B2B-Personality Disorders 2013.Dr M Mathias
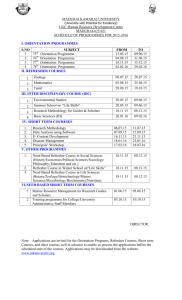
advertisement

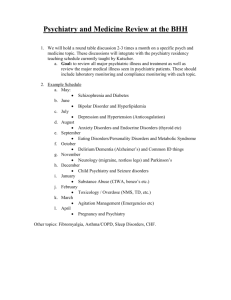
B2B: Personality Disorders Michelle Mathias, MA, MD, FRCPC April 3, 2013 Special thanks… … to Dr. Deanna Mercer Objectives General: Differentiate between PD and other mental illness, recognizing the high prevalence of comorbidities Formulate appropriate management plan Objectives Specific: List & interpret critical clinical findings, inc: Sufficient clinical info (e.g. MSE) to dx type of PD Risk factors associated with PDs (e.g. SI, substance) Any co-existing psych conditions (e.g. mood d/o) Construct an effective initial management plan, inc: Proper management for pt needing immediate intervention (e.g. suicide risk, risk to others) Judicious use of pharmacotherapy, with consideration of risk for abuse or overdose Referral for multi-disciplinary and/or specialized care, if needed 2-pass approach Criteria/overview objective/detailed By B2B… PDs from the start …definitions & diagnostic criteria! Definitions Personality: Individual’s characteristic pattern of response to his/her enviro Includes: how one… Thinks (cognitive) Feels (affective) Acts (behavioural) Relates to others (interpersonal) Etiology: transactional model Temperament (bio) + Environmental (social) time Definitions (cont’d) Personality Disorders: Clinically significant distress or impairment in functioning Enduring pattern of inner experience and behaviour that deviates markedly from expectations of individual’s culture Impacts: 2 or more cognition, affectivity, interpersonal fxn & impulse control Pattern: Inflexible & pervasive across broad range of personal and social situations Not better accounted for by other mental disorder, GMC or substance Definitions (cont’d) Personality Disorders: Ego-syntonic: Individual experiences sig distress, but doesn’t feel their thoughts, emotions or behaviors are source of their problem Locus of control: external E.g. OCPD VS Ego-dystonic: Individual sees their disorder as arising from their own thoughts, emotions or behaviours Locus of control: internal E.g. OCD Definitions (cont’d) Personality Disorder Clusters: 3-4-3 Cluster A: ODD Schizoid, Schizotypal, Paranoid Cluster B: Dramatic Borderline, Histrionic, Narcissistic, Antisocial Cluster C: Anxious Obsessive Compulsive, Dependent, Avoidant Cluster A Paranoid, Schizoid, Schizotypal Paranoid PD Pervasive pattern of: Distrust and suspiciousness of others Motives of others are interpreted as malevolent … beginning by early adulthood and present in various settings Practically: Looks like delusional d/o (paranoid type), but No full blown delusions More pervasive suspiciousness Schizoid PD Pervasive pattern of: Detachment from social relationships Restricted range of expression of emotions in interpersonal settings … beginning by early adulthood and present in various settings Practically: Mostly solitary activities Few friends other than first degree Cold & detached Little or no interest in relations; solitary lifestyle Indifferent to praise or criticism Schizotypal PD Pervasive pattern of: Social and interpersonal deficits Acute discomfort with and reduced capacity for close relationships Cognitive or perceptual distortions or eccentricities of behaviour … beginning by early adulthood and present in various settings Practically: Eccentric behaviours Odd beliefs, unusual perceptions, suspiciousness, paranoia, odd speech Discomfort in close relationships - paranoia (not b/c of fear of judgment) Flashback… (-) sx Cog sx (+) sx Schizophrenia Flashback… (-) sx Cog sx (+) sx Schizo Schizophrenia ypal Flashback… (-) sx Devoid… Schizoid Cog sx (+) sx Schizo Schizophrenia ypal Cluster B Antisocial, Borderline, Histrionic, Narcissistic Antisocial PD Pervasive pattern of: Disregard for and violation of rights of others … since age of 15 (must be at least 18yo) Practically: Repeated lawbreaking Deceitfulness Impulsivity Irritability and aggressiveness Disregard for safety of self or others Consistent irresponsibility Lack of remorse Borderline PD Borderline PD Pervasive pattern of: Instability of interpersonal relationships Instability of self-image and affects Marked impulsivity … beginning by early adulthood and present in various contexts Practically: Efforts to self-harm or end life Unstable relationships Mood lability Histrionic PD Pervasive pattern of: Excessive emotionality Attention seeking … beginning by early adulthood and present in various settings Practically: Theatrical Intense but shallow emotions Craves being centre of attention Narcissistic PD Pervasive pattern of: Grandiosity (in fantasy or behaviour) Need for admiration Lack of empathy … beginning by early adulthood and present in various contexts Cluster C Avoidant, Dependent, Obsessive Compulsive Avoidant PD Pervasive pattern of Social inhibition Feelings of inadequacy Hypersensitivity to negative evaluation … beginning by early adult and present in various contexts Practically: Similar to social phobia, but more pervasive Dependent PD Pervasive and excessive need to be taken care of, leads to: Submissive and clinging behaviour Fears of separation … beginning by early adult and present in various contexts Practically: Dependent on relationships Difficulty making everyday decisions without a lot of advice, reassurance from others Unable to disagree with others because fears loss of support Will do things that are unpleasant, degrading to maintain support Obsessive Compulsive PD Pervasive pattern of preoccupation with: Orderliness Perfectionism Mental and interpersonal control … at the expense of flexibility, openness and efficiency … beginning by early adult and present in various contexts Practically: Controlling of others, inflexible Excessively devoted to work Reluctant to delegate tasks Emotionally constricted 2-pass approach Criteria/overview objective/detailed By Objectives Specific: List & interpret critical clinical findings, inc: Sufficient clinical info (e.g. MSE) to dx type of PD Risk factors associated with PDs (e.g. SI, substance) Any co-existing psych conditions (e.g. mood d/o) Construct an effective initial management plan, inc: Proper management for pt needing immediate intervention (e.g. suicide risk, risk to others) Judicious use of pharmacotherapy, with consideration of risk for abuse or overdose Referral for multi-disciplinary and/or specialized care, if needed Objectives Specific: List & interpret critical clinical findings, inc: Criteria (done) & MSE Risk factors associated with PDs (e.g. SI, substance) Any co-existing psych conditions (e.g. mood d/o) Construct an effective initial management plan, inc: Proper management for pt needing immediate intervention (e.g. suicide risk, risk to others) Judicious use of pharmacotherapy, with consideration of risk for abuse or overdose Referral for multi-disciplinary and/or specialized care, if needed Objectives Specific: List & interpret critical clinical findings, inc: MSE Risk factors & prognosis Any co-existing psych conditions (e.g. mood d/o) Construct an effective initial management plan, inc: Proper management for pt needing immediate intervention (e.g. suicide risk, risk to others) Judicious use of pharmacotherapy, with consideration of risk for abuse or overdose Referral for multi-disciplinary and/or specialized care, if needed Objectives Specific: List & interpret critical clinical findings, inc: MSE Risk factors & prognosis Comorbidities Construct an effective initial management plan, inc: Proper management for pt needing immediate intervention (e.g. suicide risk, risk to others) Judicious use of pharmacotherapy, with consideration of risk for abuse or overdose Referral for multi-disciplinary and/or specialized care, if needed Objectives Specific: List & interpret critical clinical findings, inc: MSE Risk factors & prognosis Comorbidities Construct an effective initial management plan, inc: Risk assessment & acute management (safety) Judicious use of pharmacotherapy, with consideration of risk for abuse or overdose Referral for multi-disciplinary and/or specialized care, if needed Objectives Specific: List & interpret critical clinical findings, inc: MSE Risk factors & prognosis Comorbidities Construct an effective initial management plan, inc: Risk assessment & acute management (safety) Pharmacotherapy Referral for multi-disciplinary and/or specialized care, if needed Objectives Specific: List & interpret critical clinical findings, inc: MSE Risk factors & prognosis Comorbidities Construct an effective initial management plan, inc: Risk assessment & acute management (safety) Pharmacotherapy Non-pharm treatment Objectives List & interpret critical clinical findings, inc: MSE Risk factors & prognosis Comorbidities Construct an effective initial management plan, inc: Risk assessment & acute management (safety) Pharmacotherapy Non-pharm treatment General Word on Tx approach Bio Acute – safety (self & others) Short-term (stabilization) Long-term (maintenance) Psycho Social Cluster A Paranoid, Schizoid, Schizotypal Paranoid PD (refresher… which one is this?) MSE: evasive, minimal answers, suspicious, paranoid thought content, serious, humourless affectively restricted, lack warmth Risk factors & prognosis: Relatives often have Schizophrenia Lifelong problem working & living with others Comorbidities: Other cluster A PDs, mood disorder, substance use, agoraphobia, OCD Paranoid PD (refresher… which one is this?) Risk assessment & acute management (safety): Suicide attempters in ER: 9% with PPD Pharmacotherapy: Antidepressants as indicated Low dose antipsychotic for brief psychotic episodes (increased stress) Non-pharm treatment: Rarely seek help – insufficient trust to engage in process CBT – address core beliefs Group therapy – tend not to tolerate Schizoid PD (refresher… which one is this?) MSE: Cold, constricted, aloof, difficulty gaining rapport, odd metaphors, ill at ease, difficulty tolerating eye contact Risk factors & prognosis: Parents – cold, neglectful, suggest relationships not worth pursuing Introversion Possible family link – schizophrenia Childhood onset, likely stable course Comorbidities: other cluster A PDs, mood d/o, anxiety d/o Schizoid PD (refresher… which one is this?) Risk assessment & acute management (safety): Low insight, low motivation… not usually self-directed for tx Suicide attempters in ER: 4% Pharmacotherapy: Low-dose antipsychotic, antidepressants Non-pharm treatment: Psychoeducation Therapeutic distance needed for pt to tolerate relationship Social skills training Schizotypal PD (refresher… which one is this?) MSE: Superstitious, difficulty identifying own feelings, odd mannerisms and interests, prone to minimal responses (use open-ended questions), peculiar speech, appear unusual Risk factors & prognosis: 10% commit suicide; pre-morbid personality of schizophrenia (or milder version of); 10-20% develop schizophrenia 14% have schizophrenia in family Comorbidities: Other cluster A PDs, depression, possible Borderline PD traits (poor interpersonal relationships) Schizotypal PD (refresher… which one is this?) Risk assessment & acute management (safety): SI assessment; intensity of delusion-like beliefs Pharmacotherapy: Treat comorbidities Mild-mod improvement with low-dose antipsychotics Non-pharm treatment: Supportive psychotherapy Social skills training Encourage activity, but does not have to be social Cluster B Antisocial, Borderline, Histrionic, Narcissistic Antisocial PD (refresher… which one is this?) MSE: Try to impress MD, good verbal intelligence; possibly demanding Appear composed & credible (underneath = tension, hostility… may need to push to discover) Risk factors & prognosis: Px better if connected to some group Decrease impulsivity & criminal behaviour, but continue to be difficult people ++ substance risk; ++ legal involvement Comorbidities: Substance use disorders; other cluster B PDs, impulse control disorders, ADHD Antisocial PD (refresher… which one is this?) Risk assessment & acute management (safety): Harm to others!! Legal risk Pharmacotherapy: Mood stabilizers for impulsivity Stimulants for ADHD Tx comorbid depression, anxiety Non-pharm treatment: Firm limits Rational Emotive Therapy (CBT alternative) Psychoeducation Probation officers Borderline PD (refresher… which one is this?) MSE: Manipulation, splitting, inconsistencies, avoiding, deflecting, dramatic, poor problem solving, insight varies, poor judgment, thought process can vary and be significantly impaired in great distress Risk factors & prognosis: Abusive upbringing, substance use disorders Can decrease over time, but less so than other PDs Comorbidities: Other cluster B PDs, somatization disorders Mood disorders (BPD vs Bipolar), anxiety disorders (social anxiety) Brief psychotic episodes Substance use disorders Borderline PD (refresher… which one is this?) Risk assessment & acute management (safety): SAFETY!!! Self-harm, suicide attempts, aggressive acts towards others Hospitalization if needed… try to avoid DBT support; ACT teams Pharmacotherapy: Avoid TCAs (lethal in OD); SSRIs; mood stabilizers Antipsychotics for psychotic sx (derealization) Non-pharm treatment: DBT (modified CBT); individual + group Psychoeducation… give them the diagnosis! Psycho-analytic – NOT appropriate Social skills training Family & couples therapy Histrionic PD (refresher… which one is this?) MSE: Dramatic, temper tantrums, superficial (nil when go deeper), dramatic appearance (often sexual, esp clothing), eye contact varies Risk factors & prognosis: As age, sx decrease History of sexual abuse Substance use Comorbidities: Other cluster B PDs, brief psychotic episodes, somatization, DID Histrionic PD (refresher… which one is this?) Risk assessment & acute management (safety): Substance use Suicide attempts and ideation Heteroagressive ideation (“heat of passion”) Pharmacotherapy: Treat comorbidities: antidepressants (depression, anxiety, somatic complaints) Anti-psychotics: for derealization & illusions Non-pharm treatment: Psychoanalysis is ideal Insight-oriented Psychoeducation Family & couples therapy Narcissistic PD (refresher… which one is this?) MSE: Want their own way, no empathy, fake sympathy, superficial rapport; vague answers or avoiding Risk factors & prognosis: Substance use Upbringing with limited support and warmth Comorbidities: Substance use, mood disorders, anxiety disorders Other Cluster B PDs, sexual disorders Narcissistic PD (refresher… which one is this?) Risk assessment & acute management (safety): Rejection, loss, occupational problems, interpersonal problems Substance use Pharmacotherapy: Antidepressants Treat comorbidities (substance use disorders treatment) Non-pharm treatment: Insight-oriented therapy Probation officers Family & couples therapy Social skills training – learn how to develop empathic response for others Cluster C Avoidant, Dependent, Obsessive Compulsive Avoidant PD (refresher… which one is this?) MSE: Timid, lack self-confidence, afraid to speak, ++ anxiety during interview, hypersensitive to disapproval or rejection Do not express wishes, opinions, needs Risk factors & prognosis: Genetic link with social phobia Parents – inconsistent, absent, abusive, discouraging Comorbidities: Anxiety d/o (social phobia - generalized, agoraphobia) Depression, dysthymia Avoidant PD (refresher… which one is this?) Risk assessment & acute management (safety): Risk comes from associated anxiety and depression Risk of substance use – to cope with anxiety Pharmacotherapy: Treat comorbidities: anti-depressant Beta adrenergic receptor antagonists (Atenolol): decrease autonomic arousal Non-pharm treatment: Assertiveness & social skills CBT – core beliefs Mindfulness Dependent PD (refresher… which one is this?) MSE: Submissiveness; rapport is easy, but deeper exploration is difficult; easy to interview… want you to like them… watch for boundary violations Lack of self-confidence, pessimistic, helpless, childlike, ++ anxiety Risk factors & prognosis: Pts with chronic physical illnesses Can’t fxn independently; limited social relations Suicide risk: termination of Dependent relationship - Comorbidities: Mood disorders (MDD, adjustment d/o), anxiety disorders (social phobia, agoraphobia) BPD, histrionic PD, avoidant PD Dependent PD (refresher… which one is this?) Risk assessment & acute management (safety): Suicide risk, safety Isolation Pharmacotherapy: Treat comorbidities: anti-depressants Non-pharm treatment: Psychodynamic approach CBT Social skills training Family/ couples therapy OCPD (refresher… which one is this?) MSE: Stiff, formal, rigid demeanor, lack spontaneity; stickler for rules Detailed answers; constricted affect; eager to please (esp MD) Routine disturbed = anxiety; indecisive (fear of making mistake) Risk factors & prognosis: Parental control, perfectionism, shame, criticism Pressures can lead to mood & anxiety d/o… suicide concern Comorbidities: Other anxiety disorders Depressive disorders, dysthymia Vs OCPD (egodystonic): 30% OCPD have OCD (not same in reverse) NPD, Schizoid, somatoform d/o OCPD (refresher… which one is this?) Risk assessment & acute management (safety): Status of mood and anxiety Substance use – less prevalent (against rules; makes more anxious) Pharmacotherapy: Antidepressants Benzos… bad for anxiety disorders; some use short-term Non-pharm treatment: CBT… careful for the perfect homework! Psychoeducation Family & couples therapy Resources “Brain Calipers” “Field Guide to Disordered Personalities” (David Robinson, Rapid Psychler Press) Thank You … questions? comments? Michelle Mathias mmath051@uottawa.ca