Hiatal Hernia Case Study
advertisement

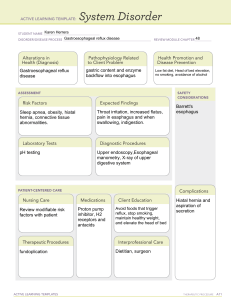
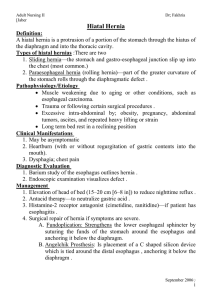
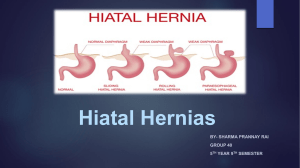
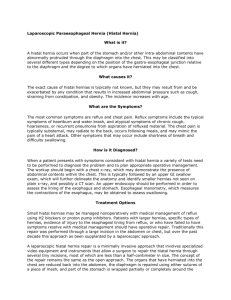
HIATAL HERNIA CASE STUDY By Sally Smith Pathophysiology 5/2010 SYMPTOMS & HISTORY A 56 y/o male c/o experiencing pain about an inch beneath his sternum and sharp pains in radiating towards his left shoulder. It varies in intensity and is increased immediately after eating spicy foods. After most meals, he c/o suffering from mild heartburn. His PCP initially prescribed a two week course of Omeprazole, which alleviated the symptoms, but they returned after a few days. PHYSICAL FINDINGS The physical examination does not disclose any strong evidence. The patient is obese, lacks regular physical activities and poor diet. All other findings are within normal limits DIAGNOSTIC METHODS (X-RAY) Although a chest radiograph may reveal a large hiatal hernia (and many incidentally diagnosed hiatal hernias are discovered in this manner), a barium study of the esophagus helps establish the diagnosis with greater accuracy . DIAGNOSTIC METHODS (X-RAY) Typical findings include: An outpouching of barium at the lower end of the esophagus A wide hiatus through which gastric folds are seen in continuum with those in the stomach And occasionally, free reflux of barium. OTHER POSSIBLE DIAGNOSIS If it is not a hiatal hernia, there could be a mass obstructing the area and causing pain. Heart work up would be done first to r/o any cardiac issues. TREATMENT OPTIONS The goals of treatment are to relieve symptoms and prevent further complications. Reducing the gastroesophageal reflux will relieve pain. Medications may be prescribed, which this patient has already used. Other measures to reduce symptoms include: Avoiding large or heavy meals Not lying down or bending over immediately after a meal Reducing weight and not smoking If these measures fail to control the symptoms, or complications occur, surgical repair of the hernia may be necessary. PROGNOSIS Most symptoms are alleviated with treatment so prognosis is excellent. Chronic untreated GERD can cause serious complications. Inflammation of the esophagus from refluxed stomach acid can damage the lining and cause bleeding or ulcers—also called esophagitis. Scars from tissue damage can lead to strictures—narrowing of the esophagus—that make swallowing difficult. Some people develop Barrett’s esophagus, in which cells in the esophageal lining take on an abnormal shape and color. Over time, the cells can lead to esophageal cancer, which is often fatal. Persons with GERD and its complications should be monitored closely by a physician. Studies have shown that GERD may worsen or contribute to asthma, chronic cough, and pulmonary fibrosis. This may be due to chronic aspiration. DISEASE CHANGES FOR DIFFERENT AGE GROUPS Hiatal hernias are common in people over 50 years old. They can occur in pediatrics, but not very often. If they do, treatments are the same as for adults. Infants with symptoms are placed prone with elevation of the head at least 30 degrees to reduce the possibility of aspiration. RESOURCES Allison PR. Reflux esophagitis, sliding hiatal hernia, and the anatomy of repair. Surg Gynecol Obstet. 1951 Apr;92(4):419–431. Bettex M, Kuffer F. Long-term results of fundoplication in hiatus hernia and cardio-esophageal chalasia in infants and children. Report of 112 consecutive cases. J Pediatr Surg. 1969 Oct;4(5):526– 530. Borema I, Germs R. Fixation of the lesser curvature of the stomach to the anterior abdominal wall after reposition of the hernia through the oesophageal hiatus. Arch Chir Neerl. 1955;7(4):351–359. Orlando RC. Diseases of the esophagus. In: Goldman L, Ausiello D, eds. Cecil Medicine. 23rd ed. Philadelphia, Pa: Saunders Elsevier; 2007:chap 140.