Chapter 26 - FacultyWeb
advertisement

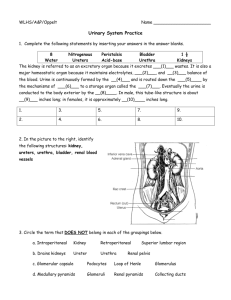
Which structures exit at the hilum of the kidney? 1. 2. 3. 4. Renal artery and nerves Renal vein and ureter Renal capsule and renal sinus 1 and 2 are correct Where does urine production begin? 1. 2. 3. 4. Renal artery Minor calyces Nephron Collecting duct How are cortical and juxtamedullary nephrons structurally different? 1. Cortical nephrons are surrounded by vasa recta. 2. Cortical nephrons have very short PCTs. 3. Juxtamedullary nephrons have longer loops of Henle. 4. All of the above are differences. Which portion of a nephron is not in the renal cortex? 1. 2. 3. 4. Proximal convoluted tubule Distal convoluted tubule Collecting duct Loop of Henle Why don’t plasma proteins pass into the capsular space under normal circumstances? 1. 2. 3. 4. Glomerular capillary pores are too small. Glomerular blood pressure is too low. Glomerular filtration rate is too low. Glomerular blood flow is too slow. Damage to which part of the nephron interferes with hormonal control of blood pressure? 1. 2. 3. 4. Bowman’s capsule Juxtaglomerular apparatus PCT Loop of Henle What is the composition of the filtrate in the capsular space? 1. 2. 3. 4. Like urine, only more concentrated Similar to water Like urine, only less concentrated Similar to plasma, only no proteins Why is the presence of microvilli important to the epithelial tissue of the PCT? 1. Because reabsorption is occurring 2. Because filtration is occurring 3. Because secretion of toxins and ions is occurring 4. Because urine elimination is occurring How does the diameter of the lumen of the loop of Henle change along its length? 1. The lumen is widest near the PCT. 2. The lumen is the same diameter along its length. 3. The lumen is narrower where water reabsorption is occurring. 4. None of these is correct. What event occurs when the plasma concentration of a substance exceeds its tubular maximum? 1. 2. 3. 4. Glomerular blood pressure increases. Filtration shuts down. Excess is excreted in urine. Glomerular osmotic pressure decreases. Why are glomerular pressures higher than pressure in other capillaries? 1. The efferent arteriole has a smaller diameter than the afferent arteriole, increasing resistance. 2. Sodium content of the filtrate increases pressure. 3. E and NE cause increased glomerular pressure. 4. The length of the afferent arteriole is longer than the efferent arteriole. What nephron structures are involved in filtration? 1. PCT, lamina densa, and descending loop of Henle 2. Filtration slits of the podocytes and PCT 3. Glomerular capillaries, lamina densa, and filtration slits of the podocytes 4. Glomerular capillaries and PCT What is the role of capsular hydrostatic pressure (CsHP)? 1. Pushes water and solutes out of plasma into the filtrate 2. Draws water out of the filtrate and into plasma 3. Pushes water and solutes out of filtrate into plasma 4. Regulates blood pressure What direct affect does sympathetic activation have on GFR? 1. Produces powerful vasoconstriction of the afferent arteriole 2. Metabolic waste buildup 3. Dilation of the afferent arteriole 4. Dilation of glomerular capillaries and constriction of the efferent arteriole All of the following except ____ are effects of angiotensin II. 1. Elevation of glomerular pressures and GFR 2. Inhibition of ADH release 3. Elevation of arterial pressure throughout the body 4. Stimulation of NA reabsorption in the DCT What effect does an increased amount of aldosterone have on K+ concentration of urine? 1. 2. 3. 4. K+ increases K+ decreases No effect Impossible to predict What effect does decreased Na+ concentration of filtrate have on the pH of tubular fluid? 1. 2. 3. 4. Tubular fluid pH will be higher Tubular fluid pH will be lower There is not an effect on pH Tubular fluid neutral, pH 7 How would the absence of juxtamedullary nephrons affect the volume of urine and its osmotic concentration? 1. 2. 3. 4. Decrease volume; decrease osmotic concentration Decrease volume; increase osmotic concentration Increase volume; decrease osmotic concentration Increase volume; increase osmotic concentration Where is concentration of urine the greatest? Why? 1. In the PCT/the PCT is where most reabsorption is occurring 2. In the medulla/concentrating mechanism relies on osmosis 3. In the DCT/water diffuses out 4. The glomerulus/it has highest concentration of solutes Why does a decrease in Na+ in the distal convoluted tubule lead to an increase in blood pressure? 1. 2. 3. 4. Because it decreases water content in blood Because it increases renin production Because it increases filtration rate Because it increases water loss through kidneys Why does osmotic concentration decrease in the thick ascending limb of the loop of Henle? 1. Urea is transported out of the tubule. 2. Na+ and Cl- are actively transported out of the tubular fluid. 3. The thick ascending limb is permeable to water. 4. 1 and 2 are correct. What is the role of the vasa recta in the urinary system? 1. Increasing specific gravity of urine 2. Increasing the osmotic concentration of urine 3. Returning water and solutes to general circulation 4. Cleansing blood before it reenters systemic circulation Mary has had a urinalysis that indicates a high level of bilirubin. What condition may she have? 1. 2. 3. 4. Liver disease Anorexia Ketonuria Renal infection What effect does eating a high-protein diet have on the composition of urine? 1. 2. 3. 4. Increased urea Increased potassium Increased fluid volume 1 and 3 are correct An obstruction of a ureter by a kidney stone limits the flow of urine between which two points? 1. 2. 3. 4. Ureter and urethra Renal medulla and renal pelvis Renal medulla and urethra Renal pelvis and urinary bladder The ability to control the micturition reflex depends on the ability to control which muscle? 1. 2. 3. 4. Urogenital diaphragm Internal urinary sphincter External urinary sphincter Coccygeus