clinical presentation and predictors of outcome in patients
advertisement

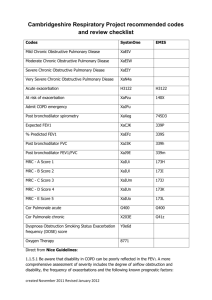
CLINICAL PRESENTATION AND PREDICTORS OF OUTCOME IN PATIENTS WITH SEVERE ACUTE EXACERBATION OF COPD REQUIRING ADMISSION TO ICU By Mohan et al BACKGROUND • COPD is a common, costly preventable disease and is the 4th leading cause of death globally • Acute exacerbation of COPD(AE-COPD) is a common cause of ER visit • Major cause of morbidity and mortality with more than half of these patients requiring re-admission in subsequent 6 months • Great variability in clinical course making predictions of outcome in a given patient difficult • The study was designed to prospectively study the clinical presentation and predictors of outcome in patients with AE-COPD requiring admission to ICU METHODS • During period from June 2000 and December 2004 , 914 patients diagnosed with COPD in MOPD and Chest Clinic at a Tertiary Hospital • 314 of these later on presented to ER with AE-COPD • After appropriate initial treatment, 116 admitted to Medical ICU, 18 discharged, 180 admitted to Acute Medical Unit and Medical Ward • Basis of study is on the 116 admitted to ICU • Patients with bronchiectasis, interstitial lung disease,PE, Pulmonary Oedema excluded • Study was approved by Ethical Committee • COPD diagnosed on basis of Pulmonary Function tests during MOPD visits • AE-COPD diagnosed if all following present: rapid worsening dyspnoea, increase in sputum volume and purulence • Only single enrolement per patient regardless of frequency of exacerbations • On arrival full Hx including type of smoking habit cigarette or bidi and pack years, domestic fuel use and examination • Baseline investigations including imaging • O2 given as appropriate nasal prongs, face mask or Ventura devices • Nebs of Salbutamol/Ipratropium every 15 min to 8 hourly , steroids if no improvement iv aminophylline. Empiric antibiotics given could be changed on sensitivities • No standard criterion for Invasive Ventilation • In study indications include, failure to respond to pharmacologic and other non-ventilatory Rx, severe dyspnoea, severe acidosis (pH < 7,25) , hypercapnea (P CO2 > 60mmHg), life threating hypoxaemia, respiratory arrest, somnolence, impaired mental status and co-morbid illness STATISTICAL ANALYSIS • Variables following normal distribution were summarised by mean and standard deviation • Association between two categorical variables was by χ2 or Fisher’s exact test as appropriate • Student t test used for quantitative variables • Quantitative variables categorised and if it showed statistically significant association with outcome at p < 0.20 considered for inclusion • Stepwise multivariate logistic regression performed with potential candidate variables as co-variates • SYSTAT Version 7.0 used. All stat tests performed were two tailed, p <0.05 considered statistically significant RESULTS . Mean age 62.1 ± 9.8 years with 102(88%) males .Mean duration of COPD 7.2 ± 5.8 years .All males were smokers for 22.3 ± 11.2 pack years 35.2% smoked cigarettes and 64.8 % smoked bidis. All women non-smokers and were exposed to domestic fuels .81 (69.8%) patients had co-morbid illness with 53 (45.7%) having one condition and 28(54.3%) having 2 or more .Past PTB in 33(28.4%) patients, 5 patients with Type 2 DM found to have active PTB .ABG showed Respiratory Failure in 40(33.8 %) patients Type 1 in 17.5% and Type 2 in 82.5% .Invasive Ventilation required in 18 patients .16 (13.7%) patients died in the study Predictors of death: need for invasive ventilation, presence of co-morbid illness and hypercapnoea Table 1 Demographic characteristics and co-morbid conditions in 116 patients with acute exacerbation of chronic obstructive pulmonary disease admitted to the medical intensive care unit Age (years) (mean ± SD) Gender Male Female Smoking (all males) Duration of symptoms (years) (mean ± SD) COPD, GOLD stage* Moderate [No. (%)] Severe [No. (%)] Very severe [No. (%)] Co-morbid conditions Hypertension [No. (%)] Alcoholism [No. (%)] Type II diabetes mellitus [No. (%)] Past pulmonary tuberculosis [No. (%)] Coronary artery disease [No. (%)] Chronic renal failure [No. (%)] Number of co-morbid illnesses 0 [No. (%)] 1 [No. (%)] 2 [No. (%)] 3 [No. (%)] 4 [No. (%)] • • • • • • • 62.1 ± 9.8 102 14 22.3 ± 11.2 pack years 7.6 ± 5.2 25 (21.6) 55 (47.4) 36 (31.0) 40 (34.5) 38 (32.8) 36 (31.0) † 33 (28.4) ‡ 12 (10.3) 10 (08.6) 35 (30.2) 53 (45.7) 18 (15.5) 07 (06.0) 03 (02.6) GOLD = Global Initiative for Chronic Obstructive Lung Disease (reference 1) COPD = chronic obstructive pulmonary disease * In all patients post-bronchodilator forced expiratory volume in one second (FEV1)/forced vital capacity (FVC) was ≤ 0.7. Moderately severe COPD, FEV1 = 50 – 80% predicted; severe COPD, FEV1 = 30 – 50% predicted; very severe COPD = <30% predicted (reference 1) † 3 patients had diabetic ketoacidosis and 5 patients had active pulmonary tuberculosis ‡ Clinical and radiographic evidence of past tuberculosis was present More than one co-morbid conditions were present in several patients Mohan et al. BMC Pulmonary Medicine 2006 6:27 doi:10.1186/1471-2466-6-27 Table 2 Clinical presentation in 116 patients with acute exacerbation of chronic obstructive pulmonary disease admitted to the medical intensive care unit Variable Symptoms Cough Increased sputum volume Increased sputum purulence Recent rapid worsening of dyspnea Accessory muscle use Inability to complete a full sentence while talking Pedal edema Fever Altered sensorium Upper respiratory infection Gastroesophageal reflux Signs Wheezing Respiratory rate > 24/min Crepitations Cyanosis Heart rate > 100/min Elevated JVP Systolic BP < 90 mm Hg • • % 100 100 100 100 60.3 60.3 19.8 29.3 12.9 8.6 7.8 100 94 56 33.6 25 12.9 3.4 JVP = jugular venous pulse Mohan et al. BMC Pulmonary Medicine 2006 6:27 doi:10.1186/1471-2466-6-27 Table 3 Laboratory abnormalities in 116 patients with acute exacerbation of chronic obstructive pulmonary disease admitted to the medical intensive care unit Variable % Polycythemia (PCV >54% in men, >49% in women) 32.8 Leukocytosis [(>12 × 103/mm3), (>12 × 109/l)] 64.7 Neutrophilia [(> 70%), (> 0.7)] 77.6 Elevated ESR (>20 mm at the end of the first hour) 64.7 Hypoalbuminemia [(< 3.5 g/dl), (< 35 g/dl)] 19.0 Hyponatremia [serum sodium < 120 meq/l, (< 120 mmol/l)] 16.4 Hypokalemia [serum potassium < 3.5 meq/l, (< 3.5 mmol/l)] 16.4 Hyperbilirubinemia [(>1.2 mg/dl), (> 20.5 μmol/l)] 6.0 Elevated transaminases [>50 IU/l] 22.4 Elevated blood urea [(>50 mg/dl), (>17.9 mmol/l)] 45.7 Elevated serum creatinine [(>1.5 mg/dl), (> 132.6 μmol/l)] 19.0 • ESR = erythrocyte sedimentation rate • Mohan et al. BMC Pulmonary Medicine 2006 6:27 doi:10.1186/1471-2466-6-27 Table 4 Predictors of outcome in 116 patients with severe acute exacerbation of chronic obstructive pulmonary disease requiring admission to the intensive care unit: univariate sensitivity analysis Variable • χ2 p-value Presence of co-morbid illness 1.673 0.0196 Altered consciousness 3.650 0.0560 Presence of tachycardia 9.605 0.0020 Peripheral edema 1.900 0.1680 Hypoalbuminemia 4.300 0.0380 Elevated transaminases 4.200 0.0350 Acidosis 10.257 0.0010 Arterial hypoxemia 4.999 0.0250 Hypercapnia 2.189 0.1390 Presence of new infiltrates on the chest radiograph 5.240 0.0170 Need for invasive ventilation 16.178 0.0001 Mohan et al. BMC Pulmonary Medicine 2006 6:27 doi:10.1186/1471-2466-6-27 Table 5 Predictors of death in 116 patients with severe acute exacerbation of chronic obstructive pulmonary disease requiring admission to the intensive care unit: stepwise multivariate logistic regression analysis Variable • Odds ratio 95% Confidence intervals p-value Need for invasive ventilation 45.809 607.46 to 3.009 p < 0.001 Presence of co-morbid illness 0.126 0.428 to 0.037 p < 0.01 Hypercapnia 0.114 1.324 to 0.010 p < 0.05 Mohan et al. BMC Pulmonary Medicine 2006 6:27 doi:10.1186/1471-2466-6-27 DISCUSSION • Not much info on burden of AE-COPD in ER, its presentation and outcome • Significant number of patients (n=53; 45.7%) had co-morbid conditions, and this was a predictor of death • Accurate assessment of co-morbid conditions and institution of specific treatments should help to reduce morbidity and mortality • Past PTB important cause of COPD and also of AE-COPD (p<0.001) • Ramifications in areas where PTB endemic and smoking on the rise • High prevalence of respiratory failure in study . Invasive ventilation associated with poor prognosis • In conclusion, in addition to host genetic factors, smoking behaviour, accessibility to health care and presence of co-morbid conditions contribute to morbidity and mortality due to AE-COPD