CVS Spiral II Study Guide - Shifa College of Medicine
advertisement

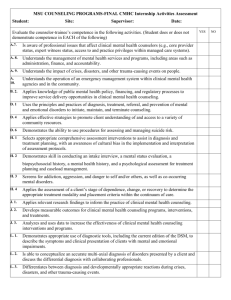
1 SHIFA COLLEGE OF MEDICINE STUDY GUIDE CARDIO-VASCULAR SYSTEM Y-3 (Spiral II) 2 CONTENTS Introduction ICON’s index Themes of the module TOS 1. ACUTELY PAINFUL DISCOLOURED LIMB 20 % 2. CHEST PAIN 25% 3. HYPERTENSION (SILENT KILLER) 15% 4. BREATHLESSNESS WITH SWELLING 10 % 5. PALPITATIONS 15% 6. YOUNG FEMALE WITH FEVER AND PALPITATIONS 05% 7. SUDDEN DEATH Resource Material Team members & People to contact Glossary 10% 3 INTRODUCTION What this module is all about. Welcome to CVS (Cardio vascular system), a module you would most like, is a blend of basic and clinical sciences. The CVS is an important system as in this modern world of science; the cardiovascular diseases are the most common cause of death in the developed and the developing countries. CVS related diseases are more common throughout the world, these diseases are responsible for huge burden on economy and utilize a greater part of health resources. You have already gone through the basic structure and function of CVS in Spiral I and now this module will be more focused on pathogenesis of CVS related diseases along with their clinical significance. General Overview In the CVS module you will find the true spirit of integration. The 3rd year (CVS Y-3) module will be of 5 weeks. It will include 7 themes of diseases which are clinically and epidemiologically important. It will comprise themes for third year and on these themes cases have been developed to create clinical relevance to whatever is being discussed in the later sessions. You have already been exposed to the integrated system in spiral 1.The format of this module would inshallah surely help you enforce and engrip your hold on both the clinical and basic concepts. Introduction To Exit Competencies You are already aware of various exit competencies which we expect from a doctor, but this module in particular will focus more on Pathogenesis, 4 Clinical expertise, Health advocasy, Communication, Collaboration, Management and professionalism. Linkages With Other Modules CVS Module is strongly inter-related with Respiratory and Urinary System and they are strongly interdependent for maintenance of normal Homeostasis. You have already encountered CVS Module in Spiral I in which emphasis was on normal structure and functions. Now your encounter in spiral II would be with pathogenesis and therapeutic management. General Overview Of Learning Strategies Your time table will guide you through the module and will also tell you about the learning strategy being used during that very session, comprising of SGD (small group discussion), LGIS (large group interactive sessions) and SCIL lab sessions. You will also come across session on journal club to give you an insight into EBM (evidence based medicine). In the guide you will also come across useful tips to help you during the various sessions, your learning resources and people to contact for your problems. Assessment Formative assessment will be carried out during module and summative assessment will be held at the end of Module which will include MCQ’s, SAQ’s and IPE’s. 5 CVS MODULE Duration : 5 weeks (August 26 to 27 September) Team Leader: Dr. Ghazala Mudassir, Dr Tahir Iqbal Team members: 1. Dr. Talat Ahmed 2. Dr. Riffat Nadeem 3. Dr.Samina Ghayur 4. Dr. Mahwish Majid Bhatti 5. Dr AbidaShaheen 6. Dr Fahad Azam 7. Dr Zubaida Zain 8. Dr Tehzeeb Zehra 9. Dr. Gemza Shah 10.Dr. Arooj Anthony 11.Dr. Imran Khan Jehangir 12.Dr. Syeda Hanna Fatima 13.Dr. Muhammad Umer Farooq 14.Dr. Syeda Sitwat Mehmud 15.Dr. Zubia Arshad 16.Dr. Ali Azeem 17.Dr. Sara Rathore 6 You will find symbols throughout the module which indicate some action on your part as follows: Introduction to case Learning objectives SCIL sessions Critical questions Key words Resource material Web address link 7 THEME 1: SWOLLEN LIMB (Thrombosis) CASE 1 Mrs. Ahmed a 40-year-old woman presents with a 10-hour history of gradually increasing pain and swelling in her left calf. There is no history of trauma to the leg. She started taking oral contraceptive pills (OCP) 1 week ago. Her left calf is erythematous, warm and tender to palpation, and is 4 cm thicker than the right calf. Vital signs are normal. Pulses are 2+, and there is 2+ lower extremity pitting edema. 8 CRITICAL QUESTIONS What is the most concerning possibility at this time? What are the risk factors for DVT? What complications can occur? How you will manage a patient with DVT? Knowledge 1. Enumerate relevant investigations e.g. EKG, Echo, BNP 2. Describe the dosage, pharmacokinetics, mechanism of action, adverse effects, drug interactions & contraindications of the drugs used in the 9 management of DVT. Learning Objectives 1) Describe the pathophysiologic causes of edema 2) Describe hyperemia, congestion and hemorrhage. Describe normal hemostasis. 3) Describe normal hemostasis, pathogenesis of thrombosis and its complications. The students should know the medicolegal significance of ante and post mortem clot. 4) Describe the pathogenesis and morphological appearance of infarction. 5) Describe the role of anti-coagulant drugs. SKILL The student should identify; 1) The histopathological slides of thrombosis, edema 2) Order appropriate tests to document DVT 3) Select appropriate plan for DVT treatment 4) Counsel patient on DVT & its complications 10 ATTITUDE 1) Identify risk factors and Risk factors reduction strategies. 2) Health promotion of disease prevention 3) Demonstrate general professional attitude when dealing with patients 4) Counseling for prevention and its complication Theme 2: CHEST PAIN CASE 1 Mrs. Ahmed now presents with an 8 weeks history of substernal chest tightness and pressure that radiates to the left arm. The discomfort occurs predictably after 5 minutes of exercise and causes her to stop all activity. Her symptoms gradually increase in intensity and resolve within 3-4 minutes of rest. Breathing and position don’t change her symptoms .She doesn’t have any dyspnea, diaphoresis, nausea or vomiting. She has a history of hypertension that is controlled with hydrochlorothiazide. Her father has diabetes and both parents have hypertension. She has smoked a pack of cigarettes a day since she was 25 years old. Physical examination, vital signs and resting EKG are normal. 11 Anterior Ischemia (Angina) CRITICAL QUESTIONS What is the most likely cause of her symptoms ? How is stable angina managed ? Why is an exercise stress test recommended in patient with stable angina? How is revascularization of the coronary arteries achieved ? Should this patient undergo percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) ? 12 Case 2 Mrs. Ahmed presented in medical emergency with c/o severe crushing chest pain, tachycardia and edema for the last 1 hour. She has a h/o stable angina on exertion that is usually relieved by sub-lingual nitroglycerine. Her current symptoms occurred at rest and have not responded to nitroglycerine at home. She has h/o hypertension and smoking. She is sweating and appears anxious. On examination: Pulse 110/min, BP 140/85 mmHg, R/R 22/min, oxygen saturation 98% on room air,Temperature37.6C.CVS=S1+S2+0,Chest=Clear. 13 Acute Anterior wall MI Coronary angiography. Showing triple vessel disease . 14 Learning Objectives The student should be able to : Enumerate various causes of cell injury. Describe the various series of events resulting in cell injury eg following ischemic insult, Mitochondrial damage, intracellular Ca influx, ROS & Defects in membrane permeability. Differentiate between Reversible & Irreversible cell injury on basis of histological features. Define necrosis & describe its mechanisms . Differentiate & describe the gross & microscopic features of various types of necrosis. To recognize the histological features & diagnose apoptosis (like cell shrinkage,chromatin condensation , apoptotic bodies etc) To be able to describe Mechanisms of development of apoptosis (The Extrinsic,Intrinsic pathway,Execution phase & removal of dead cells). To describe various subcellular responses to injury eg.lysosomal catabolism,smooth muscle hypertrophy etc by microscopic analysis. To enumerate the various intracellular accumulations with their salient histological features , their correlation with various diseases To identify the causes, morphology & pathogenesis of pathologic calcification. Describe the causes, pathogenesis & complications of myocardial infarction with clinical correlation of continuum of IHD (stable angina, unstable angina, CHF, Arrhythmias) Describe the dosage, contraindication, mechanism of action and cautions of the drugs used in Angina and Myocardial Infarction; (Fibrinolytics, Drugs used to decrease ischemia, Drugs used as adjunct treatment) Formulate an evidence based plan for ACS. Discuss the causes, pathogenesis & complications of hypercholesterolemia. 15 Increased cholesterol levels with various endothelial changes. Relate Atherosclerosis with organ dysfunction (myocardium). Discuss Atherosclerosis & Differentiate between the concepts of fixed vessel narrowing and Plaque rupture. SKILLS The student should be able to: Identify histopathological slides of coagulation necrosis, caseation necrosis To identify histopathological slides of intracellular events like fatty change, hemosiderosis, cholestasis, melanin pigmentation, anthracosis and dystrophic calcification. Take history of chest pain (intensity, site, radiation, associated symptoms) Perform general physical examination & detailed CVS examination Differentiate between various components of pulse (rate, rhythm, volume, character) (revisit) Identify the heart sounds (normal, abnormal) (S1, 2, 3, & 4) and added sounds Formulate differential diagnosis of chest pain Choose appropriate labs: laboratory tests for ACS e.g. cardiac enzymes (CK-MB, Troponins, and LDH) and understanding their time of rise and diagnostic preference Identify and differentiate gross and microscopic morphological features of live and dead tissue and to determine the cause of death in that tissue EKG: basis of cardiac electric activity, ST depression and elevation (revisit) 16 CXR &Echocardiogram ATTITUDE Counseling on risk factors (DM, HTN, dyslipidemia, smoking, sedentary life style etc) and risk factors reduction strategies. Demonstrate professional attitude when dealing with patients Counseling for primary & secondary prevention of heart disease Nutritional counseling CRITICAL QUESTIONS What is the most likely diagnosis? How will you investigate this patient ? What are the initial steps in the management of this patient? Which thrombolytic agent should this patient receive? What revascularization method should this patient undergo? What tests are recommended prior to discharge for risk satisfaction? What medications should this patient receive? What additional therapy would you recommended if the patient had evidence of systolic heart failure with an ejection fraction of 30 percent on Echocardiography? 17 Case 3 The condition of Mrs. Ahmed deteriorated. Fifteen hours later, blood pressure is 90/60, pulse is 120 bpm, respirations are 25/minute, and oxygen saturation is 94%. Skin is cool and clammy, and 14 cm of JVD is present. New crackles are appreciated in both lung bases. Urine output is 0.2 mg/kg per hour. LEARNING OBJECTIVES 1. Discuss the causes, types, pathogenesis & clinical features of cardiogenic shock and differentiate it from other types of shock. 2. Explain the treatment of various types of shock. Critical Question 1: What is the likely cause of shock? 18 2: What are the next steps in management? 4: What is a Swan-Ganz catheter? What are the Swan-Ganz findings in different types of shock 5: PCWP is 21 mm Hg (normal 6 to 12). Hypotension, elevated PCWP, and other signs of shock persist despite vasopressors. Is there any treatment for patients with refractory cardiogenic shock? THEME 3: HYPERTENSION CASE A 50 years old man presents to the clinic for an annual check-up. He does not have any prior medical history, hospitalization or surgery. He smokes half a pack of cigarettes a day and drinks a glass of wine every night. Physical examinations are unremarkable. Temperature, pulse and respiration are within normal limits .Blood pressure is 135/80., cvs=S1+S2+0.The patient asks if his BP is normal. 19 Typical ECG in Hypertension showing LVH with lateral strain pattern LEARNING OBJECTIVES KNOWLEDGE Draw a concept map for pathways /mechanism leading to hypertension. Classify and select anti hypertensive drugs and discuss the dosage, pharmacokinetics, mechanism of action, adverse effects and drug interaction of various anti hypertensive’s 20 SKILL Take focused history of a hypertensive patient Record blood pressure in different positions Perform necessary bed side clinical evaluation and order pertinent laboratory tests ATTITUDE Identify risk factors and risk factors reduction strategies. Demonstrate professional attitude when dealing with patients Counseling for primary & secondary prevention of HTN and its complications Nutritional and life style counseling. CRITICAL QUESTIONS What non-pharmacological measures you will advise to this patient? During his follow up appointment 1 year later, his BP readings are above 145/90 mmHg. What anti-hypertensive you will start. What end-organ damage caused by hypertension? 21 How does malignant hypertension differs from accelerated hypertension and hypertensive encephalopathy ? How does hypertensive emergency managed? THEME 4: BREATHLESSNESS AND SWELLING (CCF) A 58 years old man with 10 year h/o hypertension presents with dyspnea and dry cough that has been progressively worsening over the last 6 months. Initially he experienced dyspnea only after a brisk 1 km walk. He now has dyspnea climbing up a few flight of stairs. On lying down, his symptom worsen and he often needs three to four pillows to fall asleep (orthopnea). Auscultation of the heart reveals a S3, S4 and a 1/6 blowing holosystolic murmur heard best at the apex that radiates to the axilla. Apex beat is displaced to the left. There are bilateral basal crackles. JVP is raised (9cm).The liver edge is tender and is 4cm below coatal margin (tender hepatomegaly). He has a marked peripheral edema. BP is 170/100 mmHg and pulse is 80/min, regular. 22 Learning Objectives 1.Enumerate relevant investigations eg. EKG, Echo, BNP. 2. Describe the dosage, pharmacokinetics, mechanism of action, adverse effects, drug interactions and contraindications of drugs used in heart failure. SKILL Take history and physical examination of patient with heart failure. ATTITUDE 1.Address risk factors and risk factor reduction strategies. 2.Demonstrate professional attitude when dealing with patients 3.Counseling for primary & secondary prevention of HTN and its complications 4.Nutritional and life style counseling. CRITICAL QUESTIONS 1. What is the most likely diagnosis? 2. What are the most important causes of congestive cardiac failure? 3. What investigations would you advise this patient? 4. How will you treat a patient with CCF? 5. What are the symptoms of Digoxin toxicity and how will you manage it? 6. What do you mean by pulmonary edema and how will you manage it? 23 THEME 5: PALPITATIONS CASE 1 : A 76 years old man presents with a 1 week history of intermittent palpitations. He is currently asymptomatic. He has a H/O hypertension that is treated with hydrochlorthiazide and lisinopril. He is alert and oriented .Heart rate is 120/min and pulse is irregular .He is afebrile .Bp is 130/80 mmHg .ECG revealed irregularly irregular rhythm with no identification P waves and wavy base line. Atrial Fibrillation with fast ventricular rate 24 Atrial Fibrillation with slow ventricular rate CRITICAL QUESTIONS What is the most likely diagnosis ? What are the causes of atrial fibrillation ? How you will manage a patient with atrial fibrillation ? Why is cardioversion not recommended initially in stable patient with atrial fibrillation? How would initial management have differed if the patient presented with palpitations and tachycardia and his Bp was 80/60 mmHg ? 25 What is synchronized cardioversion ? How does it differ from defibrillation ? CASE 2 : A 30 years old man presents with palpitation and light headedness .ECG revealed tachycardia with regular rhythm and narrow QRS complex SVT CRITICAL QUESTIONS What is the most likely diagnosis? What is the mechanism of SVT ? What are the pharmacological and non-pharmacological measures of treatment ? 26 CASE 3: A70 years old man, with a history of systolic heart failure .ECG revealed that there is no PR interval lengthening and a number of normal impulses are conducted. Suddenly , the P wave fails to conduct and there is no QRS complex. IIo Heart block (Mobitz type 2) with 2:1 conduction with Io Heart block (prolonged PR) 27 CRITICAL QUESTIONS What is the diagnosis ? What is the underlying mechanism ? What further complication can occur ? How will you manage this patient ? LEARNINGT OBJECTIVES KNOWLEDGE Explain the mechanism and etiology of brady and tachyarrhythmia Describe indication of anti-arrhythmic drugs, their mechanism of action, pharmacokinetics, adverse effects, interactions & contraindications Identify Indications for CPR (DC shock, TPM and PPM) in a patient of arrhythmias Attend the course of BLS and ACLS 28 SKILL Interpret arrythmias on ECG (Identify Arrhythmias as Brady or tachyarrhythmia) Perform BLS and CPR ATTITUDE Identify risk factors and risk factors reduction strategies. Demonstrate health promotion of disease prevention Demonstrate general professional attitude when dealing with patients Counseling for its complications Nutritional and life style counseling THEME 6: YOUNG FEMALE WITH FEVER AND PALPITATION CASE 1 : A 15 years old female presented to the medical clinic with a three weeks H/O joint pain.It initially started in her knees followed by her wrists.She recalls having a sore-throat two weeks before her symptoms began .Physical 29 examination is significant for three firm,symmetric and painless subcutaneous nodules over the olecranon processess.There are erythematous non-pruritic plaques with a pale center on the trunk .Auscultation of the heart reveals 2/6 systolic murmur, that is heard best at the apex and radiates to the axilla.Vital signs are temperatur.38.9 C,pulse=90/m, R/R =12/m ,BP=110/70mmHg and oxygen saturation 95 percent. 30 CRITICAL QUESTIONS What is the most likely diagnosis ? What are minor and major criteria ? How is acute rheumatic fever treated ? CASE 2 : A 30 years old male presented to the medical clinic with a three weeks history of low-grade fever, malaise and arthralgia .He has a history of intravenous drug abuse .He has no other prior medical history .Physical examination is significant for 1/6 blowing murmur heard best at the left lower sternal border that increases with inspiration and decreases with expiration.There are numerous recent injection marks on his right and left arms, Vital signs are temperature.39 C,Pulse :90/m, respirations (R/R):15/min, BP=110/75 mmHg. CRITICAL QUESTIONS What is the diagnosis? What are the important physical findings of infective 31 Endocarditis? What investigations you will advise? What causative organisms are most likely in this patient ? What is major and minor criteria for diagnosis of infective endocarditis? LEARNING OBJECTIVES KNOWLEDGE Describe diagnostic criteria, etiologic organisms, sequelae, prophylaxis, complications of Infective endocarditis. Outline the principles of management of a patient of Infective endocarditis. SKILL Surface marking of cardiac valves on SP (simulated patient) (revisit) Take history and perform physical examination of a patient with valvular heart disease. Identify systole and diastole murmurs on mannequin. 32 ATTITUDE Counseling risk factors and Risk factors reduction strategies. Discuss health promotion of disease prevention Demonstrate general professional attitude when dealing with patients Counseling for its complications Life style counseling THEME 7: SUDDEN DEATH CASE This is an unusual case of homicide where a young woman was found dead in her bath, slumped forwards in a kneeling position with one breast resting against a chrome tap. The left arm was trailing over the edge of the bath, in which was the usual level of water plus an electric fan heater immersed near the feet. To all intents and purposes it appeared that the woman, while taking her bath had accidentally slipped in the bath and drowned. This is not a very unusual mode of death. Several people have accidentally died in this way. 33 As regards the heater in the water, it was assumed that when the woman must be struggling to find her way out, her legs may have got entangled in the cable wire somehow and she must have accidentally dragged the heater in the bath. AUTOPSY FINDINGS: However while conducting the post mortem examination; the autopsy surgeon noted two curious marks on the body. The first was on the left breast and the other was over the inside of her left arm near the axilla. These were the marks produced by electricity. This indicated that this could be a case of homicide. Subsequent investigations revealed that it was indeed a case of homicide and the husband was involved in that ghastly murder. So just two insignificant looking marks took the perpetrator of crime to the gallows. After the suggestion of the autopsy surgeon, the police called the expert electricians and asked them to examine the concerned heater. Surprisingly it was found that the third `earth' wire was disconnected from the earth pin inside the plug. This clearly established the intentions of the murderer who incidentally turned out to be the woman's husband himself. Since the enamel lining of the bath can not allow the current to pass through, the earthing of the current could only occur through the bath water via the chrome waste pipe. The woman was subsequently pushed against the tap by her husband in such a way that her left breast touched the metal tap. This started another path for the current to pass out-through the body and then through the metal tap. This path presumably took the woman's life. 34 OBJECTIVES At the end of the session, the students should be able to Knowledge: • Enlist the criteria of Certification of Death according to WHO standards. • Differentiate between somatic and molecular death • Enlist sudden natural and unnatural causes of death • Differentiate between mode, manner, mechanism and cause of death. • Determine time since death in different environmental and pathological conditions • Describe the factors affecting time since death • Relate the immediate, early and late changes after death to the mode , manner, mechanism and time since death • Identify post mortem chemical and path physiological changes after death and the factors influencing such changes • Identify the poisons that can lead to a cardiac event. Skills: • Complete/ fill death certificate on the basis of standards laid down by WHO Attitude 35 • Recognize the ethical issues regarding death • Develop sensitivity towards death, the dying patients and the bereaved family CRITICAL QUESTIONS What is the basic criteria of certifying death What are the factors affecting time since death What are the differences between the mode, manner and mechanism of death How would you calculate the time since death after reviewing the changes after death Recommended Reference Books: Medicine: Kumar and Clark clinical medicine 7th edition Davidson’s principles and practice of Medicine Current medical diagnosis and treatment 2011 Pathology: Robbins Pathologic Basis of Disease Microbiology: Jawets, Melnick & Adelberg’s Medical Microbiology 36 Pharmacology: • Basic & Clinical Pharmacology Bertram G. Katzung 11th edition • Lippincott’s Pharmacology latest edition • Essentials of medical pharmacology, JayPee, Tripathy, 6th edition. Forensic: Parikh’s Textbook of medical Jurisprudence.