Pancreas: Anatomy & Physiology - bushelman-hap
advertisement
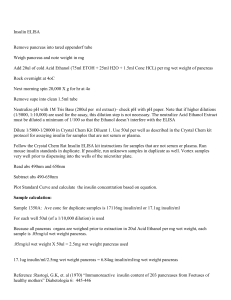
Pancreas: Anatomy & Physiology Pancreas- Brief History • Pancreas – derived from the Greek pan, “all”, and kreas, “flesh”, probably referring to the organ’s homogenous appearance • Herophilus, Greek anatomist and Surgeon, first identified the pancreas in 335 – 280 BC • Ruphos, another Greek anatomist, gave pancreas its name after few hundred years • Wirsung discovered the pancreatic duct in 1642. • Pancreas as a secretory gland was investigated by Graaf in 1671. Pancreas • Gland with both exocrine and endocrine functions • 6-10 inch in length (15-25 cm) • 60-100 gram in weight • Location: retro-peritoneum, 2nd lumbar vertebral level • Extends in an oblique, transverse position • Parts of pancreas: head, neck, body and tail Histology • There are two distinct organ systems within the pancreas • The endocrine portion of the pancreas is served by structures called the islet of Langerhans o The islet of Langerhans have several distinct cell types • Alpha cells-produce glucagon and constitute approximate 25% of the total islet cell number • Beta cells-the insulin producing cells (majority of the cells) • Delta cells-produce somatostatin (smallest number) • The exocrine portion of the pancreas is made up of acini and ductal systems o Acinar cells contain zymogen Anatomy • Is a retroperitoneal structure found posterior to the stomach and lesser omentum • It has a distinctive yellow/tan/pink color and is multilobulated • The gland is divided into four portions o o o o The head The neck The body The tail • The pancreas has an extensive arterial system arising from multiple sources • The venous drainage parallels arterial anatomy o The veins terminate in the portal vein • Multiple lymph nodes drain the pancreas • Neural function is controlled by duel sympathetic and parasympathetic innervation Pancreas Head of Pancreas • Includes uncinate process: Lower part of the posterior surface of the head that wraps behind the superior mesenteric artery and superior mesenteric vein • • • • • Flattened structure, 2 – 3 cm thick Attached to the 2nd and 3rd portions of duodenum on the right Emerges into neck on the left Border b/w head & neck is determined by GDA insertion SPDA and IPDA anastamose b/w the duodenum and the rt. lateral border • Broadest part • Moulded into the C shaped concavity of duodenum • Lies over the inferior venacava, the right and left renal veins at the level of L2 • Posterior surface is indented by the terminal part of the bile duct Neck of Pancreas • 2.5 cm in length • Lies in front of the superior mesenteric and portal veins • Posteriorly, mostly no branches to pancreas Body of Pancreas • Elongated structure • Anterior surface, separated from stomach by lesser sac • Posterior surface, related to aorta, lt. adrenal gland, lt. renal vessels and upper 1/3rd of lt. kidney • Splenic vein runs embedded in the post. Surface • Inferior surface is covered by tran. Mesocolon • Body passes across the left renal vein and aorta, left crus of diaphragm, left psoas muscle, lower pole of left suprarenal gland to the hilum of left kidney • Upper border crosses the aorta at the origin of the celiac trunk • Splenic artery passes to the left along the upper border • Lower border crosses the origin of the superior mesenteric artery Pancreas Tail of Pancreas • Narrow, short segment • Lies at the level of the 12th thoracic vertebra • Lies in the lienorenal ligament along with splenic artery, vein, lymphatics • End of tail of pancreas touches the hilum of spleen • Anteriorly, close to splenic flexure of colon • May be injured during splenectomy (fistula) • Passes forward from the anterior surface of the left kidney at the level of hilum Pancreatic Duct • Main duct (Duct of Wirsung) runs the entire length of pancreas o Joins Central Bile Duct at the ampulla of Vater o 2 – 4 mm in diameter, 20 secondary branches • Lesser duct (Duct of Santorini) drains superior portion of head and empties separately into 2nd portion of duodenum o Drains the uncinate process and lower part of head Pancreatic Physiology • Exocrine pancreas 85% of the volume of the gland • Extracellular matrix – 10% • Blood vessels and ducts - 4% • Endocrine pancreas – 1% Histology-Exocrine Pancreas • 2 major components o Acinar cells which secrete primarily digestive enzymes o Centroacinar or ductal cells which secrete fluids and electrolytes • Constitute 80% to 90% of the pancreatic mass • Acinar cells secrete the digestive enzymes • 20 to 40 acinar cells coalesce into a unit called the acinus • Centroacinar cell (2nd cell type in the acinus) is responsible for fluid and electrolyte secretion by the pancreas • Duct system - network of conduits that carry the exocrine secretions into the duodenum Histology-Endocrine Pancreas • Accounts for only 2% of the pancreatic mass • Nests of cells - islets of Langerhans • Four major cell types o o o o Alpha (A) cells secrete glucagon Beta (B) cells secrete insulin Delta (D) cells secrete somatostatin F cells secrete pancreatic polypeptide Histology-Endocrine Pancreas • B cells are centrally located within the islet and constitute 70% of the islet mass • PP, A, and D cells are located at the periphery of the islet Physiology – Exocrine Pancreas • Secretion of water and electrolytes originates in the centroacinar and intercalated duct cells • Pancreatic enzymes originate in the acinar cells • Final product is a colorless, odorless, and isosmotic alkaline fluid that contains digestive enzymes (amylase, lipase, and trypsinogen) • Alkaline pH results from secreted bicarbonate which serves to neutralize gastric acid and regulate the pH of the intestine • Enzymes digest carbohydrates, proteins, and fats Exocrine • The bulk of the pancreas is an exocrine gland secreting pancreatic fluid into the duodenum after a meal. • The principal stimulant of pancreatic water and electrolyte secretion – Secretin • Secretin is synthesized in the S cells of the crypts of Liberkuhn • Released into the blood stream in the presence of luminal acid and bile Bicarbonate Secretion • Bicarbonate is formed from carbonic acid by the enzyme carbonic anhydrase • Major stimulants Secretin, Cholecystokinin, Gastrin, Acetylcholine • Major inhibitors Atropine, Somatostatin, Pancreatic polypeptide and Glucagon • Secretin - released from the duodenal mucosa in response to a duodenal luminal pH < 3 Enzymes: Types and Secretion • Amylase o only digestive enzyme secreted by pancreas in active form o hydrolyzes starch and glycogen to glucose, maltose, maltotriose, and dextrins • Lipase o emulsify and hydrolyze fat in the presence of bile salts • Proteases o o o o essential for protein digestion secreted as proenzymes; require activation for proteolytic activity duodenal enzyme, enterokinase, converts trypsinogen to trypsin Trypsin, in turn, activates chymotrypsin, elastase, carboxypeptidase, and phospholipase • Released from the acinar cells into the lumen of the acinus and then transported into the duodenal lumen, where the enzymes are activated. • Ultimate result of all these actions is food digestion and absorption Physiology – Endocrine Pancreas • Principal function is to maintain glucose homeostasis • Insulin and glucagon play a major role in glucose homeostasis • In addition endocrine pancreas secrete somatostatin, pancreatic polypeptide, c peptide, & amylin • pancreatic polypeptide – released internally to selfregulate pancreas activities • amylin – released with insulin; contributes to glycemic control Insulin • Synthesized in the beta cells of the islets of Langerhans • 80% of the islet cell mass must be surgically removed before diabetes becomes clinically apparent • Insulin and C peptide are packaged into secretory granules and released together into the cytoplasm • 95% belong to reserve pool and 5% stored in readily releasable pool • Thus small amount of insulin is released under maximum stimulatory conditions Insulin • Major stimulants o Glucose, amino acids, glucagon, GIP, CCK, sulfonylurea compounds, β-Sympathetic fibers • Major inhibitors o somatostatin, amylin, pancreastatin, α-sympathetic fibers • Stimulation of Beta cells results in exocytosis of the secretory granules o Equal amount of insulin and c peptide are released into circulation o o o o Insulin circulates in free form and has half life of 4-8 minutes Liver predominantly degrades insulin C peptide is not readily degraded in the liver Half life of c peptide averages 35 minutes Glucagon • Secreted by the alpha cells of the islets of Langerhans • Major stimulants o Amino acids, Cholinergic fibers, β-Sympathetic fibers • Major inhibitors o Glucose, insulin, somatostatin, α-sympathetic fibers • Main physiological role o increase blood glucose level through stimulation of glycogenolysis and gluconeogenesis • Antagonistic effect on insulin action • Release is inhibited by hyperglycemia and stimulated by hypoglycemia Somatostatin • Secreted by the delta cells of the islets of Langerhans • Major Stimulants o High fat, protein rich , high carbohydrate meal • Generalized inhibitory effect o Inhibits the release of growth hormone o Inhibits the release of almost all peptide hormones o Inhibits gastric, pancreatic, and biliary secretion • Used to treat both endocrine and exocrine disorders Diseases and Disorders • Acute Pancreatitis – Includes a broad spectrum of pancreatic disease o Varies from mild parenchymal edema to severe hemorrhagic pancreatitis associated with gangrene and necrosis • Chronic Pancreatitis o Is associated with alcohol abuse (most common), cystic fibrosis, congenital anomalies of pancreatic duct and trauma to the pancreas • Disruptions of the Pancreatic Duct o In adults, the most common cause is alcoholic pancreatitis o In children the most common cause is neoplasms. (tumors) • The fifth most common cause of cancer death • 90% of patients die within the first year after diagnosis • Adenocarcinoma of the Body and Tail of Pancreas o Represents up to 30% of all cases of pancreatic carcinoma Diseases and Disorders • Endocrine Tumors – Rare with an incidence of five per one million o Insulinoma: Most common endocrine tumor of the pancreas • Gastrinoma (Zollinger-Ellison Syndrome) o Identification of a islet cell tumor of the pancreas o Patient management is through control of gastric acid hypersecretion • Pancreatic Lymphoma o Involvement of pancreas with non-Hodgkin’s lymphoma is an unusual neoplasm • Pancreatic Trauma o Pancreas is injured in less than 2% of patients with abdominal trauma Diseases and Disorders • Diabetes Mellitus o Group of diseases characterized by high levels of blood glucose resulting from defects in insulin production, insulin action, or both o Leads to Hyperglycemia, or high blood glucose (sugar) • Estimated 20.8 million in US ( 7% of population) • Estimated 14.6 million diagnosed (only 2/3) • Consists of 3 types: 1) Type 1 diabetes 2) Type 2 diabetes 3) Gestational diabetes http://faculty.smu.edu/jbuynak/images/Diabetes MellitusBuynak.ppt Diabetes Mellitus • Type 1 Diabetes (insulin-dependent diabetes) o cells that produce insulin are destroyed o results in insulin dependence o commonly detected before age 30 • Type 2 Diabetes (non-insulin-dependent diabetes) o blood glucose levels rise due to 1) Lack of insulin production 2) Insufficient insulin action (resistant cells) o commonly detected after age 40 o effects > 90% of persons with diabetes o eventually leads to beta cell failure (resulting in insulin dependence) • Gestational Diabetes o 3-5% of pregnant women in the US develop gestational diabetes http://faculty.smu.edu/jbuynak/images/Diabetes MellitusBuynak.ppt Conclusions • Pancreas is a composite gland o Has exocrine and endocrine functions • Plays major role in digestion and glucose homeostasis