Uniform Anatomical Gift Act Protecting the Decision
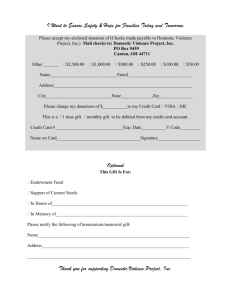
advertisement

Uniform Anatomical Gift Act Protecting the Decision SUZANNE A. FIDLER, M.D., J.D., CPHRM Senior Director of Risk Management Patient Safety Desert Regional Medical Center Objectives Understand the authority to make an anatomical gift. Review legal protections for organ and tissue donation. Explore how updating hospital policies and procedures based on current law support the donation process. Scenarios If a family objects to recovery of organs and/or tissues from a person who is listed in the donor registry, how will providers, OPOs, and the hospital respond? What if an advance directive and the decision to donate are incongruent? Does the hospital have a policy providing for administrative consent if unable to locate next of kin? Authorization for Organ and Tissue Donation Due to the disparity between the public support and the percentage of Americans actually donating Strong public policy to support organ and tissue transplantation Law provides authority and protection for providers, hospitals, and organ procurement organizations involved in donation. Uniform Anatomical Gift Act (UAGA) Promulgated in 1968 to provide national uniformity Drafted by the National Conference of Commissions of Uniform State Laws (NCCUSL) Amended in 1987 Revised in 2006 Majority of states have adopted Revised UAGA of 2006 Strengthens the rights of the individual and others to make an anatomical gift Retains the “opt-in” system that honors the free choice of an individual to donate Expands the list of persons who can make a gift Provides new definitions to clarify and expand the opportunities for anatomical gifts California Has Adopted the UAGA California Health & Safety Code Sections 7150-7151.40 May be cited as the California Uniform Anatomical Gift Act Based on the federal Uniform Anatomical Gift Act which is premised on gift law, not informed consent A Donor May Make an Anatomical Gift By indicating such on the donor’s driver’s license or identification card Directly through the Donate Life California Organ and Tissue Donor Registry Internet Web site In a will (takes effect upon donor’s death) During a terminal illness or injury by any form of communication that clearly expresses the donor’s wishes and addressed to at least 2 adults Full Faith and Credit from State to State A document of gift which is valid where executed is valid in another state. If the document of gift is valid based on the California UAGA, then California law governs the interpretation of the document of gift. A person may presume that a document of an anatomical gift is valid unless that person knows otherwise. CA Health & Safety Code Section 7150.85; UAGA Section 19 Purposes of the Anatomical Gift An anatomical gift of a donor’s body or part may be made for the purpose of: Transplantation Therapy Research, or Education Prioritizes Purposes of Gift If the purposes of the gift are not set forth in any priority, the gift shall be used for transplantation or therapy, if suitable; otherwise for research or education.* Example: if a person is in a donor registry for “all organs and tissues” without designation of purpose, the gift will be used first for transplant if suitable. *CA Health & Safety Code Section 7150.50(d); UAGA Section 11(f) Public Policy Favors the Making of Anatomical Gifts A presumption arises that the most comprehensive interpretation of the document of gift controls. There is no requirement that documents of gift be dated; purposely omitted to avoid invalidating documents of gift. Example: donor’s later-issued driver’s license is silent regarding licensee’s prior intent to make an anatomical gift. The gift on the prior license would still be effective. Others Barred from Amending or Revoking ***Absent an express, contrary indication by the donor, a person other than the donor is barred from making, amending or revoking an anatomical gift of a donor’s body or part if the donor made an anatomical gift. CA Health & Safety Code Section 7150.35(a); UAGA Section 8 A Donor’s Autonomous Decision Must be Honored Anatomical gift that the donor does not revoke before death is irrevocable. No permission from the donor’s family is warranted. The law firmly states that a donor’s decision to make an anatomical gift is not subject to change by others. The family does not have the power, right, or authority to consent to, amend, or revoke. Persons Authorized to Make an Anatomical Gift on Behalf of Decedent In the following order of priority for those persons reasonably available: (1) an agent of the decedent (2) the spouse or domestic partner (3) adult children (4) parents (5) adult siblings (6) adult grandchildren (7) grandparents Persons Authorized to Make an Anatomical Gift on Behalf of Decedent (8) An adult who exhibited special care and concern for the decedent (9) The persons who were acting as the guardians or conservators (10) Any other person having the authority to dispose of the decedent’s body, including but not limited to, a coroner, medical examiner, or hospital administrator , provided that reasonable effort has been made to locate and inform persons listed above. CA Health & Safety Code Section 7150.40(a); UAGA Section 9 Administrative Consent Supports hospital administration as a donation decision-maker in the event that no one is reasonably available to decide on behalf of the potential donor For these cases, hospitals have developed policies incorporating administrative consent where the hospital may be in a position to step in to potentially permit the gift of life. Person Authorizing the Donation May Expand the Gift A donor’s gift of a part for one purpose does not preclude another person from expanding the gift to include another purpose or part. Example: A donor signs a document of gift stating, “I give my liver for transplantation.” Following the donor’s death, an individual listed above may expand to include research or include the donor’s heart, unless the donor restricted the purposes of the gift or the part. Objection Based on Majority Rule Previous versions of UAGA provided that one person in a class could veto a gift (e.g., a single dissenting person has disrupted the donation process). Currently, if an objection is known, the gift can only be made by a majority of the members of the same class who are reasonably available. CA Health & Safety Code Section 7150.40(b); UAGA Section 9(b) “Reasonably Available” Known objections by persons not reasonably available do not bar persons who are reasonably available from making an anatomical gift. Defined as “able to be contacted by a procurement agency without undue efforts and willing and able to act in a timely manner consistent with existing medical criteria necessary for making anatomical gifts” * *CA Health & Safety Code Section 7150.10(a)(23); UAGA Section 2(23) “Reasonably Available” “Reasonably available” is not synonymous with physically present. Provides guidance to hospitals and OPOs in time sensitive situations. If a member in a higher class is unwilling to make a decision, that person is not reasonably available; this permits the ability to move down the priority list. Reasonable Search A reasonable search shall be conducted to locate a document of gift or other information identifying the individual as a donor or as an individual who made a refusal A reasonable effort shall be deemed to have been made when a search of the persons has been underway for at least 12 hours. The search shall include a check of local police missing persons records, examination of personal effects, and the questioning of any persons visiting the decedent before his or her death.* A person is not subject to criminal or civil liability for failing to discharge these duties but may be subject to administrative sanctions. ** * CA Health & Safety Code Section 7150.40(a)(10)(B); UAGA Section 12 ** CA Health & Safety Code Section 7050.55; UAGA Section 12 Karen Jacobsen and Hardy Jacobsen v. Marin General Hospital California case sent on appeal to the U.S. Court of Appeals for the Ninth Circuit, 1999. Martin Jacobsen, a Danish citizen, was visiting the U.S. and found by CHP unconscious along Highway 101. He had no identification, was presumed homeless, and no next of kin were identified. The OPO contacted the Marin County Coroner’s Office and requested donation. Jacobsen Case The coroner denied the request and initiated a 40- hour search for next of kin that included the FBI. No next of kin identified and Martin was declared brain dead. Coroner released the body for organ donation (kidney, liver, pancreas and heart were harvested). Jacobsen Case Martin’s parents, living in Denmark, were later located and they sued the hospital, network and coroner. The district court dismissed the case stating that the search was reasonable and that the defendants acted in compliance with the Gift Act. The Appeals Court upheld the ruling: (1) there was no duty for the hospital or network to also search for next of kin and (2) acted in good faith Medical Suitability The OPO may conduct any reasonable examination necessary to ensure the medical suitability. During the examination period, measures necessary to ensure the medical suitability of the part may not be withdrawn. CA Health & Safety Code Section 7150.65(c); UAGA Section 14 Advance Directives and Donation Situation where there is an advance directive instructing the withdrawal or withholding of lifesupport and consent for donation Requires that parties look toward the patient’s intent rather than assume an advanced directive to withdraw support automatically overrides the decision to donate. Potential Conflict Before resolution of the conflict, measures necessary to ensure the medical suitability of the part may not be withheld or withdrawn as long as not contraindicated by appropriate end-of-life care. When possible, the prospective donor (or agent) and attending shall confer to resolve the conflict. The conflict should be resolved as expeditiously as possible and collaborate with OPO. CA Health & Safety Code Section 7151.10(b); UAGA Section 21(b) Revocation and Amendments A donor may revoke or amend an anatomical gift by signing a record or directing another individual to do so. A donor’s revocation of an anatomical gift does not bar another authorized person from making an anatomical gift before or after the donor’s death; a donor who wishes to bind others to a revocation must sign a refusal. Refusal: a record that expressly states an intent to bar other persons from making an anatomical gift of an individual’s body or part. CA Health & Safety Code Section 7150.35(b); UAGA Section 6 Family Consent Practices The UAGA has always authorized an adult to “gift” organs and tissues without requiring family consent or permitting family to override that gift. However, fear of litigation and negative publicity have driven the practice of obtaining family consent. No reported cases of a family successfully suing healthcare or donation professionals where an individual had made a valid donation. Legal Immunity Professionals who act in good faith Not liable in a civil action, criminal prosecution, or administrative proceeding* Courts have upheld this protection Kelly-Nevils v. Detroit Receiving Hosp. (Mich. 1995) Nicoletta v. Rochester Eye & Human Parts Bank, Inc. (New York 1987) Carey v. New England Organ Bank (Mass. 2006) *CA Health & Safety Code Section 7150.80 UAGA Section 18 Kelly-Nevils v. Detroit Receiving Hospital Unidentified man with a gunshot wound to the head was admitted to the hospital. The hospital solicited an organ donation consent from a young man identifying himself as the brother and only living relative but did not verify the man’s identity. Police located the mother 3 days after the patient’s death; he had no brother. Kelly-Nevils Court Ruling There was no duty on the hospital to conduct an independent investigation to determine whether the young man had authority. No one had notified the hospital of any opposition to the organ donation. The court concluded that to impose any duty of investigation would frustrate the purpose of the UAGA since “time is of the essence.” Nicoletta v. Rochester Eye and Human Parts Bank Peter Nicoletta was injured in a motorcycle accident and a woman identified herself as the wife and signed the chart as “Judy Shufelt” with “wife” in parenthesis. Several hours later she signed paperwork to donate the organs as “Judy Nicoletta” (wife). The father sued the hospital and eye bank because “Judy” did not have authority to authorize donation. Nicoletta Court Ruling The Court upheld the “good faith” immunity protection conferred by the UAGA. The Court ruled that the hospital and eye bank had acted in “good faith” (“honest belief, the absence of malice and the absence of design to defraud or to seek an unconscionable act”). Maintain Clearly Defined Roles Neither the physician who attends the decedent at death nor the physician who determines the time of death may participate in the procedures for removing or transplanting a part. This section addresses potential public misperceptions and avoids the appearance of a conflict of interest. CA Health & Safety Code Section 7150.65(i) UAGA Section 14(j) Summary Strong public policy supports the transplantation community. UAGA upholds the rights of the individual and others to make an anatomical gift. A donor’s autonomous decision to donate must be honored. Continue to update policies and procedures in collaboration with providers, hospitals, and the OPO incorporating the evolving legal protections developed for donation. Call to Action To request a policy review, please call your Donation Development Coordinator directly or contact: Clinique Burrell Executive Assistant OneLegacy Donation Development Department 213-229-5634 / cburrell@onelegacy.org