Staffing Look at Staffing Five Star Report Determine expected vs reported o Did you enter the correct data during last survey? o What does CMS Expect you to run? Look At CASPER Staffing Report for reported hours Five Star Staffing Rating Five Star Staffing Report RN hours Five Star Staffing Report Five Star QM Rating SS Stay Antipsychotic LS Antipsychotic FUTURE CHANGES TO FIVE STAR IN 2015 & 2016 CMS plans to add additional quality measures to Five-Star • • • • Rehospitalizations Discharge back to community Staffing turnover and retention Other measures from IMPACT act Change how much measures contribute to scoring based on CMS audits of MDS and Staffing reports Linkages to individual state reporting and inspection results CMS raised the bar, now SNFs return to work of quality improvement Outline of a strategy for improving your Five Star rating: Decrease survey score (frequency of tags weighted by scope and severity) o Monitor deficiencies (Trend Tracker) o Implement strategies to reduce them o Must be consistent, as survey score is 3-year average Increase RN and DCS staffing o Monitor staffing (LTC Trend Tracker) o Implement strategies to increase PPDs (see the Trend Tracker Five Star staffing predictor) Improve the 11 QMs o Monitor QMs (LTC Trend Tracker) o Implement strategies to improve them (see the Trend Tracker Five Star QM predictor) o Also must be consistent, as there is roughly a 6 month delay before appearing in Nursing Home Compare, and most measures are based on 12 months of data. So sustain improvement for at least 18 months. Also decrease rehospitalizations and increase discharge to community rates, as they will be added to Five Star QM component in 2016 The full list of elements to target in your Five Star strategy… Benefits of Joining the National PSO for AL Access to data For benchmarking Detect and address emerging quality issues as they arise For the AHCA/NCAL Quality Award Program Reduce liability costs and exposures Access to resources including webinars, policies & procedures, and training material to improve quality Improve safety and quality, leading to better resident outcomes www.ncalpso.org What Data Does the PSO Collect? Demographics Falls Pain Management Pressure Ulcers Infection Control Unplanned Hospitalizations Hospice Elopements Depression Medication Management www.ncalpso.org You Have Data…now what? How to Use Data As part of Root Cause Analysis (RCA) Quality Assurance & Quality/Performance Improvement (QAPI) PDSA – Plan, Do, Study, Act Referral programs/working with other providers Marketing Resident/Family/Staff Satisfaction What is your data telling you? 1. Demonstrate good clinical care/outcomes? 2. Low readmission rates? 3. Excellent customer experience scores? 4. Staff stability? Share your outcomes Share outcomes with staff, residents and families Show progress in the break room Talk about outcomes at meetings, resident and family council Share with other providers Setting Your Goals Make it a SMART goal Specific – reduce Rehospitalization by 10% Measurable – current turnover (X%) a 10% decrease is (X%) Achievable – can your center do this? Do you have support? What can you do to make it achievable Realistic – think about everything else going on in your center, setting up goals that are not realistic is setting your center up for failure which is counter-productive Time-targeted – by 12/31/2015 Setting Goals EXAMPLE Goal 1 (remember SMART): Goal- Reduce Rehospitalization Measurable – Reduce Rehospitalization by 10 Time frame: by 7/23/2016 Activities to support this goal 1. Implement Interact tool 2. Identify trends for improvement when are the most readmissions to the hospital? 3. Train Staff and Physicians 4. Develop protocols for readmissions 5. Implement program by October 31, 2015 Quality Improvement: PDSA Plan Do Study Act (PDSA) Commonly used quality improvement tool Others include Root Cause Analysis (5 Whys) Flow Charts Many others! Can utilize with any quality improvement project PDSA: Plan Step 1: Plan Plan the test or observation, including a plan for collecting data. State the objective of the test. Make predictions about what will happen and why. Develop a plan to test the change. (Who? What? When? Where? What data need to be collected?) From the Institute for Healthcare Improvement http://www.ihi.org/resources/Pages/HowtoImprove/ScienceofImprovementTestingChanges.aspx PDSA: Do Step 2: Do Try out the test on a small scale. Carry out the test. Document problems and unexpected observations. Begin analysis of the data. From the Institute for Healthcare Improvement http://www.ihi.org/resources/Pages/HowtoImprove/ScienceofImprovementTestingChanges.aspx PDSA: Study Step 3: Study Set aside time to analyze the data and study the results. Complete the analysis of the data. Compare the data to your predictions. Summarize and reflect on what was learned. From the Institute for Healthcare Improvement http://www.ihi.org/resources/Pages/HowtoImprove/ScienceofImprovementTestingChanges.aspx PDSA: Act Step 4: Act Refine the change, based on what was learned from the test. Determine what modifications should be made. Prepare a plan for the next test. From the Institute for Healthcare Improvement http://www.ihi.org/resources/Pages/HowtoImprove/ScienceofImprovementTestingChanges.aspx What you can do Embrace Value Based Purchasing Programs – they allow you more control over your payment Embrace data and the feedback it provides The details matter – learn the details of each proposed measure and train your staff Keep an open mind as you perform root cause analysis Establish a common goal within your center When you get back Look at Rehospitalization rates, implement INTERACT Review your Five Star Rating Use your clinical systems and root cause analysis to make changes MDS Process Use Free Tools such as Advancing Excellence or LTC Trend Tracker. Questions