OS 213 Lec 1: Dementia and Other Neurological Disorders OS 211
advertisement

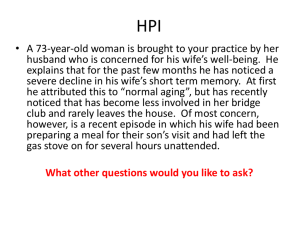
OS 211 [A]: Integration, Coordination, and Behavior Lec 01: Dementia and Other Neurological Disorders Michelle Anlacan, MD, FPNA TOPIC OUTLINE I. II. III. IV. V. VI. Cortical Dementia A. Alzheimer’s Dementia B. Frontotemporal Dementia C. Lewy Body Dementia Subcortical Dementia A. Parkinson’s Disease Dementia B. Huntington’s Disease C. Progressive Supranuclear Palsy D. Normal Pressure Hydrocephalus E. White Matter Disease F. Multiple System Atrophy G. Other Subcortical Dementias H. Distinguishing Cortical from Subcortical Dementias Toxic Metabolic Dementias A. Systemic Illness B. Metabolic and Toxic Causes Reversible Dementias Rapidly Progressing Dementias A. Non Prion Diseases B. Prion Diseases Approach to a Patient with Dementia 1 August 3, 2013 o May already exhibit hallucinations and delusions (defend their delusions) 3. Severe Alzheimer’s Disease o Cannot use or understand words o Cannot recognize who they are when they look in the mirror o Cannot recognize family members o Cannot care for themselves I. CORTICAL DEMENTIA Types of dementia (for age group > 65) o Alzheimer’s disease 43% o Frontotemporal 11% o Lewy Body 15% o Vascular (stroke related, etc.) 30% A. ALZHEIMER’S DISEASE Most common type of dementia worldwide (affects elderly patients 60 years old and above) Almost half of people above 85 years old have Alzheimer’s disease Impaired cognitive functioning and activities of daily living (difficulty handling money, taking public transportation) Neurodegenerative disease with no known cure Insidious onset (gradual and progressive, months to years unlike stroke/vascular dementia – sudden) ABCs of Alzheimer’s o Activities of daily living impaired o Behavioral and Psychiatric symptoms (usual reason for consult) o Cognitive impairment (usually the first one to manifest) Cognitive loss in 2 or more domains: memory (recent memory affected first), language, calculation, orientation, and judgment o Memory is erased backwards Sufficiently severe to cause social or occupational disability o Difficulty bathing, grooming, toileting, can’t count change, loses wallet Figure 1. Natural history of Alzheimer’s Disease. Medication slows down loss of functional independence due to AD. However, the course still remains the same across cultures. Patient is symptomatic for 1-2 years and experiences mild cognitive impairment. There is a gradual progressive decline but early intervention can lead to period of longer functional independence. Death from complications o Progressive debilitation, bedsores (usually bedridden at end stage) o Malnutrition o Dehydration o Pneumonia o Urinary infections o Alzheimer’s itself can kill – neurons of respiratory center die out GROSS BRAIN ATROPHY Gross cortical atrophy, prominent gyri, and deep sulci Often affects the temporal, parietal and frontal Usually, first manifestation is bitemporal hypometabolism More prominent atrophy of hippocampus, entorhinal complex, and limbic structures Note: without a hippocampus, there is no formation of new memory Starts from hippocampus frontal parietal temporal CLINICAL COURSE Mean survival after onset: 10.3 years Survival range: 2 - 20 years Gradual cognitive decline Most patients evolve through stages: 1. Mild Alzheimer’s Disease o Say the same thing over and over o Lose orientation even in familiar places (e.g. at the home, at the mall) o Lose interest in things they once enjoyed (e.g. bathing) o Have trouble finding names for common items o Lose things more often than normal (esp. money) o Undergo personality changes (have simplistic thoughts) 2. Moderate Alzheimer’s Disease o More confused about recent events o Have difficulty with simple daily activities like dressing, eating o Argue more often than usual o Believe things are real when they are not o Require close supervision o Display anxiety or depression TRANSER, TRANSER, TRANSER Page 1 / 7 Lec 1: Dementia and Other Neurological Disorders Figure 2. Brain of a normal individual and a patient with Alzheimer’s Disease. Note the deepening of the sulci and loss of brain matter (cortical atrophy). Figure 3. Hippocampal atrophy. These are MRI scans showing hippocampal atrophy can still be present even if memory gap is not severe, and this is usually the first sign of mild AD. To be symptomatic, at least 50% of neurons must have died. The hippocampus is critical for the formation of new memories and consolidation of information from short term to long term memory. OS 213 Amyloid forms tangles caspases are activated and induce cell death Always asked! o Neuritic plaques (outside neuron) Amyloid plaque outside neuron induces inflammation Always asked! o Granulovacuolar degeneration and amyloid angiopathy Amyloid is abnormally accumulated in AD (don’t know yet if it’s due to abnormal production, folding, or degeneration) o Neurofibrillary tangles and amyloid plaques from outside neurons will eventually: Choke the cells until they can no longer function well Attract interleukins inflammation cells eventually die Activate caspases cells programmed to die “Wherever there is amyloid, there is death and damage to neuron.” (Anlacan, 2011 and 2013) o The more amyloid, the worse the AD Controlling hypertension, DM, and dyslipidemia decreases chances of getting AD. Figure 5. Neuropathological finding. Left: neurofibrillary tangle (arrow). Right: neuritic plaques. PATHOLOGICAL FEATURES Trivia: Famous people who had Alzheimer’s include Ronald Reagan and Margaret Thatcher. B. FRONTOTEMPORAL DEMENTIA Personality change is the primary manifestation, not memory loss. Memory problems develop later on. Usual psychiatric patients (psych problems manifest first). Strikes relatively young patients (40-60 y/o) Behavioral features include: o Personality changes o Disinhibition o Psychosis Cognitive features (executive dysfunction) include: o Loses ability to plan and organize o Forgets the steps in bathing and other activities of daily living o Prone to repetitive behaviors and collection mundane items (e.g. nail biting, collecting broken bottles, hoarding tansans) Symptomatic treatment only; no known cure GROSS BRAIN FINDINGS Figure 4. Pathophysiology of Alzheimer’s Disease. Accumulation of A-beta has several effects on neurons and neuronal function. Small aggregates of A-beta can alter neurotransmission, and the aggregates can be toxic to neurons and synaptic endings. Larger deposits, in the form of plaques, also lead to neuronal death through activation of caspases, elicit a local inflammatory response that can result in further cell injury, and may cause altered region to region communication through mechanical effects on axons and dendrites. The presence of A-beta also leads neurons to hyperphosphorylate the microtubule binding protein tau. With this increase level of phosphorylation, tau redistributes within the neuron from the axon into dendrites and cell body and aggregates into tangles. This process also results in neuronal dysfunction and cell death. The anatomic distribution of these changes, which occur roughly in parallel, are responsible for the clinical signs and symptoms. They appear to develop well in advance of clinical presentation. The process of degeneration from Alzheimer’s is as follows: o Beta-secretase cleaves the APP molecule producing amyloid, which then accumulates Amyloid causes activation of caspases resulting in the cleavage of tau protein Tau proteins aggregate to form NF tangles NF tangles cause neuronal cell death. Microscopic features include: o Neurofibrillary tangles (inside neuron) AICA, LEA, JEBBICK Figure 6. Frontotemporal dementia. A brain scan shows severe atrophy of the frontotemporal lobe. C. LEWY BODY DEMENTIA CORE FEATURES Parkinsonism with dementia o Parkinsonism may be concurrent or it may precede dementia o Onset of dementia at a point within a year of Parkinsonism Onset: any age Parkinsonism has milder symptoms, especially in the morning/waking hours, compared to true Parkinson’s disease Visual hallucinations of people and animals: most striking finding because hallucinations are very vivid and repetitive Page 2 / 7 Lec 1: Dementia and Other Neurological Disorders OS 213 Fluctuating attention and cognition (awake for 2 days and asleep for the next 2 days) Prognosis: rapid decline Other suggestive symptoms include: o REM movement disorder Shouting, biking in the air, bites caregiver while sleeping, etc. Important to rule out seizures o Parkinsonism: bilateral manifestation o Parkinson’s Disease: starts from one side, then crosses HISTOPATHOLOGY Single, multiple, intracytoplasmic, eosinophilic, round to elongated inclusions that often have a dense core surrounded by a pale halo (Lewy body) Ultrastructurally, Lewy bodies are composed of fine filaments, densely packed in the core but loose at the rim Lewy bodies may also be found in the cholinergic cells of the Basal Nucleus of Meynert, as well as in other brainstem nuclei Figure 8. Features of Parkinson’s Disease. Stooped-over posture, speaks in whispers, takes small steps PATHOPHYSIOLOGY Figure 7. Gross and histologic presentation of Lewy Body Dementia. On the left, note loss of substantia nigra (which explains Parkinsonism), and the presence of Lewy bodies (arrow) on the right. II. SUBCORTICAL DEMENTIA A. PARKINSON’S DISEASE DEMENTIA (PDD) Incidence of dementia in PD may be as high as 6 times more than in the general non-PD population 25% of patients will develop dementia of the AD type due to overlap of these two pathologies PDD patients are more likely to have akinetic/rigid PD phenotype rather than the tremor-predominant phenotype It will usually take at least 5 years for a patient with PD to have memory deficits. The executive functions are the first to go. Trivia: Prominent people who have atypical Parkinson’s disease include Michael J. Fox (diagnosed with juvenile Parkinson’s; he had no facial expressions) and Muhammad Ali, who acquired the disease from boxing (chronic traumatic encephalopathy with development of dementia fugilistica). Figure 9. Parkinson’s Disease. Substantia nigra as seen in Parkinson’s Disease. In LBD and PDD, abnormal protein (alpha synuclein) deposits disrupt the brain’s normal functioning. These Lewy body proteins are found in an area of the brainstem where they deplete the neurotransmitter dopamine, causing Parkinsonian symptoms. In Lewy body dementia, these abnormal proteins are diffuse throughout other areas of the brain, including the cerebral cortex (basically same abnormal protein in both diseases but accumulate in different areas). FEATURES OF PARKINSON’S DISEASE DEMENTIA Tremor (resting tremor, postural tremor) Rigidity Bradykinesia Unilateral (as compared to Parkinsonism which is bilateral) Postural instability (flexed posture, impaired postural reflex) Other features include expressionless face (hypomimia), greasy skin, and soft rapid indistinct speech Tremor, rigidity, and bradykinesia respond well to therapy unlike postural instability Give Levodopa and Carbidopa Figure 10. Parkinson’s Disease. During movement, signals pass from the brain’s cortex, via reticular formation and spinal cord (pathway A), to muscles, which contract. Other signals pass, by pathway B, to the basal AICA, LEA, JEBBICK Page 3 / 7 Lec 1: Dementia and Other Neurological Disorders ganglia; these damp the signals in pathway A, reducing muscle tone so that movement is not jerky. Dopamine, a nerve transmitter made in the basal ganglia, is needed for this damping effect. In Parkinson’s disease, degeneration of parts of the basal ganglia causes a lack of dopamine within this part of the brain. The basal ganglia are thus prevented from modifying the nerve pathways that control muscle contraction. As a result, the muscles are overly tense, causing tremor, joint rigidity, and slow movement. Most drug treatments increase the level of dopamine in the brain or oppose the action of acetylcholine. OS 213 Dementia (mild to moderate) Incontinence Triad of dementia, ataxia, and incontinence o Do not wait for full triad before treating May respond to shunting (prognosis better if symptoms are reduced by relief of pressure). Thus partially reversible. May be a post traumatic sequelae Presumed to be caused by obstruction to normal flow of CSF over the cerebral convexity and delayed absorption into the venous system resulting to enlarged lateral ventricles and stretching and distortion of white matter tracts in corona radiata In contrast to AD, NPH patient has early and prominent gait disturbance and has no evidence of cortical atrophy on CT or MRI GROSS BRAIN FINDINGS Neuroimaging studies reveal enlarged lateral ventricles with little or no cortical atrophy o Communicating hydrocephalus with patent aqueduct of Sylvius o Ventriculomegaly Lumbar puncture opening pressure is in the high normal range Figure 11. Dopaminergic cell death. Accumulation of alpha-synuclein leads to death of dopaminergic neurons. B. HUNTINGTON’S DISEASE Not very common Affectation of the caudate nucleus Autosomal dominant form of inheritance o If none is inherited, then you’re probably safe from this disease o Since it’s autosomal dominant, usually parents with Huntington’s are advised not to have children anymore Movement disorder: choreiform movements (“shaker”) Progressive dementia, with psychotic symptoms Characterized by motor abnormalities and fewer language abnormalities Psychomotor slowing and difficulty with complex tasks, but memory, language, and insight remain relatively intact in the early and middle stages of the illness Distinguished from AD type with the ff: o High incidence of depression and psychosis o Classis choreoathetoid movement disorder Important differential is X-linked dystonia; inquire family history or if clan hails from Panay island Figure 12. Normal pressure hydrocephalus. CSF has no way out so a shunt must be placed. This can bring them back to functional level. However, in very severe cases, shunting could not be done. E. WHITE MATTER DISEASES Dementia is a common occurrence in patients with disorders affecting cerebral hemispheric white matter (e.g. strokes, multiple sclerosis, HIV encephalopathy, leukodystrophies) o White matter hyperintensities on MRI are hallmark of HIV encephalopathy Pathological findings include numerous ischemic areas prone to stroke (due to very “bad” vessels) with loss of myelin C. PROGRESSIVE SUPRANUCLEAR PALSY Also known as Steele-Richardson-Olszewski Syndrome Uncommon type of dementia Loss of balance (falls) Vertical gaze difficulties usually come first (can’t look up or down) o Note: if there are problems in vertical gaze, think midbrain; if in horizontal gaze, think pons o Rule out pineal/quadrigeminal plate tumor which can also cause impaired vertical gaze Dementia, slurring, choking (cause of death: choking) Brain MRI reveals midbrain atrophy (superior colliculus) due to widespread neuronal loss which also affects globus pallidus, subthalamic nucleus, substantia nigra, periaqueductal gray matter, and dentate nucleus of the cerebellum PET studies show symmetric frontal and striatal hypometabolism Figure 13. HIV Leukoencephalopathy. The MRI shows atrophy and white matter hyperintensity on T2 not involving U-fibers. This 40-year old female patient is diagnosed with HIV and presented with confusion, decline in memory without focal findings, and dehydration E. MULTIPLE SYSTEM ATROPHY FEATURES WITH MSA D. NORMAL PRESSURE HYDROCEPHALUS FEATURES OF NORMAL PRESSURE HYDROCEPHALUS Gait problems (ataxia/apraxia, with wide based/”magnetic” gait) AICA, LEA, JEBBICK Also known as olivopontocerebellar atrophy Include all other syndromes that could not be classified back in the days (i.e. Shy-Drager syndrome) Ataxia is a manifestation Relatively rapid progression Autonomic dysfunction o Orthostatic hypotension (all patients will have this) o BP of patient from lying to sitting/standing should increase but in orthostatic hypotension, it decreases o Incontinence Parkinsonism Page 4 / 7 Lec 1: Dementia and Other Neurological Disorders Group of disorders with the presence of glial cytoplasmic inclusions typically within the cytoplasm of oligodendrocytes, that can have different patterns of clinical presentation No medications to stop the atrophy OS 213 ENDOCRINOPATHIES Hyper/hypothyroidism o Hypothyroidism is very common in patients who undergo thyroidectomy but fail to follow up Parathyroid/adrenal disturbances GROSS BRAIN FINDINGS B. TOXIC AND METABOLIC CAUSES Figure 14. Multiple system atrophy. In cerebellar forms, there is typically atrophy of cerebellum, including the cerebellar peduncles, pons (especially the basis pontis), and medulla (inferior olive), while in Parkinsonian forms, the atrophy involves both the substantia nigra and striatum (putamen). G. SUBCORTICAL DEMENTIAS Spinocerebellar degenerations Cerebellar + memory + frontal dysfunctions Idiopathic basal ganglia calcifications (may be asymptomatic) Cortico-basal ganglionic degeneration (“alien hand syndrome”; can’t recognize half of the body) Pseudodepression Wilson’s disease, along with Sydenham’s Chorea of Rheumatic Fever, is a differential diagnosis for very young children who move too much and is caused by a ceruloplasmin problem Vascular dementia (e.g. from hypoxic encephalopathy) Vitamin deficiencies (deficiencies in B1, B12, folate, niacin) o Vitamin B12 deficiency is not common in the Philippines because most of us are not vegetarians who need vitamin B12 supplementation o B1 deficiency – alcoholics Drugs that cause dementia include: o Psychotropic agents o Anticholinergics o Anti-convulsants Heavy metals and toxins (esp. common in those from the mining and gold rush districts or those exposed to lead) IV. REVERSIBLE DEMENTIAS Drugs and toxins Metabolic dementias Normal pressure hydrocephalus Tumors Infections SLE Endocrinopathies Vitamin deficiencies Alcoholism (mammillary bodies shrink) Pseudodementia (like those seen in depression) V. RAPIDLY PROGRESSING DEMENTIAS H. DISTINGUISHING CORTICAL FROM SUBCORTICAL DEMENTIA Figure 15. Various forms of rapidly-progressing dementia. The terminology prion refers to an infections protein agent that “replicates” by inducing the misfolding of the native polypeptides which leads it to take on a dysfunctional form A. NON-PRION DISEASES These include: o Corticobasal ganglionic degeneration o Frontotemporal dementia o Lewy Body dementia o Alzheimer’s disease o Progressive Supranuclear Palsy Creutzfeldt-Jakob disease is not synonymous to Mad Cow Disease CJD has been present even before MCD. CJD has been demonstrated in the Kuru tribe in Papua New Guinea where they open skulls of cows and eat the brains. MCD is under Variant CJD. It is a disease of cows that has been transmitted to people. It has younger age of onset, more rapid progression, and leads to ataxia and earlier death. B. PRION DISEASES III. TOXIC METABOLIC DEMENTIAS A. ETIOLOGY FROM SYSTEMIC ILLNESS Chronic hypoxia - can be caused by too much smoking Hepatic encephalopathy - can be caused by hyperammonemia Uremia (elevated creatinine) Persistent electrolyte imbalance (i.e. hyper/hyponatremia) SPORADIC CREUTZFELDT-JAKOB DISEASE AICA, LEA, JEBBICK Occurs between 50-70 years old Page 5 / 7 Lec 1: Dementia and Other Neurological Disorders Mean survival of 5 months 85% die witching a year of diagnosis Prion disease is not the same as mad cow disease Dementia + 2 of the ff: o Pyramidal or extrapyramidal symptoms o Visual/cerebellar dysfunction (mainly) o Myoclonus Startle myoclonus using clap as stimulus - feet/whole body jerks when startled Most common in Filipino patients o Akinetic mutism o EEG: periodic sharp waves This is diagnostic of SCJD Different from epilepsy since it does not respond to AEDs o CSF 14-3-3 protein elevation A very expensive diagnostic test Confirm to prognosticate VARIANT CREUTZFELDT-JAKOB DISEASE Transmitted from cows to humans Occurs in 12-74-year olds Includes Mad Cow Disease Early and profound psychiatric illness which is followed by: o Ataxia (e.g. some die by head injury) o Dementia o Movement disorder (myoclonic jerks) o EEG: no periodic sharp waves (usually normal) o MRI: Pulvinar sign can be seen (unlike SCJD which is usually normal) Figure 16. Pulvinar sign. 33-year old woman with VCJD. Axial fluidattenuated inversion recovery MRI shows high signal intensity bilaterally in pulvinar and medial aspects of thalamus (arrows). VI. APPROACH TO PATIENT WITH DEMENTIA HISTORY Check patient’s instrumental and daily activities: o Everyday problem solving o Handling business and financial affairs o Job responsibilities o Shopping o Participation in volunteer and social groups o Home activities, hobbies o Maintenance of personal hygiene o Intake of medications o Phone dialing o Traveling alone; knowing destination o Handling money Important to assess is impact on patient’s daily activities, which will help differentiate between normal and pathologic forgetfulness Alzheimer’s can occur as early as 40s if there is history of trauma OS 213 Early mutism Lateralizing signs o e.g. hemiplegia (caused by vascular dementia) and stroke or subdural hematoma on one side Refer dementia patients with red flags WORK-UP CBC with platelet count ESR Urinalysis Cholesterol, lipids VDRL/TPA – neurosyphilis but no cases the past 5 years HgbA1c, electrolytes BUN, creatinine Serum B12, folate LFTs, TFTs ECG 2D Echo Carotid/Vertebral Doppler Cranial MRI Toxic screening NOTE: The most important procedure to be done is the MRI. If it cannot be performed, CT-Scan will do. These are important because the patient may have had trauma or vehicular accidents. TEST EEG Lumbar Puncture (Neurosyphilis, TB meningitis) Heavy metal screen HIV screen Ceruloplasmin ApoE4 (susceptibility gene) / Genetic testing INDICATION Possible seizures: CJD Onset before 55 y/o: rapid progression of dementia History of potential exposure History of potential exposure Wilson’s disease To strengthen diagnosis; strong family history ApoE4 is a susceptibility gene. It doesn’t mean that if you have it, you have dementia. PET Scan with amyloid screening Diagnostic test for Alzheimer’s disease Table . Optional laboratory work-ups. Only done when other comorbids/etiologies are suspected. Biomarkers: PET Scan with amyloid screening, CSF testing PREVENTION Ballroom dancing (you use your body and your mind) Low fat diet, high in omega 3 Memoplus Gold = NO approved therapeutic claims Sufficient hours of sleep After 26 years, difficult to memorize things already Question: What if there are normal findings but presented with signs of cognitive degradation? Answer: Probably Alzheimer’s! END OF TRANSCRIPTION Greetings Aica: Hi Phive Star! Hello Harvey and Extra D’yiz! Lea: Punta kayo IMDC please and support our class! Yay! NEUROLOGIC EXAMINATION Check for the ff: o Aphasia (speech) o Apraxia (motor memory) o Agnosia (sensory recognition) o Executive functioning (complex behavior sequencing) o Judgment and insight (MSE) o Complete cranial nerve testing o Complete motor testing o Tremors, gait disturbances o Orthostatic hypotension (check for multiple system atrophy) RED FLAGS Early gait disturbances – comes late in Alzheimer’s Early incontinence – comes just before patients become bedridden AICA, LEA, JEBBICK Page 6 / 7 Lec 1: Dementia and Other Neurological Disorders OS 213 APPENDIX. Diagnostic work-up for dementia. Screen for treatable causes of dementia. If treatable, treat. o Example of atypical features: hemiparesis, which could indicate stoke leading to vascular dementia bad gait, but this occurs at later stages of Alzheimer’s AICA, LEA, JEBBICK Page 7 / 7