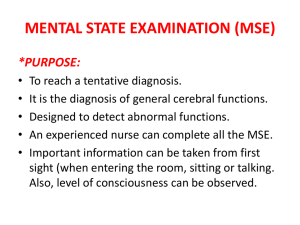
Mental state examination (MSE)
advertisement

Mental state examination (MSE) Prepared by: * Mr. Bassim Bakeer Supervised by: * Dr. Abed Alkareem Radwan. Purpose: the purpose of mental state examination is to reach a tentative diagnosis. It is the diagnosis of general cerebral functions. It is designed to detect abnormal functions. An experienced nurse can complete all the MSE. Important information about the patient can be taken from first sight as the patient seen entering the room, sitting or talking. The first observation is made to the level of consciousness. General appearance: is a good indicator of the patients over all mental build. functioning. It includes the weight, height and general body Nutritional status: poor nutrition can result from medical or psychiatric disorders. In anorexia nervosa the patient is emaciated but still thinks she is fat. Overweight can point to over eating as in affective disorders with hyperphagia. Hygiene and dress: self care and cleanliness reflects the patients awareness and activity level. In depression the patient loses interest on his appearance and hygiene. In mania the patient dresses in colorful and flamboyant manner. She may use too much makeup and mismatched dress. Schizophrenics may use strange items for dress e.g. antennas, bags to protect them from the control of space people. Eye contact: people usually maintain eye contact when they speak, and track the movement and gestures of the interviewer. Abnormal eye movement can be diagnostic. Wandering eyes show distractibility, visual hallucinations, mania or organic states. Avoidance of eye contact may be due to hostility, shyness, or anxiety. If the patient is suspicious he tracks your movements and look to every gesture. Psychomotor behavior: Psychomotor activity can be reduced in depression and catatonic schizophrenia or increase in mania. Posture: the way the patient sits, walks and behaves. Facial expression: the facial expression of the patient e.g. sad face in depression. Activity level: the level of activity of the patient. Restlessness in anxiety, agitation in some depressed patients, excitement in mania. Abnormal movements: can be voluntary or involuntary, voluntary abnormal movements such as the mannerisms of the schizophrenia or bizarre movements also seen in schizophrenia. Involuntary movements such as hand tremor in Mood and affect: Mood: is defined as the pervasive and sustained emotion that colors the persons perception of the world. In depression the patient is depressed he sees the world through dark glasses. On the other hand in mania he is euphoric or elated he feels superior and able to do great things. In anxiety the patient is tense and expecting the worst. Affect: it is the external expression of the patients emotional responsiveness. It is what the examiner observes in the patients facial expression and expressive behavior in response to internal or external stimuli. Affect is evaluated for its intensity, duration, appropriateness to the situation, range of affective expression and control. In schizophrenia the affect is blunted (flat) or restricted, it may be inappropriate to the situation. In mania it is expansive and out of control. Hysterical patients show labile affect that changes from extreme happiness to extreme sadness in minutes. Speech: Amount of speech: increased in mania and anxiety states were the patient is talkative, a manic may experience a pressure to speak continuously, a depressed patient speaks very little and brief. Speed: anxious patient speaks rapidly, depressed one speaks slowly. Articulation: speech can be slurred (dysarthria) as in organic brain disorders or intoxication with alcohol or hypnotic. Rhythm: in depression speech is monotonous. Thought: Thought is divided into process and content. Thought process: Process is the way patient puts thoughts together and associates between them. Thought process may be rapid and the patient feels pressure of thoughts, this may go on to form flight of ideas as in mania, or it may be slow as in depression. In schizophrenia there is loss of association between thoughts or poverty of thoughts were they could be empty or vague. Blocking is the interruption of thought process as if they were withdrawn from the patients head as in schizophrenia. Thought content: The interviewer should evaluate the content of thoughts for abnormalities. Delusions: these are false fixed beliefs held by the patient and not shared by persons in his culture. They indicate that the patient is psychotic e.g. delusions of persecution, reference or grandiosity. Overvalued ideas: unreasonable sustained false beliefs held less firmly than delusions. Phobias: unreasonable fear of exposure to specific objects or situations e.g. agoraphobia, claustrophobia. Obsessions: irresistible recurrent thought or feeling that cannot be eliminated by logical effort and associated with anxiety. Compulsions: meaningless acts that the patient feels compelled to perform. Counting, washing…… Hypochondria: exaggerated concern over ones health based on false interpretation of physical signs and not supported by realistic pathology. Perception: interpretation of events. Some types of hallucination appears in some clients according to the senses. We have to be sure that patient has no organic problems especially in the condition of visual hallucination. They are divided into five types: 1- visual 2- auditory 3- olfactory 4- tactile 5- taste Sensorium and cognition: Level of consciousness: the patient awareness of and responsiveness to his internal and external environments. It can be clouded in organic states and intoxication. Orientation: patients awareness of his time, place and person. This usually disturbed in organic brain syndromes. Concentration: the ability to keep ones attention on a certain task. See if the patient can subtract 7 from 100 and notice his effort and time taken to perform this task. Concentration is impaired in mania were the patient is distractible by minor stimuli and in anxiety states. Memory: the ability to recall information. It is divided into: Immediate retention: ask the patient to repeat 6 digits in the same order (within seconds to less than a minute) Short term memory: tell the patient three items and ask him to repeat them after 5 to 10 minutes. Long term memory: ask the patient what he did yesterday. Remote memory: ask the patient about information in his childhood, school….. Abstract thinking: this is the ability to deal with concepts. Ask the patient to explain a known proverb or the similarity between two things. Answers may be concrete as if the patient says that an orange and an apple are both round. Or abstract if he says that they are both fruit. Abstract thinking is impaired in schizophrenia and organic brain syndrome. Intelligence and information: if impairment is suspected, you can ask the patient to perform simple tasks as calculations, for example ask him what remains of a 100$ if he buys a shirt with 35$ and a pants with 64$. If he finds difficult ask easier questions. The patients fund of information should be relevant to his educational and social background. Ask about important dates persons, or….. Insight and judgment: Insight: is the degree of the patients awareness that he is ill. The patient may deny completely that he has any problem, here insight is totally lost. Some patients realize that there is a problem but explain it to be a result of somatic or social cause. This is partial insight. Judgment: is the ability to choose appropriate goals and appropriate means to reach them. Ask the patient what he would do if he smelled smoke in his house or found a closed addressed letter in the street. Impulse control: Is the patient ability to control his sexual, aggressive and other impulses. Some patients cannot resist impulses to explore your office they look in books and turn things e.g. mania. Impulse control can be assessed from the patients history. Reliability: How reliable is the information gathered about the patient. Did he report his condition accurately or was there any difficulty due to mental retardation, dementia or impaired consciousness. Is there a need for further investigations. Summary: Major positive and negative data from the history and MSE are summarized. A provisional diagnosis is suggested and a differential diagnosis is given. Investigations and tests The End: Thank you