File
advertisement

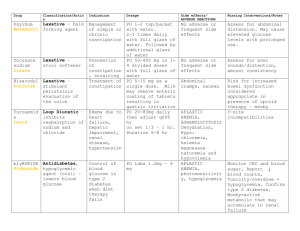
Medication Dose Frequency Route Purpose/action C- Category H - How this category works N - normal dosage ranges W - Why my pt is on it Bisacodyl (Ducolax) 10 mg Rectal (suppository) Once Stimulant laxative Stimulats the bowels to produce a BM ??? -- but it may take 6-12h for this to cause a BM Pt had diarrhea --Ducolax treats constipation & cleans out the intestines before a bowel exam/surgery T-Having a BM within 6-12h C-abdominal pain or cramping, nausea, diarrhea, or weakness L-irregular heartbeat, decreased urination, allergic reaction Proton pump inhibitor Suppresses gastric acid secretion by specific inhibition of an enzyme; blocks the final step of acid production 20-40 mg PO daily for the reduction of risk fo gastric ulcers Bc stomach is forever producing gastric acid & the more stress you have the more acid that is produced… dr don’t want pt to have a stomach problem so pt is on nexium to prevent abdominal discomfort T-gastric acid decreases, thus decreasing heartburn c- headache, dizziness, abdominal pain, diarrhea, nausea, URI symptoms Amino acid (found naturally in the body) Used for SE such as diarrhea, t-diarrhea will decrease, immune system will stay good c-don’t use if you Esomeprazole (Nexium) 20 mg Q morning before breakfast IV Glutamine (Glutasolve) 15 mg (oral powder packet) PO Daily Side effects T-therapeutic C-common L -life threatening Nursing Implications A - assess before giving W - watch for? IV - drugs alcohol, dilute, etc Outcomes Ppredicted outcome A - Actual outcome If pt is passing flatus, make sure they either have a commode, bedpan, or are able to get up to use the BRM on their own If pt has a BM, and any abdominal pain or n/v p-pt will have a BM within 612h of administering a-goal not met. Did not give med to pt. However, pt was having intermittent diarrhea all day a- urinary output bc Nexium can cause URI symptoms as a SE W-abdominal pain??? IV - Give IVP over at least 3 minutes (or .5 mL per 15 seconds) & FLUSH w/ sterile saline p-pt will not c/o heartburn or GERD a-goal met pt did not c/o heartburn or GERD a- liver lab values w- liver lab values, any complaints of n/v p-pt's diarrhea will decrease a-goal not met. Pt Heparin 5000 units Q8h subcut Trace elements comb. No. 1 (Addemel N) 50 mL Q M, W, F IVPB @ 100 mL/h muscositis, nerve pain. Glutamine is also used to protect the immune system & digestive system in ppl undergoing esophagus radiation. Multiple others Max 40 mg daily Pt has diarrhea - this is used for cancer pts who have diarrhea as a SE…….GLUTAMINE PROMOTES GOOD BACTERIA IN THE BOWELS!! are pregnant, have mania, or severe liver disease (Glutamine can worsen liver damage), or seizures continued to have diarrhea as the day went on Anticoagulant Heparin inactivates factor Xa, therefore inhibiting thrombus & clot formation by blocking the formation of prothrombin --> thrombin & fibrinogen --> fibrin (which are the final steps in the clotting process) 5000 units for prophylaxis of postoperative thromboemboli sm Pt had surgery 6 days ago (exploratory lap (laproscopic surgery) w/ repair of fistula) t-blood thins out c-bruising l-hemorrhage, white clot syndrome Adult trace element Elements include: chromic chloride, copper t-pt's lab values are WNL c-over supplementation of trace elements a-PTT lab value w-any bruising, internal bleeding (sudden increase in HR then decrease in BP) Subcut-alcohol swab, pinch skin, 45-90 degree angle a-trace element levels w-? p-blood clot will not form a-goal metclot did not form (pt ambulating helped this) p-pt's trace elements will increase a-unknown, a few lab values for a duration of 30m TPN 95.8 mL/h Continuous IV o PICC lumen #2 Diphenhydramine (Benadryl) 12.5 mg or 25 mg Q6h PRN o For itching IV chloride, ferric chloride, manganese chloride, K iodide, Na floride, Na molybdate, Na selenite anhydrous, sinc chlroide ??? He could be malnourished, alcoholic, poor & cant afford good food.. All possibilities are still off Total parental nutrition Provides protein, suguar, vitamins, minerals, & sometimes lipids ??? - depends on pt? Pt needs nutritional support (is also on Addemel N for trace element nutritional support)….. Or bc of an INFECTION or problems in your pancreas, intestines, BOWEL PT MAY BE MALNOURISHED OR AN ALCOHOLIC so pt is on TPN to build up immune system so pt can heal faster t-pt's electrolytes and lab values will be WNL c-protein/fluid overload Antihistamine, cough suppressant, anti motion-sickness Blocks histamine effects at h1receptor sites, has sedative effects 10-50 mL for t-pt's itching/inflammati on will decrease c-drowsiness, sedation, dizziness, epigastric distress, thickening of bronchial secretions l-anaphylactic a-lab values, intake & output w-fluid overload? Iv-may need to decrease level if pt has nausea To give: 1) remove TPN from fridge 2h before giving to allow it to warm to room temp 2) expiration date, don’t use if cloudy or has solid pieces floating g-pt will be able to handle 95 mL/h without nausea, lab values will be WNL Goal partially met - pt was able to handle 95 mL/h without nausea but lab values are not WNL a-give with food if GI upset occurs, where pt is itching at w-if itching decreases Iv-clean w alcohol swab before p-pt's itching will decrease to pt not itching anymore a-did not give Hydromorphone (Dilaudid) 2 mg IV Q4h for severe pain Oxycodone (Roxicodone) 5, 10, or 15 mg PO Q3h PRN for moderate-severe pain Promethazine (Phenergan) 12.5 mg IV or 25 mg rectal or 25 mg oral Q6h prn o For nausea injection Itching & to suppress coughs d/t hernia shock, 2 anemias, leukpenia, agranulocytosis, pancytopenia. Opiod analgesic Acts at specific mu-opioid receptors in the CNS to produce analgesia, euphoria, sedation For injection-110 mL Pt recently had surgery & this is his only pain med t-pain level will decrease c-n/v, dizziness, sedation l-RESPIRATORY DISTRESS, apnea, circulatory depression, respiratory arrest, shock, cardiac arrest Opioid analgesic Acts as agonist at specific opioid recepotrs in the CNS to produce analgesia, euphroria, & sedation Pt has this & dilaudid for pain - pt did not c/o pain throughout the day though t-pt's pain level will decrease to an acceptable level decided upon by the pt & RN c-dizziness, sedatoin, n/v, sweating l-shock, cardiac arrest, respiratory arrest, bronchospasm a-pt's pain level, RESPIRATIONS wRESPIRATIONS!!!!! ! Antiemetic Blocks histamine-1 receptors, diminishing the effects of histamine on cells 25-50 mg iv, 12.5-50 po An indication is postop pain or postop sedation, n/v t-n/v will decrease c-dizziness, drowsiness, urinary frequency, epigastric distress, thickening of bronchial secretions l-agranulocytosis, pancytopenia a- if pt vomitted w-n/v decrease, IV site Iv-Phenergan = irritant.. IVP admin REQUIRES dilution w/ 10 mL saline, a-pain level, RESPIRATIONS w-respiratory distress Iv-clean port w/ alcohol pad p-pt's pain level will decrease (however, pt did not c/o pain throughout the day) a-goal not met d/t med not being given p-pt's pain level will decrease to an agreed upon level bw the RN & pt a-goal not met r/t not given p-pt's n/v will decrease a-did not give