Response to reviewer 2 (John Belisle)
advertisement

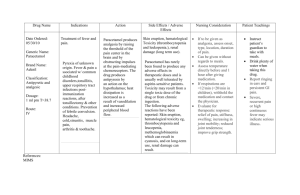
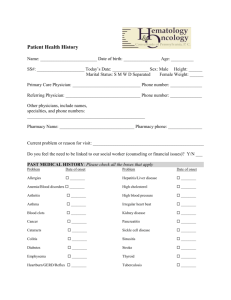
Response to reviewer 2 (John Belisle) Dear Reviewer, Thank you very much for all the comments and suggestions which were very important to improve the manuscript entitled “Effect of anti-tuberculosis drugs on hematological profiles of tuberculosis patients attending at University of Gondar Hospital, Northwest Ethiopia”. All the comments were considered important and here below is our point-by point response. We also want to assure you that all the response documented here are also incorporated in the manuscript. At this time, we believe that we made the manuscript within the standard requirements of the BMC hematology. All the bests! Baye Gelaw Tarekegn (PhD), corresponding author Response No 1: The use of healthy controls in the study At the beginning of this investigation, the hematological parameters of all smear positive TB patients were determined prior the initiation of the anti-TB drugs. At this point, all the study subjects were treatment free which is considered as a base line data. Then after completion of the intensive phase of tuberculosis treatment (2 months), the hematological parameter of each patient was also determined. Because the aim was to evaluate the effect of the anti-TB drugs on hematological parameters of TB patients, we did not used health controls as these controls will not tell us the effect of the anti-TB drugs because they are treatment free. Response No 1: The effect of host process to clear the bacteria versus the effect of anti-TB drugs on hematological parameters In this study, the hematological parameters of TB patients determined prior anti-TB drug initiation and after completion of the intensive phase of treatment was investigated. We are assuming that hematological parameters of TB patients would have been remained relatively similar if patients were not treated with anti-TB drugs because tuberculosis is a chronic disease whose effect is very gradual. Moreover, the only well known permissive cell that host the TB bacilli in the lung is the macrophage which have very lower proportion in the peripheral blood on which hematological parameters are determined. We understand that the immune response after initiation of anti-TB drugs could have got some strength because the bacillary load is decreasing as a result of the anti-TB drugs. However, at this point we are expecting that the contribution of the anti-TB drug in killing the TB bacilli will be by far higher than the immune response and because of that we evaluated the effect of the anti-TB drugs on hematological profiles in comparison with that of treatment naïve but the same cases. Major compulsory concern: demographic data We used age and sex as demographic characteristics valuable in this study because hematological parameters reference values are always determined based on age and sex of individuals. As the aim of this study was to determine the effect of anti-TB drug on hematological parameters, we considered that demographic characteristics other than age and sex have only little significance. Hence, we did not consider other demographic characteristics to compare hematological parameters versus TB treatment. However, the association of age and sex with that of hematological parameters was analyzed and documented in table 1 in the revised version of this manuscript. Minor essential comments 1. Abbreviations in the abstract: The RDW and PDW documented in the abstract are defined---Thanks. 2. Method to confirm M. tuberculosis infection: This comment was found very important and we incorporated the method we used to detect the tubercle bacilli in sputum which was Ziehl-Neelsen staining method---Thank you very much once again. 3. Quality control measures: The quality control measures we used are also re-organized and all the activities conducted during this study as quality control measures are documented currently---again many thanks. 4. Terms such as slightly lower and higher and p value=0.000: We used these terms when we got differences but not statistically significant. However, we tried to minimize and avoid repetitions. A p-value of 0.000 means strongly associated but p-value of .000 is actually a mistake and corrected as “0.000”. Currently variables that are significantly associated are indicated by “ ”٭in both table 2 and 3. 5. Medical significance of the study findings The significance of the findings such as reduced Hgb, HCT, platelate, PDW together with the increased RDW are reflected on the last part of our discussion 6. Editorial error: We tried to edit the manuscript as much as possible and we are hoping that errors are minimized by now. 7. Burden of acid-fast bacilli versus hematological parameters: We are conscious enough that tuberculosis may have some effect on hematological parameters and the AFB score could also contribute to some extent. However, as the tubercle bacillus accumulates in the lungs and there are very rare or probably no cases of envision of the circulatory system, the effect of the TB bacilli on hematological parameters by itself can be considered minimum or negligible. This is evidenced by almost always negative blood culture taken from TB patients which is reported by different articles. Moreover, we have known that the lymphatic system is the major route for tubercle bacilli to migrate to different parts of the host and also to the lungs. Therefore, we are still conscious that the burden of TB bacilli may not have direct influence on hematological parameters and that is why we focused on the anti-TB drugs. the most important