Acute Hip Fracture Ward - NHS Fife
advertisement

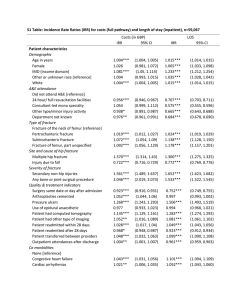
The Development of an Acut Fracture Ward Mr J A Ballantyne Cons Ortho Surgeon The development of an acute hip fracture ward • • • • Background Business Case Intended benefits Sustainability Hip Fractures in Fife (1982-2009) Hip Fracture Incidence; 65 and over; FIFE 500 9.00 450 8.00 400 7.00 300 5.00 250 4.00 200 3.00 150 2.00 100 50 1.00 0 0.00 1982 1983 1984 1985 1986 1987 1988 1989 1990 1991 1992 1993 1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 Hip Fractures 6.00 Hip Fractures Rate per 1000 Hip Fracture Rate per 1000 350 NHS Fife Trauma configuration Present • 2 trauma wards – 23 beds each • All trauma admitted next available bed • Hip fractures distributed across 2 wards • Hip fracture resources divided across 2 wards – CoE (P/T Staff Grade, 1 CoE session) – AHP input limited to 5-6/7 Planned • Acute Hip Fracture ward • General trauma ward • CoE resources concentrated on acute hip fracture ward – – – – 2 sessions CoE Cons P/T CoE Staff Grade 2 ESP Fragility Nurses Increased AHP input to allow 7 day service – Weekly Ortho Con ward round (3 dedicated consultants) Background….an ongoing process beginning in 2009 2009: Introduced a hip fracture patient pathway • Consultant engagement 2010: Introduced a Enhanced Care Area for Hip Fractures • Patients post hip fracture surgery optimised • Increased nursing care, careful fluid balance, reg. review • Introduced with some naivety • Staffing numbers incorrect – Unable to complete intended assessments • Required regular transfer of patients between bed spaces – not good practice in the cognitively impaired – Inefficient use of nursing staff Our first attempt….why did they fail? • Ward changes poorly planned – Recognized need for improvement – Failure to engage fully with MDT re changes • Ortho Consultant engagement/interest? • Limited CoE input • Management buy in…. – Hip fractures not a government priority – Other competing targets took priority • Lack of national targets – E&W had NHFD – tariff driven care 2012: Development of Orthogeriatric services for Patients Sustaining Fragility Fractures in NHS Fife: the need to comply with national standards Best Practice In Hip Fracture care: The case for Orthogeriatrics in the care of fragility fractures: Published Guidance and Drivers for Change • • • • • Blue Book National Hip Fracture Database Nice Guideline (June 2011) Sign Guideline 111 (June 2009) SHFA Present Management of Hip Fracture in NHS Fife What Care Model to adopt? Recommended Model Does Orthogeriatric Input make a difference? What level of Orthogeriatric Consultant support is required? Possible Models and Patient Flow Benefits of Improved Orthogeriatric Levels of Care – – – Cost savings to planned care directorate Foundation Trainees Support GMC response to patient safety concerns (May 2012) Funding the Orthogeriatric Service Conclusion Conclusion “The establishment of an orthogeriatric unit. This is the preferred option and the current recommended model of care from the BGS……. high level features in this sort of model are pre op assessment, the potential development of specialist roles such as hip fracture nurses…………chances of a discharge home are felt to be optimized using this model “ 2013- present…..re-allocation of resources • Started the development of an Acute Hip Fracture ward – – – – – • Admitted under shared care Admitted directly to the hip fracture ward Return to ward post op Post op rehab led by specialist MDT team Care pathways 1 sessions CoE Cons time (MDT) – 1 P/T CoE staff Grade Ortho Staff Grade salary 1 (retiral) – – – Appointment of 2 Fragility Nurse ESP Work alongside CoE medical staff Provide CGA, peri-op medical management • Secondment HAN nurse to support training of the ESPs • Ortho Staff Grade salary 2 (retiral) Staffing at this time – • • – – Appoint CoE Consultant P/T Work absorbed by Ortho Cons • • • Regular MDT team meetings • Additional CoE Cons session – • No applicants Reflects national shortage CoE consultants Alternative solutions preferred by local CoE Cons Presently 2 CoE Cons Ward rounds Cons Ortho Ward round weekly – – Additional to routine trauma ward rounds Aim to provide consistancy of decision making by a core of 3 Ortho Cons ….late 2013 • Made lots of local departmental changes to try and improve service – Converting surgical salaries to medical/nursing • Still lacked the final impetus to take us to the acute hip fracture ward SOSDG Hip Fracture Care Work strand • Scottish Standards of Care for hip fracture patients (2013) • National monthly snap audits • Provided the drivers for change • Evidenced areas we needed to do better – Allowed business case to be made to address these areas • Management engagement – national audit – Well supported in making change e-Health Information Services Department Hip fractures admissions in FY 2009/10 to 2013/14 split by time of admissions 45 40 35 30 25 20 15 10 5 0 2009-10 2010-11 2011-12 2012-13 2013-14 Day of the week of a Hip fracture procedure from FY 2009/10 to FY 2013/14 70 60 2009-10 50 2010-11 40 2011-12 30 2012-13 20 2013-14 10 Monday Tuesday Wednesday Thursday Friday Saturday Sunday Business Case for the acute hip fracture ward Focused on areas in the snap audits where we performed poorly • LOSx • Post Op mobilization • CoE input • Demonstrate areas of improvement against national data • Comparison to National Hip Fracture Guidelines Acute Hip Fracture Ward • Concentrate available resource to single area • Allow development of patient care pathways • Develop team dedicated to hip fracture patient care • Aim to reduce LOSx – Reduce dependence on downstream beds – Increase patients discharged directly home • Cost savings in terms of hip fracture care SOSDG funding Present • OT 5 out of 6 day working – Working to capacity – Staffing levels not allow 7 day input • Physio 6 out 7 – Working to capacity (Trauma/Elective) – Input aimed at those DC withing 48 hrs (ie ERP) Planned • Additional 2 generic AHP assistants – Allow 7 day input OT/Physio • 2nd physio working Saturday and Sunday – Work with the assist AHPs to increase ability to clinically prioritise post op mobilisation (elective/trauma) • Increased Nurse staffing levels Measure impact National Audit Local Audit • • • • SOSDG Audit LOSx – Recognition of other factors Physio time to initial assessment • • • • Physio – audit reasons for delay in first assessment OT – proportion assessment achieved on day 1,2 and 3 Proportion of patients transferred to downstream bed (present 51% - aim 20%) Impact of hip fracture ward on ICASS – 30% patient presently discharged through ICASS – 15% DC directly home – Local audit ICASS/DC Hub Audit of numbers of boarding patients from other directorates – Potential for remuneration form emergency care and resultant true cost saving to planned care Sustainability • Run as pilot for 1 yr • Report back to Senior Management Team at 1yr – – – – – Evidenced by reduced LOSx Reduction in patient bed days for NOF♯ Increased numbers patients DC home Increased use of ICASS Show efficiency of use of current resources • If benefits confirmed, commitment to recurring funding agreed by NHS Fife Ongoing challenges…….. • Limited CoE input well below levels required for these patients – – • Social Care issues locally/lack of down stream beds – • More interesting trauma cases often take priority Showing benefits of the ward beyond LOSx – – • reduced LOSx savings offset by boarding patients form other directorates Need to recognise the cost of boarding patients into trauma beds Prioritisation of hip fractures on trauma list – • Reinforce the benefits of good care Demonstrate the impact of increased medical input Showing actual cost saving with improved care – – • Potential impact on LOSx Staff apprehension regarding ward change – – • Alternative solutions using Fragility Nurse ESP 7 day consultant led CoE care still a dream Demonstrating benefits of the softer end points eg quality of care, patient satisfaction Softer outcomes may not be shown in terms of cost saving Medical support of other Fragility Fracture patients – – Concentration of present resources on Hip fractures Need to develop pathways of care for non hip fracture fragility patients MDT effort…… • • • • • • • • • Nursing (Maureen Speedie, Eileen Hanlon, Dorothy Letham, Karen Peacock, Andrea Bendowski) OT (Elaine Murray) Physios (Janet Macdonald, Liz McMullen, Karen Gray) CoE (Jo Hadoke, Sue Pound, Morag Paterson, Marie Williams, John McKenzie) Orthopaedic (Andy Ballantyne, Ed Dunstan) Planned Care Management (Susan Fraser, Fiona Cameron) Emergency Medicine (Maggie Currer) Anaesthetics SOSDG Audit Nurse (Jan Wood) Thank you…. CoE requirements in an orthogeriatric ward ‘An estimate of two direct clinical care sessions per week for each 100 hip fracture patients per year of senior Orthogeriatrician time is required to provide a basic service.’ ‘However, it is essential that there is a Consultant Geriatrician involved in the day to day running of the service to provide continuity of care, in making difficult decisions regarding fitness for theatre, in complex discharge planning and in end of life decision-making.’ The involvement of two Orthogeriatricians sharing the workload along with their other commitments should be considered and would provide a balanced job plan and ensure adequate cross cover when necessary.’ June 2010 BGS Newsletter5