Genitourinary Surgery - JATC Surgical Technology
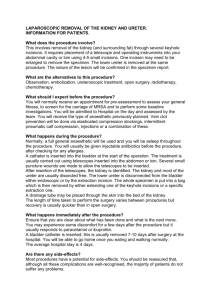
advertisement

Genitourinary Surgery Anatomy Suprarenal (adrenal) Glands Adrenal glands-sit on the superior and medial portion of the kidneys. Endocrine glands with a cortex and medulla. -Cortex- secretes steroidtype hormones essential to the control of fluid and electrolyte balance. -Medulla- secretes epinephrine and norepinephrine. -Enclosed within the Gerota’s fascia Kidneys: Filter waste Left kidney is larger than the right. Right kidney is lower than the left. Located in the retroperitoneal space. Nephrons are the functional unit of the kidney. There are more than 1 million nephrons. Two types- juxtamedullary (deep) and cortical (shallow) nephrons. 2 Basic Units of the Nephron Renal corpuscles Consist of a network of capillaries Called the glomerulus, and Bowman’s capsule Lie in the cortex of the kidney. Create a filter through which many substances must pass. Renal tubules Consists of 3 units Proximal convoluted tubule Loop of Henle Distal convoluted tubule. Ureters Conduct urine from the kidney to the bladder Have thick-walled muscular tubes with small lumen. Terminates by running obliquely through the wall of the bladder for about 1.5 cm. It allows the bladder to prevent reflux through muscular contraction upon the ureter. The pelvic ureter in the female relates to other structures in such a way as to create several surgical problems. Urinary Bladder Urine collects in the bladder Lies in the anterior half of the pelvis. Lined with a mucous membrane that is wrinkled when the bladder is not distended. Openings to the ureters are approximately 3 cm apart. Trigone-triangular area connecting ureters and urethra Male bladder lies on and is attached to the base of the prostate gland. Detrusor Muscle Male Reproductive System Penis and Male Urethra Cylindrical structure composed of three cylindrical masses of cavernous tissue. Two Corpora Cavernosa Corpus Spongiosum Penis Lies in the midline below these two structures. Expands distally forming the glans penis. Urethra passes through here and opens to the exterior via a slit like opening, the urethral orifice or meatus. The skin covering the penis is thin, hairless, and somewhat dark. The prepuce (foreskin) resembles a mucous membrane and covers the glans penis. Urethra- passes through the prostate gland Prostatic section of the urethra passes through the prostate with a gentle forward curve. Ejaculatory duct opens on each side of a urethral structure called the prostate utricle. Spongy section of the urethra is about 15 cm long. Female Urethra Only 4 cm long. Passes in front of the lower half of the vagina. Voluntary sphincter muscle surrounds the female urethra. Some of these muscle fibers help form the urethrovaginal sphincter. Skene’s glands provide lubrication. Testes Paired structures contained in the scrotum Tunica Vaginalis-interior lining of the scrotum Tunica albuginea-thick external connective tissue covering the testes 800 seminiferous tubles which connect to the epididymis Ductus Deferens (Vas Deferens) Arises from the epididymis 45 cm long Center portion of the spermatic cord Joins the seminal vesicle distally to form the ejaculatory duct Ejaculatory Ducts-lie within the prostate where they enter the prostatic urethra Prostate Gland Accessory gland (seminal) Lies at the base of the bladder Urethra runs through it Entry site for ejaculatory ducts Enclosed by a capsule Pathology Cushing’s Syndrome Over production of cortisol by adrenal cortex caused by Over production of ACTH (adrenocorticotropic hormone) by the pituitary gland (80%) Or a tumor of the adrenal cortex (20%) Benign or malignant Diagnosis Urine and blood tests CT or MRI of brain Adrenal ultrasound Symptoms Central body obesity Glucose intolerance Hypertension Hirsutism (hairiness) Osteoporosis Kidney stone formation Emotional instability Menstrual irregularity Treatment Surgical removal of pituitary tumors Radiation Benign adrenal tumors are removed endoscopically (general surgeon) Malignant adrenal tumors removed in open procedure Adrenal Insufficiency (Addison’s Disease) Adrenal glands fail to secrete hormones necessary to maintain fluid balance and blood pressure, or they inhibit the stress response May be triggered by stress Infection Surgery Trauma May be a complication of TB or AIDS Symptoms Weight loss Weakness and fatigue GI disturbances Low blood pressure Darkening of skin Hair loss Dramatic mood and behavior changes Treatment is medical Hormone replacement therapy (corticosteroids) Pheochromocytoma Tumor of the medulla of the adrenal gland Over production of adrenalin Can be deadly Symptoms Severe headaches Excess sweating Tachycardia-palpitations Anxiety Tremor Pain in the epigastric region Weight loss Heat intolerance Treatment-surgery Most tumors are small so are removed endoscopically Pathology of the Urinary System Bladder Urinary incontinence Cystitis Calculi Urinary reflux Neurogenic bladder Trauma Straddle Injuries Cancer Bladder Tumors Symptom-hematuria Benign or malignant Benign (papillomas) occur only in young adults Cystoscope to diagnose and tumor is removed transurethrally Malignant arise from epithelial lining-men over 50 Mushroom shaped with a stalk For bladder wall invasion partial or total cystectomy may be required with rerouting of ureters Chemotherapy and radiation Single or multiple Urinary Calculi Stones-small solid particles Imbedded or travel and obstruct Symptoms Painful urination Frequent urination Passage of small amounts of urine Flank pain Nausea and vomiting Urinary tract infection (UTI) Hematuria 50% recurrence Chemical types Calcium-(75%) diet or hyperparathyroidism Struvite-(15%) magnesium ammonium phosphate from chronic UTI pH higher than 7.0 Uric acid-(6%) gout pH less than 5.5 Cystine-metabolic defect of renal tubules Failure to reabsorb certain amino acids Treatment Spontaneous passage Surgical Extracorporeal shock wave lithotripsy Cystoscopicureteroscopicnephros copic Percutaneous Open Kidney Disorders Affect Fluid and electrolyte balance, blood volume, and ability to filter waste Pyelonephritis Renal Calculi Polycystic Kidney Disease Multiple fluid filled cysts (benign) 3 types Autosomal dominantinherited (90%) 30-40 year olds Autosomal recessiveextremely rare Young children Acquired cystic Patients with long tern kidney disease Symptoms Flank pain Headaches Hypertension Chronic UTI Hematuria Cysts in kidneys and other organs (liver) Leads to kidney failure (50%) end stage renal disease Treatment Dialysis or transplant ( if both kidneys are affected Diabetic Nephropathy Other names Kimmelstiel-Wilson disease Diabetic glomerulosclerosis Uncontrolled diabetes Nephrons sclerose Symptoms Thirst and edema Chronic renal failure to end stage renal disease in 2-6 years Treatment Dialysis or transplant End-Stage Renal Disease (ESRD) Kidney failure Function at less then 10% of their normal capacity Final stage of many types of kidney disease ½ are diabetic Kidney filtration is no longer effective-no urine output Death occurs from accumulation of waste and fluids Treatment-dialysis or transplant only Dialysis Hemodialysis Establish vascular access Insert a shunt or long dwelling catheter in forearm 2 cannulas Inflow Outflow A portion of the patient’s blood is pumped from the body to dialysis machine 2 compartments Incoming blood Solution of dialysate Semipermiable membrane between Blood passes over the membrane and fluid and waste are filtered I into dialysate Lager substances, blood, protein are returned to body 3 treatments per week 2-4 hours each Peritoneal Dialysis Continuous ambulatory peritoneal dialysis (CAPD) Permanent catheter in lower peritoneal cavity Dialysater infused into peritoneal cavity Peritoneum acts as filter Dialysis may be treatment of choice or temporary measure while waiting for a kidney Dialysis Renal Cell Carcinoma Most common type of kidney cancer More common in men then women Age of 50-60 Direct link to smoking and heredity Metastasizes to the lungs Radical nephrectomy-75% 5 year survival rate Congenital Nephroblastoma Wilm’s tumor Malignancy found in children (3-4 yrs) 90% of cases only one kidney involved Asymptomatic until late stages Hypertension Hematuria Abdominal enlargement Nephrectomy before metastasis has 90% 5 yr survival rate Pathology affecting the male reproductive system Phimosis Foreskin can’t retract over the glans Can cause infection do to inability to clean Pain during erection Circumcision treats this condition Hypospadias/Epispadias Hypospadias-urethral opening occurs on the under side of the penis or on the perineum (or in the vagina of a female) Epispadias-absence of the anterior wall of the urethra. Opens on the dorsal side of the penis Benign Prostatic Hypertrophy Most men over the age of 50 Prostate enlarges-can no longer expand outwardly due to capsule, so swells into the urethra Urination-frequency, urgency, and urinary retention Rectal exam Prostate specific antigen (PSA) to rule out cancer Transurethral Resection of the Prostate (TURP) is procedure of choice Cancer of the Prostate Early stages are asymptomatic Same obstructive symptoms a BPH Matastasis to bone and other organs Radical prostatectomy (suprapubic or retro pubic) with pelvic lymph node dissection Orchiectomy, radiation, hormone therapy Chemotherapy is not effective Cryptorchidism One or both testicles fail to descend into the scrotum (after 1 yr) Can cause future infertility Associated with premature birth and inguinal hernia Orchiopexy-fixation of testicle in normal position Testicular Torsion Twisting of the spermaticord Pain and eschimia Temporary manual derotation Orchiopexy to prevent recurrence Wood’s lamp to determine viability of the testicle Testicular Cancer Young men between 20 and 40 Patients who had cryptorchisism are at higher risk Young men are too embarrassed to report so goes to advance stages without treatment Orchidectomy with radiation or chemotherapy Bilateral orchiectomy-can reserve sperm Testicular implants are available Trauma to the Genitourinary System MVA Abusive or forceful sexual activity Blunt physical contact Penetrating wounds Hemorrhage can lead to shock or permanent impotence Priopism Erection that won’t subside Vessels allowing blood to exit won’t open Decompression is necessary Can lead to permanent impotence Other Male Pathology Balanoposthitis- inflammation of glans Prostatitis Erectile dysfunction Penile cancer Epididymitis Hydrocele Orchitis Varicocele Sexually Transmitted diseases Genital Warts Urinalysis Clean container Clean catch Disinfect Midstream Sterile Catheter 24 hour sample Microscopic exam vs. strips Other Tests History and physical Lab-blood and Urinalysis X-ray-KUB IVU- retrograde urogram (IVP-IV pylogram) Ultrasound CT scan MRI Biopsy Endoscopy Equipment Table for lithotomy and x-ray X-ray equipment (give radiology notice) X-ray gowns Poles for irrigation fluid Drainage system in table or floor Sitting stool for surgeon Supplies Lubricant Foley and drain bag Catheter guide Ureteral catheters and baskets Incisions Inguinal Scrotal-transverse with tension Pfannestiel Gibson Flank Lumbar Abdominal Surgical Procedures Adrenalectomy To remove a tumor causing Cushing’s Syndrome Pheochromocytoma Breast or prostate cancer Endoscopic or open (large tumors or malignancies) Procedure Flank incision #10 blade possible rib instruments Dissection Pickups and scissors Bovie Cut fibrous attachments of gland Pickups and scissors Transect artery and vein Clamp, clamp, cut, tie, tie Irrigation & hemostasis Asepto, bovie Closure Wilms Tumor Transverse skin incision Moist sponge placed over tumor to protect it. Tumor spillage increases local tumor recurrence Umbilical vein and renal vein are ligated Renal arteries and adrenal arteries ligated Tumor , adrenal glands, ureters and unilateral lymph nodes are removed. Irrigated and inspected Wound closure Nephrectomy Total or subtotal removal of kidney Subtotal-upper or lower pole only biopsy, calculi, or small cancer Renal cooling if artery will be occluded for a long period of time Use of iced slush Reduces metabolic requirements of a kidney Reduces the possibility of tubular necrosis Need sterile iced slush and Collins solution Procedure Flank incision #10 blade Dissection and mobilization of kidney Pickups and scissors Control artery Vessel loop or bulldog clamp Retract renal capsule Pickups and scissors Ligate segmental artery Clamp, clamp, cut, tie, tie Remove segment #10 blade, pickups Close capsule Cover defect with peritoneum or omentum Close Simple Nephrectomy Flank incision #10 blade, bovie Dissection Pickups and scissors Rib extraction inst Isolate and ligate the ureter Pickups and scissors, suture Expose and ligate the renal artery and vein Pickups and scissors Clamp, clamp, cut, tie, tie (0 silk) Remove kidney Hemostasis Close Removal of kidney only Small malignancies, chronic obstructive disorder, benign tumors, transplant kidney. Living donor hepranized prior to removal Kidney infused with cold collins (perservative) solution. Radical Nephrectomy Removal of kidney, adrenal gland, perirenal fat, upper ureter, gerota’s fascia Regional lymph nodes may be included Abdominal incision Abd. Organs can be inspected for metastasis. Intake and output levels are measured for 24-48 hours postoperatively Remaining kidney is expected to handle additional load without difficulty if not diseased. Renal Transplant Sources Cadavers Advanced directive or family consent Anesthesiologist-maintains heart and lungs Could need to transport organ Collins solution and iced slush used to preserve Living donors Simple nephrectomy Left kidney usually used due to longer renal vein 80% success with unrelated, 90% if related Compatibility-blood studies Recipient Undergoes dialysis just before the procedure to stabilize fluid and electrolyte balance Graft is placed in the right pelvis through gibson incision Graft to internal iliac artery and external iliac vein Perfusion of kidney is allowed and observed for proper color Manitol will be given to increase urinary output Anastomosis of the ureter to the bladder Children have kidney anastomosed to the aorta and inferior venacava (midline incision) Transurethral Endoscopy of the Genitourinary Tract Cystoscope (0, 30, 70,120 degree) or ureteroscope (rigid or flexible) Patient is in lithotomy Introduce scope through the male or female urethra Procedures Retrograde urogram Visual diagnosis Bleeding tissue fulguration Prostate tissue removal (TURP) Removal of bladder tumors Ureteral stents Caliculi removal Urethral enlargement Equipment sterilization Gas vs. steam vs. cidex Tech often sets up table (open glove) then scrubs out No saline in graduate After table is setup may assist with circulating duties Keep plenty of fluid hung Inflow and outflow should match closely “A variety of urinary catheters should be available for insertion at the end of the procedure. The surgeon, circulator, or Surgical Technologist may perform this task.” (p. 776 AST) Stone Removal Spontaneous increase fluids, muscle relaxants, pain medications Lithotripsy painful-general anesthetic Endoscope of urinary tract Open procedures Lithotomy Open stone removal Position and incision depends on location of the stone Pylolithotomy-stones in the kidney or upper ureter-flank incision Gibson incision for stones in lower ureter Suprapubic or phannesteal incision for bladder stones Extracorporeal Shock Wave Lithotripsy (ESWL) Pulverizes Calculi into small fragments for evacuation with the urine Kidney and upper urethral stones only Expensive specialized equipment so some facilities share the equipment (mobile machines) Buttocks and torso are submerged in pool of deionizing water C-arm locates stone then shock waves pulverize stone. Recheck with C-arm every 200 shocks 1000 shocks for a 4 mm stone 2,400 shocks maximum exposure for a day Patient strains urine for stone fragments to analyze chemical composition Endoscopic Stone Manipulation Stones are accessed transurethrally Cystoscopy and ureteroscope (flexible or rigid) may be needed Glide wire or guide wire to maintain communication of ureter from bladder to kidney Stone baskets or laser C-arm and retrograde dye to identify location of stone. Get all air out of syringe-looks like a stone. Ureteral stent my be placed to maintain patency of the ureter Ureteral Reimplantation Pathology requiring urinary diversion. Ureteroneocystostomy Reposition the ureter on the superior portion of the bladder. Ureterostomy Opening the ureter for continuous drainage into another body part. Ureterectomy Complete excision of the ureter In conjunction with a nephrectomy Ureteral Reimplantation Ureteroureterostomy Excision of a traumatically injured or diseased portion of the ureter with reanastomosis to restore continuity to the ureter. Ureteroenterostomy Ureteroileostomy (ileal urinary conduit) Diversion of the ureter into a segment of the ileum Ureterosigmoidostomy Diversion of the ureter into a segment of the sigmoid. Suprapubic Cystotomy Suprapubic catheter-when transurethral approach is impossible Men with enlarged prostate Disabled Percutaneous Procedure Shave prep and local anesthetic Incision #11 blade Insert cystostomy tube just above pubis Remove obturator from tube Inflate balloon the suture or tape in position Connect to collection device Regulate speed of evacuationsudden relief of abdominal pressure can lead to severe drop in blood pressure Open Procedure Cystectomy Ileal Conduit Cystectomy/Ileal Conduit Removal of bladder and diversion through a portion of the intestine Radical cystectomy-treats malignancies invading nearby tissues Male Bladder, prostate, seminal vesicles Female Bladder, urethra, anterior vaginal wall, uterus, fallopian tubes, ovaries Ileal conduit External appliance for collection of urine or Continent urinary reservoir (Koch pouch) made from reconfigured bowel 400-1200ml capacity Emptied by periodic catheterization of a stoma Radical cystectomy with Ileal conduit-continued Considerations -Major, bowel and long instrument sets, self retaining abdominal retractor, hemoclip appliers -Stoma supplies, bowel staplers, ureteral stents, ties on a pass, kitners, and sponge sticks -patient will have a bowel prep, foley -General surgeon will assist Procedure Midline abdominal incision #10 blade, bovie Expose bladder Moist laps and abdominal retractor Scissors and pickups May terminate here if tumor is too invasive Lymph nodes excised Pickups and scissors Frozen section Dissect bladder, vas, and vessels Bovie, hemoclips, long metz, long DeBakeys, long clamps, ties on a pass, sponge stick, kitners Clamp, clamp, cut, tie, tie Dissect and transect ureters Pick ups and scissors Frozen section for margins Procedure-continued Mobilize toward prostatic urethra care is taken to maintain erectile capability Remove Foley and transect urethra Large silk suture Remove bladder, control bleeding Pickups, scissors, bovie Pack with moist sponges Conduit procedure Divide 20 cm length of terminal ileum Intestinal clamps x2 Intestinal staplers Divide mesentery Clamp, clamp, cut, tie, tie Reanastomose remaining bowel and close mesentery Bowel staplers, long silk suture Implant ureters into segment of ileum Knife, suture of surgeon’s choice Stents Distal end of conduit makes stoma Skin knife, army-navys, suture Close incision Dressings and stoma bag Marshall-Marchetti-Krantz Bladder suspension Also called a Birch Women with significant urinary stress incontinence Post childbirth or aging Elevates bladder base, reduces redundant vaginal tissue, and fixes urethral angle Gynecologist-with vaginal or abdominal hysterectomy Procedure Phannenstiel incision #10 blade, bovie Blunt dissection of bladder and urethra Sponge stick, lap Metzenbaum, dressing forceps Assistant inserts 2 gloved fingers into vagina to elevate bladder Gloves, sleeve, towel around opening Bandage scissors to cut drape 4 heavy sutures are placed in the anterior vaginal wall by urethra and secured to pubis symphisis or Coopers ligament Haney needle holders, kellys to tag suture (leave untied and uncut) Tie suture sequentially then cut for optimal tension Close-may pack vagina Stamey Endoscopic attachment of bladder neck to rectus fascia using stamey needles Suture placement verified with cystoscope Done in conjunction with vaginal hysterectomy often 2 small super pubic incisions for stamey needles where suture is tied Each time scope is removed insert Foley catheter Sutures are tied sequentially for equal tension then cut Close small wounds Stamey Stamey-continued Circumcision Removal of the prepuce Newborns at parents request for religious or personal reasons or to repair phimosis Performed in the delivery room, newborn nursery, or physician’s office Minimal prep Bell Procedure Bell shaped device is placed over glans Foreskin is pulled taught over the bell Second part of bell device is place over the foreskin and tightened. Bell cuts off blood supply to prepuce and guides 15 blade as surgeon cuts Remove clamp and suture if necessary Callodian dressing or nonadherent dressing is used. Circumcision Procedure (no bell) Straight hemostat on posterior midline of foreskin several minutes to cut off blood supply Remove clamp and cut dorsal slit (15 blade) Circumferential freehand incision around shaft Raw edges are sewn together leaving glans exposed Nonadhearent dressing Orchiectomy/Orchiopexy Orchiectomy-removal of Orchiopexy-fixation of one or both testicles Radical-for testicular cancer one or both testicles in the scrotal sac Repairs Entire contents of hemiscrotum, tunica vaginalis, spermatic cord Inguinal incision Simple-abscess or prostate cancer Testis and epididymis Scrotal incision Testicular torsion Undescended testicle Scrotal incision Done bilaterally even if only one side is affected Orchiectomy Procedure Scrotal incision #15 blade, tension on scrotum Testis and spermatic cord are extruded through the wound Cord structures are separated and identified Metzenbaum and pickups Ligate cord structures Clamp, clamp, cut, tie, tie Testicular implant if desired Close Orchiopexy Scrotal incision #15 blade, tension on scrotum Enter tunica vaginalis Pickups and scissors Position testicle in scrotum Suture tunica albuginea to dartos muscle-2 lateral, one inferior Nonabsorbable suture Close Repeat on other side Hydrocelectomy Accumulation of fluid in tunica vaginalis due to trauma or infection Procedure Scrotal incision #15 blade Dissection to vaginalis Tenotomy scissors, Adson's with teeth Fluid is evacuated Scissors, Adson's, suction Excess tunica is excised Adson's and tenotomy scissors Close tunica and scrotum Dressing Fluffs and jockstrap Vericocelectomy Dilation of spermatic veins Blood pools and warms scrotal contents Can kill sperm reducing fertility Pain and swelling of scrotum Left side most common Can be done Open inguinal incision Microsurgery Laparoscope embolization Procedure Inguinal incision #10 blade, bovie Vein dissection Metzenbaum and pickups Ligate vein Clamp, clamp, cut, tie, tie Close Hypospadias Repair Usually done between ages 1-4 Done in 1 or 2 stages depending on difficulty Involves a glanuplasty, orthoplasty and urethroplasty Procedure Circumferential incision #15 blade Dissection of skin Pickups and scissors Close meatus Small suture Chordee repair Cut fibrous bands along entire penis Skin graft for urethral repair if needed Skin from penis wrapped around foley Small suture Close skin Insertion of Penile Prosthesis Treatment of male impotence Prosthesis Inflatable Semi rigid Place a foley to identify location of urethra Procedure Incision-base of penis to scrotum #15 blade Incise tunica albuginea of both corpora #15 blade Traction sutures 1 Silk Dilate corpora Hegar dilators Furlow inserter is used to measure length Advance prosthesis on both sides Keith needles through glans Place pump in scrotum following inguinal canal Fill reservoir with fluid Connect rods and reservoir Test Close Vasectomy To produce permanent sterility Usually done in doctor’s office Sterility is not immediate 15 ejaculations to remove residual sperm Reanastomosis occurs in less then 1% of cases Procedure Local Incision #15 blade Vas is isolated above the epididymis Penetrating towel clamp Wide ligation Clamp, clamp, cut, tie, tie Remove segment Fulgurate ends of remaining vas Bovie Close Vasectomy Vasovasotomy Vasectomy reversal Microscope or loupes Bilateral No intercourse for 1 month Semen analysis 50% conception rate Procedure Scrotal Incision #15 blade Excise scar tissue Micro scissors ad forceps Dilate lumens Anastimose ends of vas Micro suture, Castroviejo needle holders, pickups, scissors May stent Close scrotum Prostatectomy Instruments and supplies Major instruments Large retractor Long instruments Hemoclip appliers Bovie extender Foley KY jelly Suprapubic catheter IV indigo carmine is used to locate the ureters 3 methods Suprapubic-through bladder Retropubic-avoids bladder Perineal-potential of impotence and rectal injury Procedure Pfannenstiel incision #10 blade Dissect bladder from peritoneum Kitners, sponge stick Enter bladder “Deep” knife Remove foley and incise base of bladder Long handle #10 blade Blunt dissection of prostate Tumor is removed via bladder Hemostasis Suture, tie on a pass, bovie, hemoclips Reinsert foley Close bladder Drain and close skin Prostatectomy TURP Transuretheral Resection of the Prostate Watch for pt. jerking Electrical stimulation to nerves Hemoorhage Ready to move to open Perforation TURP syndrome TURP