Expanding community eye care for glaucoma : a pilot Ophthalmic
advertisement

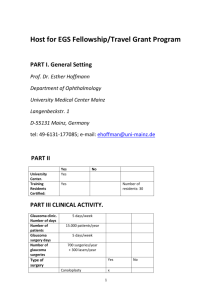
RNIB – supporting people with sight loss Research briefing Expanding community eye care for glaucoma: a pilot Ophthalmic Diagnostic and Treatment Centre Author: Helen Lee; Publisher: RNIB; Year of Publication: 2015 Key findings from the evaluation With the successful implementation of an optometry-led Ophthalmic Diagnostic and Treatment Centre (ODTC) for glaucoma: Waiting times between appointments were reduced. The hospital rescheduled fewer appointments in general ophthalmology outpatient clinics. Although one in four appointments at the ODTC were rescheduled adding, on average, 29 days between appointments. Patient satisfaction with the ODTC was almost universal. The lack of readily available routine data with which to identify glaucoma patients and their appointment activity presented challenges to the evaluation of the pilot. The actual cost of the ODTC pilot was £291.56 per patient seen; this includes significant staff training costs. Without training costs, and assuming the ODTC was to operate at full capacity with no DNAs (did not attend) the cost would be £122.48 per patient. Background Glaucoma is the second most common cause of certified sight loss in the UK. 3,291 people in England and 192 people in Wales aged over 40 were certified as visually impaired due to glaucoma, between 1st April 2012 and 31st March 2013 (1). With early detection and treatment of ocular hypertension and glaucoma visual field loss can often be prevented or minimized. There is an RNIB charity numbers 226227, SC039 316 and 1109 association between people experiencing high rates of socioeconomic deprivation and presenting in health care settings with advanced glaucoma (2, 3, 4, 5). There is increasing demand on ophthalmology departments but without increasing resource this has led to a serious problem of lack of capacity. This has resulted in follow-up appointments being delayed and many incidences of patients not receiving appropriate treatment in a timely fashion (6). Recent research conducted for RNIB Cymru found Consultant Ophthalmologists in six Welsh Health Boards stating that patients are losing their sight due to excessive waiting times (7). In 2011 RNIB began work with Cwm Taf Health Board in South Wales to explore barriers to accessing eye care services and identify potential interventions to prevent avoidable sight loss. Public Health Wales conducted an eye health equity profile (8) and Shared Intelligence undertook qualitative research with service users and service providers (9). Informed by these pieces of work it was agreed that RNIB and Cwm Taf Health Board would work in partnership to pilot a new service for people with ocular hypertension and ‘stable’ glaucoma. The service is called an Ophthalmic Diagnostic and Treatment Centre (ODTC). The development and implementation of ODTCs to help manage capacity issues within ophthalmology departments and improve the patient pathway is central to the Welsh Government’s, five year Eye Health Care Delivery Plan (2013). This pilot project was designed to gather learning prior to the roll out of ODTCs; to consider patient flow, assess impact on quality of service, patient satisfaction, waiting times and attendance at both the ODCT and consultant led ophthalmology clinics. Methods The Ophthalmic Diagnostic and Treatment Centre (ODTC) was designed to provide a service for people aged over 40 living in a rnib.org.uk particular area of high socioeconomic deprivation within the Rhondda Valley. The ODTC aimed to: Reduce waiting times for the management of people with stable glaucoma and ocular hypertension. Improve patient satisfaction offering a more flexible service closer to home. Improve service uptake and reduce non-attendance at secondary care glaucoma clinics. The service was located in a local community hospital and was originally designed to be led by a specialist nurse managing a team of technicians, seeing patients with ‘stable’ glaucoma and ocular hypertension. Patients with ‘stable’ glaucoma refers to those who, for a period of two years have: experienced no new symptoms which could be attributable to progressive visual deterioration (such as a drop in acuity or subjective change of a paracentral visual field defect); intraocular pressure remaining below a level satisfactory for the individual patient; no change in the optic disc appearance; and no significant change in visual field. Over the period of implementation the service evolved to be optometry-led, seeing patients with suspect, stable and ‘simple’ glaucoma and ocular hypertension. More information about the changes in staffing are provided in the process evaluation section of this briefing. ‘Simple’ glaucoma refers to patients who do not require consultant care (unlike complex cases) but may not have been ‘stable’ for two years. The service was nurse-led from July 2012 to June 2013; in July 2013 it became optometrist led. Evaluation data was collected until mid November 2014. Cwm Taf Health Board has continued to fund the ODTC beyond the lifetime of the pilot project. London School of Hygiene and Tropical Medicine (LSHTM) conducted independent process, outcome and economic rnib.org.uk evaluation of the pilot. There were five components of the evaluation: 1. Analysis of routine hospital data 2. Patient satisfaction surveys conducted before and after the introduction of the new services 3. Follow-up interviews with patients attending the ODTC 4. Process interviews with key people involved in the development, implementation and delivery of the ODTC 5. A cost consequence analysis. The evaluation included a comparison group of patients with ‘stable’ or ‘simple’ glaucoma living in the Cynon Valley and using ophthalmology services in various local hospitals. The evaluation was granted NHS ethical approval from Bromley Research Ethics Committee (11/LO/1264) and local Research & Development (R&D) office approval from Cwm Taf Health Board (CT/214/80513/11/12). Findings from analysis of routine data For baseline data appointment activity of 1,429 patients was analysed for a minimum of one year prior to the opening of the ODTC. One third of patients (435/1,429) were from the intervention area. For the follow up period, once the ODTC was operating as an optometry-led, appointment data for 1,412 patients was analysed. As at baseline nearly a third of patients were from the intervention site (421/1,421). At baseline: The mean interval between appointments (excluding new referrals) was 160 days. The average waiting time between appointments was significantly longer for people from the intervention area. People in the intervention area waited on average 208 days compared rnib.org.uk to those from the comparison site who waited on average 137 days. Over one in five follow-up appointments were rescheduled by the hospital (23%) adding on average 48 days to the interval between appointments. Newly referred patients did not experience rescheduling of appointments to the same extent as continuing patients, which may be related to performance targets. Only 5% of patients did not attend (DNA) their ophthalmology outpatient appointment. At follow up: The mean number of days between appointments for patients from the intervention area reduced 208 days to 126 days for those seen at the non-ODTC clinics and 111 days for those seen at the ODTC. There was no longer a significant difference in waiting times between appointments for patients from the intervention and comparison areas. Rescheduling of appointments at non-ODTC clinics was reduced to 10% (compared to 23% at baseline) adding an average of 53 days to the interval between appointments. However, 25% of appointments were rescheduled for patients attending the ODTC. On average extending the interval between appointments by 29 days. Only 4.6% of patients did not attend (DNA) at the ODTC clinic and 3.6% of non-ODTC clinics. At the same time as the ODTC was established the general ophthalmology outpatient clinics were reorganised. The table below summarises this information. Measure At baseline At follow up Non-ODTC ODTC clinics The mean interval 160 days 126 days 111 days rnib.org.uk between appointments Appointments 23% cancelled by the hospital Extra days added 48 days due to hospital rescheduling Patient did not attend 5% (DNA) 10% 25% 53 days 29 days 4% 5% The lack of readily available routine data with which to identify glaucoma patients and their appointment activity presented challenges to the evaluation of the pilot. It is also likely to inhibit effective service planning. At the outset of the project it was assumed non attendance by patients (DNAs) was a significant problem that the ODTC would help to address. Once the independent evaluators LSHTM had analysed hospital data it became apparent that DNAs were at such a low level there was little room for improvement; however hospital initiated cancellation were a significant problem. Findings from the patient satisfaction survey At baseline: 86 usable questionnaires were completed by glaucoma patients attending general ophthalmology clinics; 24 were from the intervention area and 59 from the comparison site. 66% of patients thought it important to see a doctor. 48% of patients were shown how to administer their eye drops. At follow up: 112 useable questionnaires were completed, 53 from ODTC and 59 from the general ophthalmology clinic. Patients at the ODTC travelled less distance, were less likely to use a car and incurred less travel costs. rnib.org.uk Only 26% felt it important to see a doctor compared to 66% at baseline. In response to an open question, patients most commonly reported that they didn’t mind who they saw as long as “they know what they are doing”; “are qualified”; “properly trained”; and “know their job”. ODTC patients were younger than those seen elsewhere and a lower proportion reported co-morbidities. Fewer ODTC patients reported being ‘bothered’ by their treatment. 50% of ODTC patients reported being shown how to use their drops and 71% of patients in general ophthalmology clinics compared to 48% of patients at baseline. The table below summarises this information. Measure At baseline At follow up NonODTC clinics Usable questionnaires 86 59 Felt it important to see 66% 43% a doctor Shown how to 48% 71% administer eye drops ODTC 53 26% 50% Process evaluation Staffing and tests Telephone interviews were conducted with six staff members involved in developing and implementing the ODTC. It was originally intended that that ODTC in the Rhondda Valley would be led by a specialist nurse, supported by two Band 3 ophthalmic technicians. The nurse would provide: Patients with advice about treatment adherence. Visual fields interpretation. rnib.org.uk Optic disc assessment. Stereo-disc photography. The ophthalmic technicians would conduct: Visual acuity (Snellen). Visual fields (field of vision). Pachymetry (thickness of the cornea). Goldmann applanation tonometry (inner eye pressure). Pharmacological dilatation of the pupils (shape and appearance of the optic nerve). However, a number of challenges emerged with this arrangement. Most importantly perhaps it was realised that the lead person needed more diagnostic expertise if the ODTC was to save time and provide efficiencies. The rural location of the Rhondda Valley ODTC was found to be one of the major reasons why a nurse-led model did not prove suitable. The ODTC was not located close to a specialist ophthalmology- led clinic, so if any concerns emerged, it was not possible for staff to easily ask the consultant to assess and advise, or simply redirect the patient from the ODTC back into the general clinic, without additional appointments. During the pilot phase the ODTC was not linked to ophthalmology practitioners electronically. In the absence of specialist training pathways for nurses in this field, the development of the necessary expertise relied on learning through experience ‘on the job’. The lack of sufficiently specialist skills, combined with the lack of electronic/digital facilities to share data, necessitated referring patients from the ODTC back into the hospital system for a second opinion. While this was essential for the safety and well-being of patients, it undermined one of the original aims: namely to reduce the necessity for patients to attend the hospital out-patient clinics. Therefore a decision was made to appoint two part-time optometrists in place of the specialist nurse to lead a team of ophthalmic technicians. In preparation for leading the ODTC the rnib.org.uk optometrists worked alongside the consultant ophthalmologist for several months. The optometrists competency for seeing patients within the ODTC was established by competency based supervised practice, working alongside the consultant ophthalmologist in his general clinic prior to starting in ODTC. Once deemed competent, the consultant would review the notes of the patients seen on a weekly basis. There is no national EPR available, therefore the consultant would review the notes, visual fields and 3D images the following day prior to starting his own clinic. Any discrepancies between findings and decision making were highlighted to the optometrist. In addition to this, patients who showed deterioration of their visual field, disc appearance or control of inter-ocular pressure at the ODTC were booked back into the consultant led clinic. Therefore review of ODTC findings also happened as part of the process of clinicians reviewing patient’s notes prior to seeing a patient. Consultant support was available for the ODTC provided by non glaucoma consultant led clinics running alongside the ODTC and specialist Glaucoma advice was available by telephone from the District General Hospital. With two optometrists working in the clinic, interoptometry peer support and review was available between staff. Within the ODTC the optometrists provided advice to patients about treatment adherence, examined patients, reviewed their conditions, analysed the results of the tests conducted by technicians and prescribed, advised, or referred accordingly. If optometrists noted some concerns, such as the deterioration of a patient’s condition, but felt these were not major enough to warrant a referral to the hospital, they could make another appointment sooner than they would routinely and so keep the patient under closer review. If, for example, a cataract was detected, the optometrists could refer the patient directly for an operation without the patient having to be seen in the ophthalmologist’s clinic first for a referral to surgery. They also undertook gonioscopy tests (to assess the angle in the eye where the iris meets the cornea). rnib.org.uk There was not consensus about whether a remotely based ODTC needs to be led by an optometrist or a specialist nurse but rather a strong feeling the lead health professional requires specialist training to ensure they have the necessary insight, experience and diagnostic skills. The ODTC enabled patients to have additional tests during a single visit. Previously patients would have attended a separate clinic for a visual field test. Criteria for seeing patients: stable or simple glaucoma The original intention was that the ODTC would see patients with stable glaucoma. However it became apparent that in practice this was not a reliable basis for selection, as any such diagnosis or conclusion can quickly become out of date. So when the service became optometry-led the criteria for selecting patients was revised, from ‘stable’ to ’simple’, meaning that most patients with glaucoma and OHT in the geographical catchment area aged who were aged over 40 effectively became eligible. Patient perspective In-depth interviews were conducted with twelve patients attending the ODTC. Most were unaware of the type of professional they saw, for example, ‘Mr A’s deputy’, ‘specialist nurse’, ‘a nice young man’. Patients’ main concern was that the health professional was someone who ‘knows what they’re doing’. Patients who had previously attended the Royal Glamorgan Hospital were asked if they had experienced hospital initiated cancellation of appointments. Several had, and they described it as happening frequently and often the rescheduled appointment was also cancelled. Feelings about this were mixed. Some people did not see it as a problem if the appointment is quickly rescheduled. However one patient described being concerned about the high rnib.org.uk pressure in her eyes as she was due to be seen in six months but ended up waiting twelve months before being seen. Patients were asked about their experience of time spent with staff and information provided at the ODTC as compared to the general ophthalmology clinic. However they were not able to comment on any differences. It is probable that patients will have to attend fewer appointments at the ODTC compared to attending ophthalmology outpatient clinics because visual field tests are conducted during the one appointment alongside other tests and examinations. Economic evaluation The actual cost of the ODTC pilot was £291.56 per patient; this includes significant staff training costs. The cost of running an ongoing ODTC service without including initial staff training costs, assuming 85% capacity and 5% DNAs would be £186.91. If the ODTC was operating at full capacity without training costs and assuming no DNAs the cost would be £122.48 per patient. Conclusion The pilot ODTC in the Rhondda Valley has resulted in reduced waiting times between appointments for patients. Patient satisfaction was near universal, and patients from the Rhondda seen at the ODTC travelled less distance, were less likely to travel by car and incurred less cost than patients from the intervention area seen at other clinics. Patients attending the ODTC generally had to attend fewer appointments compared to those attending consultant led ophthalmology outpatient clinics. This is because at the ODTC visual field tests were conducted during the one appointment alongside other tests and examinations. The increased capacity that the ODTC provides appears to have had a positive effect on general ophthalmology clinics in that a rnib.org.uk lower proportion of patients experience hospital initiated rescheduling of appointments. However rescheduling of appointments at the ODTC was significant. Recommendations 1. Disseminate learning from this pilot project across Wales and the rest of the UK to inform the development of eye care service delivery, to help increase capacity within glaucoma clinics and therefore ensure patients’ receive timely treatment. 2. Our pilot indicated that Ophthalmic Diagnostic and Treatment Centres (ODTC) can be led by a range of eye health professionals including ophthalmic nurses or optometrists. It is however essential these professionals receive specialist training to ensure they have appropriate expertise and diagnostic skills. 3. Hospital data about attendance at glaucoma ophthalmology outpatient clinics improved over the lifetime of the project. It is essential that detailed, accurate and update information is available on attendance and outcomes from outpatient ophthalmology clinics to monitor and evaluate the impact of services and enable effective service planning. 4. Adherence to treatment for glaucoma and ocular hypertension can be problematic for patients, changes in lifestyle, co-morbidities etc effect people’s ability to comply with treatment regimes. It is therefore recommended that treatment adherence is routinely discussed with patients in all glaucoma clinics. 5. It became apparent through this pilot study that hospital initiated rescheduling of appointments was a significant issue in both consultant led ophthalmology clinics and the ODTC. This is problematic for patient care and increases the risk of patients being ‘lost’ in the system. It is recommended that examples of good practice are identified where ophthalmology services have reduced rescheduling of rnib.org.uk appointments and these are shared throughout the UK to improve patient care. References (1) Leamon, S., Davies, M., (2014) Number of adults and children certified with sight impairment and severe sight impairment in England and Wales: April 2012 to March 2013. RNIB (2) R., Wood, F., (2010) A glaucoma equity profile: correlating disease distribution with service provision and uptake in a population in Northern England, UK. Eye 24:1478-85 (3) Fraser, S., Bunce, C., Wormald, R., Brunner, E. (2001) Deprivation and late presentation of glaucoma: case-control study. Br Med J 322:639-43 (4) Ng, W.S., Agarwal, P.K., Sidiki, S., McKay, L., Townend, J., Azuara-Blanco, A., (2010) The effect of socio-economic deprivation on severity of glaucoma at presentation. Br J Ophthalmol 94:85-7 (5) Sukumar, S., Spencer, F., Fenerty, C., Harper, R., Henson, D., (2009) The influence of socioeconomic and clinical factors upon the presenting visual field status of patients with glaucoma. Eye 23:1038-44 (6) National Patient Safety Agency (2009) Rapid Response Report. Preventing delay to follow up for patients with glaucoma. NHS National Patient Safety Agency. (7) Boyce, T., (2014) Real patients coming to real harm. Ophthalmology services in Wales. RNIB Cymru (8) Reilly, R., Humphreys, C., (2011) Cwm Taf Eye Health Equity Profile. Public Health Wales NHS Trust http://www.wales.nhs.uk/sitesplus/922/page/49905 (accessed 15/7/15) (9) Richardson, I., (2012) The barriers and enablers that affect access to primary and secondary eye care services – Cwm Taf site report. RNIB rnib.org.uk End of document rnib.org.uk