Coding Compliance in Healthcare: A Presentation
advertisement
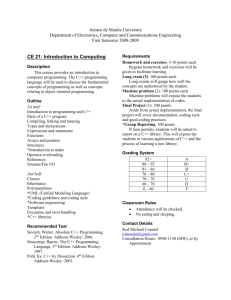
CODING COMPLIANCE October 18, 2002 Shana K. Wolfe, CHC, CMA Director of Business Integrity Washington County Health System, Inc. History Coding not the basis for payment in 1965 (beginning of Medicare) Patient volume and costs have climbed steadily Number and types of clinical interventions has skyrocketed For-profit hospital chains have changed the landscape Managed care and focus on cost containment DRG system in 1983, then APC system in 2000 GREED!!! Cases Pneumonia Chest Pain TIA/CVA Cases w/cc vs. w/o cc Consequences Personal career impact Financial loses to hospitals from fines and penalties BIG public relations nightmare! Expensive corrective strategies if placed under CIA Resources AHIMA Standards of Ethical Coding Guidelines of four Cooperating Parties – AHA, AHIMA, CMS, NCHS UHDDS Updated AHA Coding Clinics Compliance programs and OIG guidance Peer Review Organization Manual, section 4130 – DRG Validation Reviews Personal Responsibility Adherence to Code of Ethics QUERY PHYSICIANS!! Participate in documentation improvement projects The “big shots” go to jail, not coders (unless there is an incentive plan tied to CMI) Preventative Strategies Support coder credentialing and continuing education Consider internal coding peer review Utilize periodic third-party coding reviews Develop a coding compliance policy Profile your hospital coding patterns to state/nation Consider a documentation specialist for coding support Monitor your hospital’s CMI Thank you for your time and attention. Any questions?