Confidentiality: Ethical and Legal Issues
advertisement

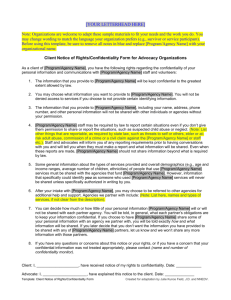
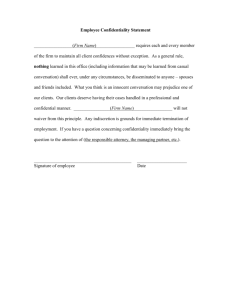
Confidentiality: Ethical and Legal Issues Chapter Six Introduction You cannot make a blanket promise to your clients that everything they talk about will always remain confidential. The more you consider the legal ramifications of confidentiality, the clearer it becomes that most matters are not neatly defined. Professional judgment always plays a significant role in resolving cases, from both an ethical and a legal perspective. Confidentiality As a general rule, psychotherapists are prohibited from disclosing confidential communications to any third party unless mandated or permitted by law to do so. Therapists are advised to err on the side of being overly cautious in protecting the confidentiality of their clients, unless faced with a mandatory exception to confidentiality such as reporting child abuse or elder abuse. Confidentiality continued Counselors MUST obtain client consent before engaging in advocacy on behalf of an identifiable client. Privileged Communication Privileged communication is a legal concept that generally bars the disclosure of confidential communications in a legal proceeding. All states have enacted into law some form of psychotherapist-client privilege, but the specifics of this privilege vary from state to state. Privileged Communication continued Generally speaking, this legal concept does NOT apply to group counseling, couples counseling, marital and family therapy, or child and adolescent therapy. No clear judicial trend has emerged for communications that are made in the presence of third persons. It is best for therapists to assume that such communications are not privileged by law. Privacy Privacy, as a matter of law, refers to the constitutional right of an individual to decide the time, place, manner, and extent of sharing oneself with others. According to Nagy (2005), you must not reveal identifying information about clients, orally or in writing, or even the fact that they consult you, without their formal consent. Confidentiality and Privacy in a School Setting In some states, therapists in private practice are required to demonstrate that attempts have been made to contact the parents of children who are younger than 16, whereas school counselors are not required to do so. Counselors working in schools are NOT required by the Family Educational rights and Privacy Act of 1994 (FERPA) to make their personal records available or to disclose the substance of confidential counseling sessions to parents. Ethical & Legal Ramifications of Confidentiality and Privileged Communication No genuine therapy can occur unless clients trust that what they say is confidential. When it is necessary to break confidentiality, it is a good practice to inform the client of the intention to take this action and also to invite the client to participate in the process. Mandatory reporting is designed to encourage reporting of any suspected cases of child, elder, or dependent-adult abuse. Exceptions to Confidentiality and Privileged Communication All of the major professional organizations have taken the position that practitioners must reveal certain information when there is clear and imminent danger to an individual or to society. It is the responsibility of the therapists to clarify the ethical and legal restrictions on confidentiality. Unless clients understand the exceptions to confidentiality, their consent to treatment is not genuinely informed. Privacy Issue with Telecommunication Devices It is the counselor’s responsibility to make sure fax and email transmissions arrive in a secured environment in such a way as to protect confidential information. It should not be assumed that email is private, because email messages can easily be accessed by people other than their intended recipients. Privacy Issue with Telecommunication Devices The courts have ruled that email sent or received on computers used by employees is considered to be the property of the company, and therefore, privacy and confidentiality do not exist. Implications of HIPAA for Mental Health Providers The Health Insurance Portability and Accountability Act of 1996 (HIPAA) was passed by Congress to promote standardization and efficiency in the health care industry and to give patients more rights and control over their health information. These regulations protect patients by limiting the ways that covered entities can use patients’ medical information and other individually identifiable health information. Implications of HIPAA for Mental Health Providers cont. Only mental health providers who fall within the definition of covered entity are subject to HIPPA requirements. The Duty to Warn and to Protect According to Mitchell (2000), those in the counseling profession often have to weigh these conflicting principles: The client’s right to privacy versus the therapist’s responsibility to protect society. The client’s right of confidentiality versus the therapist’s obligation to protect the community from violent behavior. The client’s right to die versus the therapist’s obligation to save lives. The Duty to Protect Potential Victims Even though practitioners are not generally legally liable for their failure to render perfect predictions of violent behavior of a client, they can be charged if they are careless or unprofessional. Most states permit (if not require) therapists to breach confidentiality to warn or protect victims. Many states grant therapists protection from being sued for breaching confidentiality if the therapist can show that he or she acted in good faith to protect third parties. The Tarasoff Case The California Supreme Court ruled that a failure to warn an intended victim was professionally irresponsible. The court held that simply notifying the police was insufficient to protect the identifiable victim. Negligence lies in the practitioner’s failure to warn a third party of imminent danger, not in failing to predict any violence that may be committed. The Tarasoff Case continued According to this decision, “the protective privilege ends where the public peril begins.” It is generally assumed that the duty to warn and to protect is a national legal requirement. According to Knapp & VandeCreek (1982), “psychotherapists need only follow reasonable standards in predicting violence.” Therefore, therapists should not become intimidated by every idle fantasy, for every impulsive threat is not evidence of imminent danger. The Tarasoff Case continued Not all states have embraced the Tarasoff doctrine. In 1999, the members of the Texas Supreme court unanimously rejected the Tarasoff duty. Other Court Cases The Bradley case illustrates the duty not to negligently release a dangerous client by ruling that a physician has a duty to take reasonable care to prevent a potentially dangerous patient from inflicting harm. The Jablonski case underscores the duty to commit a dangerous individual and that failure to obtain a dangerous patient’s prior medical history can constitute malpractice. Other Court Cases continued The Jaffee case found that communications between licensed psychotherapists and their clients are privileged and therefore protected from forced disclosure in cases arising under federal law. Jaffee applies only in federal cases. According to DeBell & Jones (1997), Jaffee does not appear to cover couples, family, and group therapy. Implications of Duty to Warn and to Protect for School Counselors Courts have uniformly held that school personnel have a duty to protect students from foreseeable harm. School officials may be held accountable if a student’s writing assignments contain evidence of premeditated violence. According to Hermann (2002), 63% of the school counselors in her study believed they were well prepared to determine whether a student posed a danger to others. Guidelines for Dealing with Dangerous Clients Most counseling centers and community mental health agencies now have guidelines regarding the duty to warn and protect when the welfare of others is at stake. In most cases, therapists will not have advanced warning that a client is dangerous. Under NO circumstances should clinicians alter client records. If asked under oath whether any part of the records have been altered and such entries later come to light, the clinician is guilty of perjury, a criminal offense. The Duty to Protect Suicidal Clients Therapists have a legal duty to protect suicidal clients. According to Remley & Herlihy (2005), counselors can be accused of malpractice for neglecting to take action to prevent harm when a client is likely to commit suicide, yet they are also liable if they overreact by taking actions that violate a client’s privacy when there is not a justifiable basis for doing so. School Counselor Liability for Student Suicide According to Hermann (2002), the most prevalent legal issue encountered by school counselors involves them making a determination whether students are suicidal. Hermann (2002) found that 72% of the school counselors surveyed believed they were well prepared to determine whether a client was suicidal. School Counselor Liability for Student Suicide continued According to King & colleagues (1999), only 38% of the high school counselors surveyed believed they could determine if a student was at risk for committing suicide. Court Cases and School Settings Courts have found a special relationship between school personnel and students. Even if the risk of the student actually committing suicide is remote, the possibility may be enough to establish a duty to contact the parents and to inform them of the potential for suicidal behavior. The courts have addressed the need for training school employees in suicide prevention. Guidelines for Assessing Suicidal Behavior In an assessment interview, focus should be placed on evaluating depression, suicide ideation, suicide intention, and suicide plans. Suicide is the 8th leading cause of death in the United States. It is the 13th leading cause for the elderly. It is the 3rd leading cause for young people between the ages of 15 and 24. Guidelines for Assessing Suicidal Behavior continued Men are 3 times more likely than women to commit suicide. Single people are twice as likely as married people to commit suicide. Factors such as unemployment increase the risk of suicide. Once it is determined that a client is at risk, the professional is legally required to break confidentiality and take appropriate action. Guidelines for Assessing Suicidal Behavior continued According to Sommers-Flanagan & SommersFlanagan (1995), both consultation and documentation offer safeguards against malpractice liability. The final decision about the degree of suicidal risk is a subjective one that demands professional judgment. If a client demonstrates suicidal intent, and the therapist does not exercise reasonable precautions, there are grounds for liability. The Case for Suicide Prevention Suicidal individuals often hope that somebody will listen to their cry for help. There are differing expectations for action by mental health professionals dealing with suicide depending on the setting. Remember that clients are ultimately responsible for their own actions and that there is only so much that you can reasonably do to prevent self-destruction. The Case Against Suicide Prevention Szasz (1986) does not believe that mental health professionals have an absolute professional duty to try to prevent suicide. He believes that by attempting to prevent suicide, professionals often ally themselves with the police power of the state and resort to coercion, therein identifying themselves as foes of individual liberty and responsibility. He believes that it is the client’s responsibility to choose to live or to die. Concluding Thoughts on Suicide According to Benitez (2004), there is no Tarasoff duty to report when a client is threatening suicide. Protecting Children, the Elderly, & Dependent Adults from Harm Privileged communication does not apply in cases of child abuse and neglect, nor does it apply in cases of elder and dependent adult abuse. In 2003, more than 550,000 elderly people were reported abused or neglected in the U.S., but the actual number may be 4 or 5 times higher than this. Mandatory reporting laws differ from state to state. Protecting Children, the Elderly, & Dependent Adults from Harm State laws may not always be effective in inducing professionals to report suspected child abuse as evidenced by the fact that many do not adhere to mandatory reporting laws. Confidentiality & HIV/AIDSRelated Issues People that have tested HIV-positive are often very anxious, are struggling with the stigma attached to AIDS, and they typically have a great deal of anger. Those at risk are often angry at health professionals as well. Ethical & Legal Considerations in AIDS-Related Cases Courts have not applied the duty to warn to cases involving HIV infection, and therapists’ legal responsibility in protecting sexual partners of HIV-positive clients remains unclear. The ACA (2005) ethics code states that counselors “may be justified” in disclosing information to a third party who is at risk, yet counselors are not necessarily “obligated” to take this course of action. Ethical & Legal Considerations in AIDS-Related Cases continued California state law places the practitioner who divulges this confidential information at risk for fines, civil penalties, incarceration, and loss of license. Duty to Protect versus Confidentiality The HIV-positive duty to warn decision is one of the more controversial and emotional issues practitioners might encounter. State laws differ regarding HIV and the limits of confidentiality, and the law is often different for medical professionals than for licensed psychotherapists. Duty to Protect versus Confidentiality continued Two-thirds of the states have enacted legislation specifying limits to confidentiality regarding an individual's HIV status. Very few states (just Montana and Texas) offer legal protection against liability for practitioners who break client confidentiality to warn third parties at risk. Do Tarasoff Principles Apply in AIDS-Related Psychotherapy? McGuire & colleagues (1995) suggest that therapists should be extremely cautious regarding breaching confidentiality and should first consider less intrusive measures. Therapists should be aware that some state laws prohibit warning identifiable third parties of partners who are HIVpositive. Do Tarasoff Principles Apply in AIDS-Related Psychotherapy? Therapists have a duty to protect when the following three conditions are met: There must be a “special client-therapist relationship.” “Clear and imminent danger” must exist. There must be an “identifiable victim.” If an HIV-infected individual is engaging in highrisk behavior with an identifiable, unsuspecting partner, then it appears that the three criteria under the Tarasoff decision may be met. Special Training on HIV-Related Issues According to Werth & Carney (1994), several surveys show that most students are not receiving HIV-related training in their graduate programs and are unprepared to handle ethical, legal, and professional issues pertaining to HIV situations.



![Client Confidentiality[1]](http://s3.studylib.net/store/data/006761054_1-1010f2add5d881dd5546c5d48c372038-300x300.png)