MOST Trial: Follow
advertisement

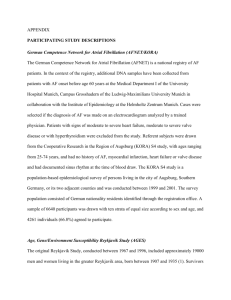
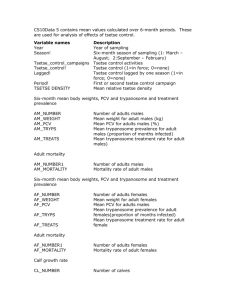
Pharmacological Prevention of Atrial Fibrillation Mattias F. Duytschaever, MD, PhD Electrophysiology Unit AZ St.Jan-Brugge University Hospital Ghent Bruxelles 2008 Pharmacological Prevention of AF Outline of the Presentation Atrial Fibrillation: The Clinical Problem − Changing Epidemiology of AF − Impact on Morbidity and Mortality Pharmacological Prevention of AF − Conventional Anti-arrhythmic Drugs − New “Anti-arrhytmic drugs” for AF Atrial Fibrillation: The Clinical Problem Clinically AF is a Multi-faceted Disease Parameters Par AF Pers AF Perm AF (N=1571) (N=1167) (N=1541) 64 ±13 66 ±12 71 ±11 Heart Failure 23% 35% 49% Valvular Heart Disease 19% 24% 40% Cardiomyopathy 7% 13% 16% Diabetes 15% 16% 22% Symptoms 77% 73% 55% LAD (mm) 43 ±7 46±8 51±17 Age Nieuwlaat et al, Eur Heart J 2005;26:2422 (Euro Heart Survey) Epidemiology of Atrial Fibrillation Prevalence (1 to 1.5%) and Incidence of AF Prevalence (%) Incidence/1000 person-years 17.8% 60 Framingham Study Mayo Clinic Study CHS Rotterdam Study 15 Framingham Study (men) CHS (men) Mayo Clinic (men) 40 10 20 5 40 50 60 70 80 40 Age (yrs) At 55y Life time risk for AF = 23.8% 50 60 70 80 90 Age (yrs) Miyasaka et al, Circ 2006;114:119-125 Heeringa et al, EHJ 2006;27:949-953 Epidemiology of AF is Changing Estimated Prevalence Pool at 2050 Projected N of Pts with AF (millions) 7 2050: 5.6 million 6 Age-adjusted Incidence/1000 person-year 4 3 3.68 5 4 2 3 2 3.04 2050:12 to 16 million 50% of AF>80y 2.3 1 1 0 1990 2010 2030 2050 Year Go et al, JAMA 2001;285:2370 1980 1985 1990 1995 2000 Year Miyasaka et al, Circulation 2006;114:119 Epidemiology of AF is Changing Temporal Relations of AF and CHF and their Joint Influence on Mortality (The Framingham Heart Study) Cumulative Incidence of AF in Pts with CHF Atrial Fibrillation and Heart Failure Another Vicious Circle 0.4 0.3 Heart Failure Incidence of AF 3-4% per year •Neurohormonal remodeling •Atrial enlargement Underlying •Loss of atrial funct •Atrial hypertrophy Heart Disease •Non-physiologic HR • atrial pressure (AHT, •Irregular V response LVH,VHD, •Atrial stretch •Loss of AV synchronicity age, •Atrial Fibrosis diabetes,..) •Electrical Remodeling 0.2 0.1 Atrial fibrillation 2 4 6 8 10 Years Wang et al., Circulation 2003;107:2920 Pharmacological Prevention of AF Outline of the Presentation Atrial Fibrillation: The Clinical Problem − Changing Epidemiology of AF − Impact on Morbidity and Mortality Pharmacological Prevention of AF − Conventional Anti-arrhythmic Drugs − New “Anti-arrhytmic drugs” for AF Impact of Atrial Fibrillation on Stroke Stroke Prevention in AF is a Pressing Health Concern Yearly Risk of Stroke in Nonvalvular AF is 5% AF is Associated with a 2 to 7-fold Increased Risk for Stroke Incidence of Dementia/1000 person-years The risk of Stroke increases Exponential with Age 80 60 Men with AF 20% of all Ischemic Strokes are Due to AF 40 40% of Patients with AF have Silent Brain Infarction General Men 20 In Patients with AF there is Twice as much Cognitive Dysfunction or Dementia 50 60 70 80 90 Age (yrs) Miyasaka et al, European Heart J 2007;28:1962-1967 Impact of Atrial Fibrillation on Stroke Long-Term Outcome in Pts with Lone AF: a 30-year Follow-Up Study Survival Free of Stroke/TIA (%) 100 96% 94% 80 60 40 Survival Free of Death (%) 89% 85% 88% 72%* 100 80 expected 60 observed 40 20 92% observed 68% 86% expected 57% 20 10 20 30 Years 10 20 30 Years Jahangir et al, Circulation 2007;115:3050-3056 Impact of Atrial Fibrillation on Mortality Mortality in AF Cases and Controls (Framingham Study) AF (men) Control (men) Total deaths 59.2* 34.3 Deaths for CVS causes 49.9* 21.2 Average time to death 5.9yr* 7.7yr Relative Risk of Mortality 4 2 Framingham Manitoba Kannel et al, NEJM 1982;306:1018 Whitehall Fuster et al, Circulation 2006;108:1979 Impact of Atrial Fibrillation on Mortality Does Atrial Fibrillation Increase Mortality in Heart Failure? Survival (%) 100 Sinus Rhythm 80 60 40 AF at Baseline 20 P=0.0013 10 20 30 40 50 FU (weeks) Middlekauff et al., Circulation,1991;84:40 Wellens et al., EHJ 2006;27:2740 Impact of Atrial Fibrillation on Mortality Studies Adressing Mortality Risk of CHF Pts with AF at Baseline Study N of AF EF(%) BB ACE/ARB Mortality RR P-value V-HeFT II (1993) 107/795 (FU 30m) 30% 0% 50% 20% vs 21% 0.76 0.18 Stevenson (1996) 140/750 (FU>24m) <40% 0% 60% 34% vs 25% 1.12 n.s. SOLVD (1998) 419/6517 (FU 33.4m) <35% 20% 50% 34% vs 23% 1.34 0.002 COMET (2005) 600/3029 (FU 58m) <35% 100% 90% N.R. (higher) 1.07 0.38 670/7599 (FU 37.7m) <40% 55% 55% 37% vs 28% 1.38 <0.001 478/7599 (FU 37.7m) >40% 55% 20% 24% vs 14% 1.80 <0.001 CHARM (2006) Neuberger et al, Eur H Journal, 2007;Sept 13 Impact of Atrial Fibrillation on Mortality Significance of AF in Heart Failure (1) New onset (Incident) AF is an Independent Risk Factor for Increased Mortality (“pre-terminal phenomenon”) Swedberg et al., Eur Heart J 2005;26:1303 (COMET) Wang et al., Circulation 2003;107:2920 (Framingham) (2) Prevalent AF is an Independent Risk Factor in Mild-tomoderate CHF Olsson et al., JACC 2006;47:1997 (CHARM) Crijns et al., Eur Heart J 2000;21:1238 (PRIME II) (3) Prevalent AF is an Independent Risk Factor in Ischemic Heart Failure Pedersen et al., Eur Heart J 2006;27:2866 (DIAMOND) Wellens et al., Eur Heart J 2006;27:2740 Pharmacological Prevention of AF Outline of the Presentation Atrial Fibrillation: The Clinical Problem − Changing Epidemiology of AF − Impact on Morbidity and Mortality Pharmacological Prevention of AF − Conventional Anti-arrhythmic Drugs − New “Anti-arrhytmic drugs” for AF Challenges of Therapies in AF Clinical Objectives for Therapy of AF Prevention of Stroke Preservation/improvement of LV Function Relief of Symptoms Reduction in Mortality The Preferred Strategy would be Pharmacological Rhythm Control, if Obtained Effectively and Safe Importance of Sinus Rhythm!! Rhythm vs Rate Cumulative Mortality (%) Sinus vs AF Endpoint Free Survival (%) 100 30 n:352 n:306 25 Rhythm Control 20 15 Sinus Rhythm 80 Atrial Fibrillation 60 Rate Control 40 AFFIRM 20 10 5 0 12 24 36 48 60 FU (months) Survival in CHF and AF 100 (%) 80 Amiodarone 0 5 10 Survival in CHF and AF 100 (%) 15 20 25 30 35 FU (months) Sinus Rhythm 80 60 60 40 STAF Placebo CHF-STAT 20 0 12 24 Atrial Fibrillation 40 20 CHF-STAT 0 36 12 FU (months) 24 36 FU (months) Conventional Antiarrhythmic Drugs for AF Vaughan Williams Classification of Antiarrhythmic Agents Fuster et al., JACC 2001, page 1-70 Conventional Antiarrhythmic Drugs for AF Efficacy of Class IC and III to Prevent Persistent AF Predictors for Recurrence Maintenance of Sinus Rhythm SR (%) 100 Male Gender Amiodarone 80 Age >75 Sotalol 60 Amiodarone Digoxin Sotalol 40 Propafenone LA <52 LVEDD 20 25% Duration>1year 0.001 0.01 0.1 1 10 100 Absence of Recurrence Duytschaever et al., PACE 1999 100 200 300 400 500 Days of Follow-up CTAF, Roy et al., NEJM, 2000 Conventional Antiarrhythmic Drugs for AF Review of RCTs on Prevention of Recurrence of AF after DCC RCT included into analysis Total No. of patients 44 11,322 Placebo controlled 25 Active comparator 14 Persistent AF 38 (60% pts) PAF/recent onset 6 EF > 50% Lone AF 41 Follow-up 1 year 1 AF Recurrence Class IA Class IC Metoprolol Class III Amio Dofetilide Sotalol Q vs Class I Q vs Sotalol Amio vs Class I Amio vs Sotalol Sotalol vs Class I 0 Lafuente-Lafuente C, et al, Arch Intern Med 2006;166:719-28 0.5 1 1.5 2 Odds Ratio (95% CI) Conventional Antiarrhythmic Drugs for AF Rhythm Control v Rate Control (The AFFIRM Trial) Cumulative Mortality (%) 30 4060 patients, FU 5 year > 65 yr or Other RF for Stroke or Death Rate Control : heart rate from 80/’ en 110/’ ; continued coumadin Paroxysmal or Recurrent Persistent Asymptomatic AF Rhythm Control : cardioversion, antiarrhythmic drugs, Stop coumadin if SR n:352 n:306 Rhythm Control 25 20 P=0.08 15 Rate Control 10 5 Years (%) 0 Primary Endpoint (Death) 1 2 3 4 5 Wyse et al. NEJM 2002 Conventional Antiarrhythmic Drugs for AF Rhythm Control v Rate Control (The AF-CHF Trial) Primary Endpoint (Cardiovascular Death) 1376 patients, FU >2 year LVEF ≤ 35% and NYHA II-IV AF ≥ 6 h within last 6 months or one episode ≥ 10 min within 6 months and prior D/C shock 82% amiodarone (rhythm control) Roy et al, NEJM 2008;358:2667-77 Conventional Antiarrhythmic Drugs for AF Class I and III Drugs are Not Safe (Certainly not in CHF) Survival in Patients with CHF and AF (%) No Antiarrhythmic 100 Drugs Survival in Patients with CHF and AF (%) 100 90 80 80 60 Antiarrhythmic Drugs 70 (Quinidine, Procainamide, Disopyramide, Flecainide, Encainide) Amiodarone 40 60 20 50 0 90 180 270 360 450 540 630 Follow-up (days) Flaker et al.(SPAF), JACC, 1992 Placebo 12 24 36 Follow-up (months) Singh et al.(CHF-STAT),Circulation, 1998 Conventional Antiarrhythmic Drugs for AF Class I and III Drugs are Not Effective Nor Safe Efficacy % of Sinus Rhythm Safety Number of Deaths 169 160 75 60% 50 40% 25 140 120 130 129 113 100 52 81 Cancer 80 23 39 Pulmonary 60 40 37 35 20 Cardiac Rate 310 † Rhythm 352 † Vascular Non Cardiovascular Steinberg et al, Circulation 2004;109:1973 Conventional Antiarrhythmic Drugs for AF ACC/AHA/ESC 2006 guidelines for the management of AF Paroxysmal or Recurrent Persistent AF No Symptoms Antico and Rate Control Permanent AF Symptoms Antico and Rhythm Control Antico and Rate Control Fuster et al, Circulation 2006;108:1979 Conventional Antiarrhythmic Drugs for AF ACC/AHA/ESC 2006 guidelines for the management of AF No Heart Disease Coronary Artery Disease Heart Failure or Hypertension with LVH Flecainide Sotalol Sotalol Amiodarone Amiodarone Catheter Ablation Amiodarone Catheter Ablation Catheter Ablation Fuster et al, Circulation 2006;108:1979 Pharmacological Prevention of AF Outline of the Presentation Atrial Fibrillation: The Clinical Problem − Changing Epidemiology of AF − Impact on Morbidity and Mortality Pharmacological Prevention of AF − Conventional Anti-arrhythmic Drugs − New “Anti-arrhytmic drugs” for AF “Antiarrhythmic” Drugs for AF Disopyramide Amiodarone Sotalol Class IA Class III b-Blocker Antiarrhythmic Agents Class IC Dofetilide Propafenone Flecainide New Class III Agents Substrate therapies b-Blocker Azimilide Quinidine Tedisamil Dronedarone Multi-channel blockers ACEI ARB Statins PUFAs Pirfenidone Savelieva and Camm, Europace 2008;647-665 Novel Drugs Connexin modulators SAC Blockers Ranolazine Na+/H+ Inhibitors Na+/Ca2+ Inhibitor Adenosine Agonist ARDAs ARDAs (Vernakalant, AVE0118) Novel “Antiarrhythmic” Drugs for AF Pharmacological Modulation of Atrial Conduction (Rotigaptide) Inter Cellular Uncoupling Modulation of Gap Junctions 16 Weeks AF Eloff et al., Circulation, dec 2003 Novel “Antiarrhythmic” Drugs for AF Late and Early Class III Drugs (Experimental) S1 S1 400 Sinus Rhythm After 24 h of AF S2 142 186 Control “Late” versus “ Early “ Class III Drugs d-Sotalol ‘Early’ Class III IAAD to I 102 Control Ca IKur 118 d-Sotalol IKrIKs 74 After 48 h of AF Control 78 0 100 200 300 400 ms d-Sotalol Duytschaever et al., Cardiovascular Research, 2005,67:69-76 Novel “Antiarrhythmic” Drugs for AF Savelieva and Camm, Europace 2008;647-665 Novel “Antiarrhythmic” Drugs for AF ‘Early’ Class III Drugg AVE0118 (IKur Blocker) AVE 0118 (3mg/kg/h) Δ AERP (ms) Remodeled Atria * 60 * * * ms 220 QT-time 200 180 * 40 160 AERP400 140 20 120 100 0 200 250 300 350 Pacing Cycle Length (ms) 400 -20 -10 0 10 20 30 Time (min) Blaauw et al, Circulation Oct 2004 “Antiarrhythmic” Drugs for AF Disopyramide Amiodarone Sotalol Class IA Class III b-Blocker Antiarrhythmic Agents Class IC Dofetilide Propafenone Flecainide New Class III Agents Substrate therapies b-Blocker Azimilide Quinidine Tedisamil Dronedarone Multi-channel blockers ACEI ARB Statins PUFAs Pirfenidone Savelieva and Camm, Europace 2008;647-665 Novel Drugs Connexin modulators SAC Blockers Ranolazine Na+/H+ Inhibitors Na+/Ca2+ Inhibitor Adenosine Agonist ARDAs ARDAs (Vernakalant, AVE0118) New “Class III” Agents for AF Dronedarone (Post-Hoc Analysis) ADONIS (N=630, follow-up 1 year) Time to First CV Hospitalization or Death Time to AF Recurrence Placebo 0.8 Placebo 0.4 0.6 0.5 0.4 0.3 0.2 0.1 Dronedarone 400 mg BID Cumulative incidence Dronedarone 400 mg BID 0.7 Cumulative Incidence EURIDIS and ADONIS Meta-analysis Log-rank test results: p=0.0017 0.3 HR=0.80 p=0.16 95%CI=[0.59; 1.09] 0.2 0.1 Few adverse events 0.0 0.0 0 60 120 180 240 300 360 0 Time (days) 60 120 180 270 360 Time(days) ? ATHENA Singh BN et al, NEJM 2008 Hohnloser. Presented at Heart Rhythm Society 2008; May 2008; San Francisco, CA (A). New “Class III” Agents for AF ATHENA and Trial Design N=4628 patients with a history of paroxysmal or persistent AF • Age ≥ 75 years with or without additional risk factors • Age ≥ 70 years and ≥ 1 risk factor (hypertension, diabetes, prior stroke/TIA, LA ≥ 50 mm, LVEF ≤ .40) R Dronedarone (400 mg bid) Placebo Phase III RCT: Minimum follow-up 12 months Primary EP: time to Death or Cardiovascular Hospitalisation J Cardiovasc Electrophysiol. 2008;19:69-73. New “Class III” Agents for AF ATHENA: Patient Characteristics Placebo (N=2327) Dronedarone (N=2301) 72+/-9 72+/-9 Female gender 45% 49% AF at baseline 25% 25% Structural Heart Disease 61% 58% Arterial Hypertension 86% 87% Coronary Heart Disease 32% 29% Valvular Heart Disease 16% 17% NYHA III/IV 22% 20% EF<0.35 4% 4% Lone AF 6% 6% Age (yrs) New “Class III” Agents for AF ATHENA: Baseline Medications Placebo (N=2327) Dronedarone (N=2301) Betablocker 71% 71% Ca-antagonists 13% 14% Digoxin 13% 14% ACE/ARB 69% 70% Statins 39% 38% Vit.K anatagonists 60% 61% Aspirin 44% 44% New “Class III” Agents for AF ATHENA: Primary Outcome Time to first cardiovascular hospitalization or death Cumulative Incidence (%) 50 40 HR=.76 P<.001 30 Placebo 20 Dronedarone 10 Patients at risk Placebo Dronedarone 0 0 6 12 18 24 30 2327 2301 1858 1963 1625 1776 1072 1177 385 403 3 2 Months Mean follow-up 21 5 months. Hohnloser. Presented at Heart Rhythm Society 2008; May 2008; San Francisco, CA (A). New “Class III” Agents for AF ATHENA: Fatal Outcomes Outcome Placebo (N=2327) Dronedarone (N=2301) Hazard Ratio 95% CI P Value All death 139 116 0.84 0.66-1.08 .18 Non-CV death 49 53 1.10 0.74-1.62 .65 CV death 90 63 0.71 0.51-0.98 .03 Cardiac non-arrhythmic death 18 17 0.95 0.49-1.85 .89 Cardiac arrhythmic death 48 26 0.55 0.34-0.88 .01 Vascular non-cardiac 24 20 0.84 0.47-1.52 .57 Hohnloser. Presented at the Heart Rhythm Society. May 2008. San Francisco, California (A). New “Class III” Agents for AF ATHENA: Non-Fatal Outcomes Placebo (N=2327) Dronedarone (N=2301) Hazard Ratio 95% CI P Value 917 734 0.76 0.69-0.84 <.001 859 675 0.75 0.67-0.82 <.001 AF 510 335 0.63 0.55-0.72 <.001 CHF 132 112 0.86 0.67-1.1 .221 ACS 89 62 0.70 0.51-0.97 .030 Syncope 32 27 0.85 0.51-1.42 .542 Ventricular arrhythmia or non-fatal cardiac arrest 12 13 1.09 0.50-2.39 .828 Outcome Primary outcome First hospitalization for CV reasons Hohnloser. Presented at the Heart Rhythm Society. May 2008. San Francisco, California (A). New “Class III” Agents for AF ATHENA: Summary •Dronedarone Significantly Prolongs Time to Cardiovascular Hospitalisation or Death in Moderate to High Risk Elderly AF Pts • All Cause Mortality was Not Increased in Pts Receiving Dronedarone • Cardiovascular Mortality (Specifically Arrhythmic Death) was Lower in the Dronedarone Compared to the Placebo Group • The Reduction in CV Hospitalisation was Mainly Due to Fewer Admissions for AF and Acute Coronary Syndromes • Discontinuation of Study Drug Was Similar in Both Groups Indicating Good Tolerability of Dronedarone • The Development Portfolio of this Drug is Practically Complete New “Class III” Agents for AF Increased Mortality after Dronedarone Therapy for Severe Heart Failure After inclusion of 627 patients (310 in the dronedarone group and 317 in the placebo group), the trial was prematurely terminated beacuse of increased early mortality related to the worsening of heart failure ANDROMEDA Study; Kober et al. NEJM 2008, 358:2678-2687 “Antiarrhythmic” Drugs for AF Disopyramide Amiodarone Sotalol Class IA Class III b-Blocker Antiarrhythmic Agents Class IC Dofetilide Propafenone Flecainide New Class III Agents Substrate therapies b-Blocker Azimilide Quinidine Tedisamil Dronedarone Multi-channel blockers ACEI ARB Statins PUFAs Pirfenidone Savelieva and Camm, Europace 2008;647-665 Novel Drugs Connexin modulators SAC Blockers Ranolazine Na+/H+ Inhibitors Na+/Ca2+ Inhibitor Adenosine Agonist ARDAs ARDAs (Vernakalant, AVE0118) Substrate Therapies for AF Atrial Remodeling Therapies ACE inhibitors and ARBs Aldosterone antagonists Statins Corticosteroids n-3 PUFA (fish oil) Beta blockers Possible Target Hypertension Heart failure AA effects (anti-fibrotic, antiarrhythmic?) Hypertension, heart failure AA effects (anti-fibrotic, antiarrhythmic?) Prevention of Atrial Remodeling Disease Substrate Coronary artery disease Systemic atherosclerosis AA effects (antiinflammatory, antioxidant) Anti-inflammatory effects Lipid-lowering effects Antiarrhythmic effects AF Targets: -Prevention of Heart Disease -Prevent HD-induced Remodeling Reduction of BP, CHF MI, etc. Antiarrhythmic effects -Prevent AF-induced Remodeling Substrate Therapies for AF Prevention of AF by Treating Heart Failure (Primary Prevention) ACE Inhibitors AR Antagonists SR (%) Enalapril (5% AF) 100 Cumulative Incidence of AF 0.15 Placebo (8% AF) 80 Placebo (24% AF) 60 40 0.10 0.05 Valsartan (5.1% AF) 20 1 2 3 4 5 Years 6 12 18 FU 2.9y FU 23m (SOLVD) (ValHeFT) Vermes et al, Circulation 2003;107;2926 24 Months Maggioni et al, Am Heart J 2005;149:548 Substrate Therapies for AF Prevention of AF by Treating Heart Failure (Primary Prevention) Prevalence of recommended HF treatment in Euro Heart Survey on AF l -b a t be f o B n AR o ti or na - I i b E m AC o c nd a k oc er I EC ,A r ke c lo s - b ta li a e t i gi b d of nd n a tio AC a n bi B, O m co r AR o Geographic distribution of enrolment in Euro heart Survey on AF • 5333 patients • 35 countries • 182 hospitals European Society of Cardiology – Euro Heart Survey Eurlings L, et al. Preliminary results European Society of Cardiology – Euro Heart Survey With the courtesy of H Crijns Substrate Therapies for AF Prevention of AF by Treating Hypertension (Secondary Prevention) • N=250 • Mild AHT and Documented AF in Previous 6 months • Amiodarone 200 + Losartan 50mg • Amiodarone 200 + Amlodipine 5mg Fogari et al Journal of Cardiovasc. Pharmacol 2006 Substrate Therapies for AF Prevention of AF by Treating Hypertension (Primary Prevention) Stroke (%) New Onset AF (%) 8 7 10 RR: 0.67 [95% CI: 0.55-0.83], p<0.001. Atenolol 8 6 5 6 4 4 3 Losartan 2 Atenolol 2 Losartan 1 0 12 24 36 48 60 Months LIFE, Kjeldsen et al, JAMA, 2002; 288:1491 12 24 36 48 60 Months Wachtell et al, JACC; 2005; 45 Substrate Therapies for AF Prevention of Progression of AF (No Structural Heart Disease) Natural Hx and Progression of AF Study UK general practice, 2005 Tokyo study, 1995 CARAF, 2001 # pts Follow-up 525 1st PAF age 40-89 yrs Progression 70/418 (17%) 2.7 yrs; 1606 person- progression increased risk yrs of mortality 1.5 (0.8-2.9) 137 new onset PAF 560 men, 339 women AF 1 year 1st 30/137 (22%) 19%; time to 4.14 yrs progression 1138 days (men), 1092 days (women) 757 new onset PAF 8 (2-11) yrs 8.6% by 1 year; 25% by 5 yrs; probability of any AF 63% by 5 yrs 426 1st PAF 9 (0-24) yrs 141 (33%) Parkinson, 1930 200 PAF 10 yrs 25% Tokyo study, 2004 171 PAF 14 yrs 132/171 (77%) (5.5%/year CARAF, 2005 Danish study, 1986 Substrate Therapies for AF Secondary Prevention in The Absence of Heart Disease After ECV of Persistent AF SR (%) In Paroxysmal AF SR (%) Amiodarone+ Irbesartan 100 Amiodarone+ Losartan 100 80 80 60 60 Amiodarone Amiodarone 40 40 P:0.007 P:0.006 20 20 * 60 120 180 240 300 360 180 Days Madrid et al, Circulation 2002;106:331 360 540 720 Days Yin et al, Eur Heart J 2006;27;1841 Substrate Therapies for AF ACTIVE Study Dose-adjusted OAC (INR 2.0–3.0) Yes ACTIVE W R with AF Irbesartan (150–300 mg/day) Clopidogrel (75 mg/d) + ASA (75–100 mg/day) n = 14.500 Patients ACTIVE Investigators, Lancet 2006;367:1903-1912 Willing/able to take OAC No R R Clopidogrel (75 mg/day) + ASA (75–100 mg/day) ACTIVE A Placebo + ASA (75–100 mg/day) Primary endpoint: Stroke, MI, CV death, Systemic Emboli ACTIVE I Placebo Pharmacological Prevention of AF AF During the Next Half Decade Atrial fibrillation will become much more common Conventional therapies are only modesty effective New “safer” variations of conventional therapies are almost available Drugs with novel antiarrhythmic actions are in development New targets that prevent substrate development or suppress triggers will become available The rate versus rhythm debate will reignite Mortality and morbidity will improve