Eyes
advertisement
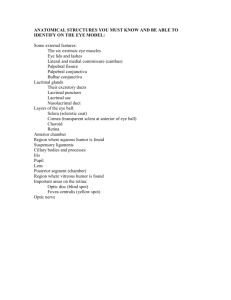
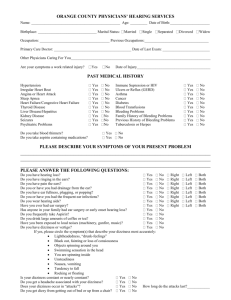
Assessment of Eyes and Ears Eye Anatomy – Why Study It? Why should you care? Optometrist – Doctor of optometry, 4 year undergrad + 4 year optometry school Ophthalmologists – Medical doctors In general, optometrists practice primary and preventive eye care, while ophthalmologists perform eye surgery What do nurses do? History Vision difficulty? Eye pain? Photophobia – inability to tolerate light Childhood strabismus? Halos around lights – in glaucoma Scotoma – blind spot in visual field – in glaucoma, optic nerve, and visual pathway disorder Night blindness – Vit A deficiency, glaucoma, A history of crossed eyes? AKA “lazy eye” Redness or swelling? Infections? History cont. Excessive or lack of tearing? May be due to irritants or obstruction in drainage Past history of ocular problems? Glaucoma? Family history? Use of glasses or contact lenses? When tested last? Any medications? Anatomy of Eyelid Eyelids (L. palpebrae) protect the cornea and eyeball from injury Canthi (sing. canthus) are corners of the eye, also called angles of eye Caruncle is located near medial canthus and contains sebaceous glands Tarsal plates are made of connective tissue and strengthen eyelid. They contain meibomian (tarsal) glands which secrete lipid to create airtight seal when closed and also prevent eyelids from sticking together Inspecting External Ocular Structures General Eyebrows Note if facial expression is relax or tense Note if movement is symmetrical Eyelids and lashes Note if any redness, swelling, discharge or lesions Note if eyelid closes completely and if drooping Pallor of lower lid is good indicator of anemia For upper eyelid, use applicator stick to fold the eyelid over Abnormalities in Eyelids Ectropion Lower lid rolls out, causing an increase in tearing The eyes feel dry and itchy due to inappropriate itching Increase risk for inflammation Occurs mostly in elderly due to atrophy of elastic tissue Entropion The lower lid rolls in Foreign body sensation Abnormalities in Eyelids Periorbital edema May occur with local infection or systemic condition Ptosis Occurs with neuromuscular weakness (myasthenia gravis) or CN III damage Lesions on the Eyelids Blepharitis Chalazion Inflammation of eyelids Staph or dermatitis Burning, itching, tearing, foreign body sensation, pain A cyst in or an infection of meibomian gland Nontender, firm, overlying skin freely movable Hordeolum (Stye) Localized Staph infection of hair follicle at lid margin Painful, red, swollen, purulent Anatomy of the Eye Lacrimal apparatus provides irrigation of conjunctiva glands – secrete lacrimal fluid (tears) Lacrimal ducts – lacrimal fluid to conjunctiva Lacrimal canaliculi (puncti) – drain fluid into Nasolacrimal duct – conveys lacrimal fluid to nasal cavity Lacrimal Inspecting the Lacrimal Apparatus Inspect for bulges or pressure near canaliculi Dacryocystitis Inflammation of the lacrimal sac and/or nasolacrimal duct Dacryoadenitis Infection of lacrimal gland Dacryoadenitis Dacryocystitis Anatomy of Extraocular Muscles 4 rectus (straight) 2 oblique Innervations SO4 – Superior oblique m. LR6 – Lateral rectus m. CN IV (trochlear n.) CN VI (abducens n.) AO3 – All other muscles CN III ( Trigeminal n.) Extraocular muscle movement Extraocular Muscle Dysfunction Anatomy of the Eyeball – Outer Layer Sclera – tough protective white covering (posterior 5/6) Cornea – transparent part of the fibrous coat covering the anterior of the eyeball (anterior 1/5) Conjunctiva – transparent protective covering of exposed part of eye (palpebral conjunctiva covers inside of eyelash) iris Corneal reflex – lightly touching the eye with cotton stimulates a blink. Trigeminal n. (afferent) Facial n. (efferent) Inspection Conjunctiva Sliding the lower lids down, observe for redness on conjunctiva and if eyeball looks moist and glossy Reddening may be pathogenic Sclera Should be white, although may have gray-blue hue Might contain yellowish fatty deposits beneath the lids Yellowing of sclera indicates jaundice Vascular Disorders of Eye Conjunctivitis “Pink eye” Due to bacterial, viral, allergic, or chemical irritation Redness throughout the conjunctiva, but usually clear around the iris Purulent discharge usually common Symptoms: itching, burning, foreign body sensation Iritis Red halo around the iris and cornea Pupils may be irregular due to swelling Symptoms: photophobia, blurred vision, throbbing pain Inspecting Cornea and Lens Corneal abrasion Assess by shining a light and observing from the side Pupillary light reflex Charted according to size of pupil Charted as a ratio of before light/after light (3/1) A sluggish response may be caused by increased ICP No response may indicate neurological damage How to chart pupillary light reflex? PERRLA: Pupils Equal, Round, React to Light and Accommodation Anatomy of the Eyeball – Middle Layer Canal of Schlemm Choroid – provides vascularity to retina Pupil – variable-sized, black circular or slit shaped opening in the center of the iris that regulates the amount of light that enters the eye. Appears black because most of the light entering the pupil is absorbed by the tissues inside the eye. Lens – biconvex disc controlled by the ciliary muscle to produce far vision when flat Anterior chamber Aqueous humor is produced by the ciliary body and secreted into posterior chamber of eye. From there, aqueous humor travels to the anterior chamber where it exits through the Canal of Schlemm Determines intraocular pressure Increase leads to Glaucoma Vascular Disorders of Eye Physiology review: Aqueous humor is produced by the ciliary body and secreted into posterior chamber of eye. From there, aqueous humor travels to the anterior chamber where it exits through the Canal of Schlemm Glaucoma Excessive pressure in eye due to blockage of outflow from anterior chamber This puts pressure on optic nerve Redness around the iris, dilated pupils Symptoms: sudden clouding of vision, sudden eye pain, and halos around lights Disorders of Opacity of Lens Cataract Anatomy of the Eyeball – Inner Layer Retina – visually receptive layer where light waves are changed to nerve impulses Optic disc – area where the optic nerve enters the eyeball Fovea centralis – area of most acute vision Inspecting the Ocular Fundus Using an ophthalmoscope to inspect the internal surface of the retina, anterior chamber, lens, and vitreous. Darken the room to dilate the pupils Remove eye glasses, contacts may stay in Ask person to stare at distant object Hold ophthalmoscope close to your eye and move to within a few inches of the person’s face A red glow filling the pupil is called the red reflex and is caused by light reflecting off the retina Cataracts appear as opaque black areas against the red reflex Inspecting the Optic Disc and Retina Normal optic disc is: Yellow-orange to pink Round or oval Distinct margins Normal retina is: Arteries in each quadrant Arteries are bright red Visual pathways Testing Visual Reflexes Pupillary light reflex Constriction of pupils when bright light shines on the retina Direct light reflex – constriction of same sided pupil Consensual light reflex – simultaneous constriction of both pupils The impulse is carried afferently by CN II and efferently by CN III Accommodation Adaptation of eye for near vision Ask person to focus on distant object (dilates the pupils). Then ask person to shift gaze to near object few inches away. A normal response is pupillary constriction and convergence of axes of the eyes Testing Visual Accuity Snellen Eye Chart Standing 20 feet from the chart Test one eye at a time by covering the other eye Leave contact lenses and glasses on, unless the glasses are reading glasses Normal vision is 20/20 Near vision Use Jaeger card (smaller version of Snellen chart) or just read newspaper Testing Visual Fields Confrontation test Measures peripheral vision compared to examiner (assuming examiner’s vision is normal) Both examiner and pt cover one eye with a card, stand about 2 feet away, and maintain eye contact Advance finger, starting from periphery, and ask patient to say “now” when the finger is first visible Inability to see when the examiner sees suggests peripheral field loss Testing Ocular Muscle Function Cover Test Detects deviated alignment of eyes Ask pt. to stare straight at your nose and cover one of the pt.’s eyes with a card While noting the uncovered eye, move away the card A normal response is a steady fixed gaze Diagnostic Position Test Ask pt. to hold head straight and move finger in all positions, holding it about 12 inches away A normal response is parallel tracking of the objects with both eyes Nystagmus Fine oscillating movements around the iris Normal at extreme lateral gaze Developmental Considerations – Infants and Children Strabismus – must be detected and treated early to prevent permanent disability Esotropia – inward turning of eye Exotropia – outward turning of eye Color vision – due to inherited Xlinked recessive trait, occurs more often in boys External eye structures – an upward lateral slope together with epicanthal folds occurs in Down syndrome Ophthalmia neonatum – conjunctivitis due to bacteria, virus, or chemical irritation Developmental Considerations – Aging Decrease in visual acuity, diminished peripheral vision Ectropion (drooping of lower lid) or entropion (eyelids turning in) Pinguecula – yellow nodules due to thickening of conjunctiva as a result of prolonged exposure to sun, wind, and dust Developmental Considerations Aging Arcus senilis – graywhite arc seen around the cornea. Due to deposition of lipids. No effect on vision Xanthelasma – raised yellow plaques. Normal Ear Anatomy Ear Physiology External Ear External auditory meatus funnels sound waves, which reflect off the tympanic membrane to produce vibrations Cerumen (ear wax) protects the tympanic membrane from foreign substances Middle ear Malleus, incus, and stapes and eustachian tube Function to: Conduct sound vibrations from tympanic membrane (outer ear) to cochlea (inner ear) Protect the cochlea by reducing the amplitude of sounds Eustachian tube allows equalization of air pressure Inner ear Vestibule and semicircular canals Allow brain to sense body position and relation of angle of head to gravity Cochlea Transfers vibrations from stapes into nerve impulses The outer ear catches the waves of sound and funnels them down the ear canal (about an inch long) and flush up against the ear drum. The ear drum (tympanic membrane) is the boundary between the outer ear and the middle ear. In the middle ear, the malleus picks up the vibrations from the eardrum, passes them to the incus which then passes them to the stapes. The stapes terminates in a tiny footplate that fits precisely into the contact point or window of the inner ear. The window of the inner ear is the contact point of the cochlea. The vibrations set up rolling waves in the cochlear fluid which stimulate different areas of the membrane, which rubs against specialized cells called hair cells. This friction creates electrical impulses transmitted by the cochlear nerve. CN VIII is responsible for signal transduction from vestibule and cochlea to the brainstem. From brainstem, a signal is sent to the cerebral cortex to interpret the sound. Hearing Loss Conductive Mechanical dysfunction of external or middle ear Partial hearing loss May be caused by impacted cerumen, foreign bodies, perforated tympanic membrane, pus or serum in middle ear, or otosclerosis (hardening of stapes) May be fixed Sensorineural Dysfunction of inner ear, CN VIII, or cerebral cortex Cannot be fixed Developmental Considerations Infants Greater risk for otitis media (middle ear infections) due to shorter eustachian tube Aging Cilia lining ear canal become coarse and stiff, impeding sound waves Cerumen more common Dry cerumen – gray and flaky. More common in Asians and Native Americans Wet cerumen – brown and moist. More common in whites and blacks Presbycusis - degenerative sensorineural hearing loss Auditory reaction time increases Obtaining History Earaches? (otalgia) Location, character, intensity, associative and alleviating factors May be directly due to ear disease or maybe referred pain from a problem in teeth or oropharynx Infections? A viral or bacterial upper respiratory infection may migrate up the eustachian tube and involve the middle ear Frequency? Occurred in childhood? Discharge? (otorrhea) May suggest infection or perforated eardrum Typically with perforation, ear pain drainage Otitis externa – purulent, sanguineous, or watery Acute otitis media with perforation – purulent discharge More History Trouble hearing? Gradual our sudden? Ringing in ears? (tinnitus) Some are ototoxic Vertigo? (spinning) May be a result of medication Medications? Presbycusis – gradual sensorineural hearing impairment in the elderly Hearing loss due to trauma is often sudden Subjective – person feels like he or she spins Objective – person feels like room spins Environmental noise Noise-induced hearing loss Lesions of External Ear Otitis Externa Gouty Tophi Assessing External Ear Size and Shape Skin conditions normal is 4-10cm tall Note edema, inflammation, lesions Tenderness Location? Pain in pinna indicates otitis externa Pain at mastoid process indicates mastoiditis or lymphadenitis External Auditory Meatus Atresia – absence or closure of ear canal Otitis externa may cause purulent discharge Otitis media may cause rupture of tympanic membrane If drainage present following trauma, possible basal skull fracture. Perform glucose test (CSF (+) for glucose). Inspecting Using Otoscope Pull the pinna up and back in adult, straight down in children under 3 years Hold otoscope upside down and place dorsal side of hand along person’s cheek Insert speculum slowly and avoid touching the inner section of canal wall, which is sensitive and may cause pain. Inspecting the External Canal Note any redness or swelling, lesions, or foreign bodies If discharge present, note color and odor Otitis Externa Inspecting the Tympanic Membrane Normal is shiny and translucent Flat, slightly pulled in at the center Valsalva maneuver causes tympanic membrane to flutter, used to assess drum mobility Which tympanic membrane is perforated? Testing Hearing Acuity Voice test Whisper two syllable words into one of the person’s ears, while covering the other one. Ask person to repeat what you’ve said. Tuning fork tests Measure hearing by air conduction or bone conduction Weber test Rinne test Weber Test Tuning fork is struck and placed on head or forehead, equal distance from both ears Used to determine if hearing loss is more extensive in one ear than the other This test cannot confirm normal hearing, because hearing defects affecting both ears equally will produce an apparently normal test result Rinne Test Compares air conduction and bone conduction Place stem of vibrating fork on mastoid process and ask when sound goes away Quickly invert the fork so the vibrating end is near the ear canal. The person should still hear a sound Normally the sound is heard longer by air conduction rather than bone conduction In conductive hearing loss, sound heard longer by bone conduction Normal Hearing Conductive Hearing Loss Sensorineural Hearing Loss Infants and Children Save otoscopic examination until the end May help to show otoscope to child and let him or her play with it Stabilize (or ask a parent for help) the child’s head in order to prevent movement Pull pinna straight down In infants, the tympanic membrane may look thick and opaque after first few days or after crying Tympanostomy tubes may be in place if drainage occurs as a result of otitis media Abnormalities in the Ear Canal Acute Otitis Media Otitis Externa Excessive Cerumen