Directed reading answers (Chapter 15-16)
advertisement

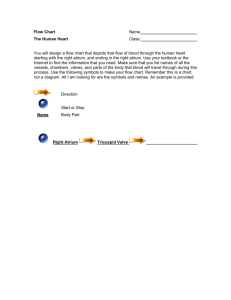
Directed Reading Chapter 15: The Cardiovascular system & assessment 1. The right atrium receives what type of blood? The left atrium receive what type of blood? a. The right atrium receives deoxygenated blood from the veins of the body via the superior and inferior venae cavae. The right atrium is separated from the right ventricle by the tricuspid valve. When open, deoxygenated blood flows through this valve into the right ventricle, which then pumps it through the pulmonary artery to the lungs b. The left atrium receives freshly oxygenated blood from the lungs through the pulmonary veins. The left ventricle, separated from the left atrium by the bicuspid or mitral valve, pumps this freshly oxygenated blood out the aorta to the systemic circulation. 2. The right side of the heart pumps blood to what part of the body? The left side of the heart pumps blood to what part of the body? a. See above reading 3. What 3 factors determine peripheral vascular resistance? a. Arterial circulation is maintained by a balance of blood flow, peripheral vascular resistance, and blood pressure. Blood flow is the amount of blood transported. b. Peripheral Vascular Resistance (PVR) is the force opposing blood flow. PVR is determined by three factors: i. Blood viscosity (thickness): The greater the viscosity of the blood, the greater its resistance to moving and flowing. ii. Vessel length: The longer the vessel, the greater the resistance to blood flow. iii. Vessel diameter: The smaller the vessel is, the more friction is produced, and the greater the resistance is to blood flow. 4. What affect does an increase in renin/angiotensin (released by the kidneys) have on blood pressure? a. The kidneys help regulate BP. A fall in BP stimulates the renin-angiotensin-aldosterone mechanism, causing vasoconstriction and salt and water retention. Antidiuretic hormone (ADH) from the pituitary gland promotes water retention, increasing blood volume, cardiac output and blood pressure. 5. What affect does and increase in antidiuretic hormone released by the pituitary have on blood pressure? a. See above #4 Document1 3/23/2016 1 6. As a person ages, what changes occur with their heart rate (especially when they exercise)? a. Many older adults experience occasional early heartbeats, although the rate remains basically regular. Although many older adults become more sedentary, regular exercise such as walking, swimming, and weight training is encouraged. The heart rate does not respond as rapidly to exercise and physical activity, requiring longer warm-up and cooldown periods. 7. On an 12-lead ECG, how much time is a small box? 1 large box? How many large boxes make 1 second? a. 1 large box or 5mm = 0.2 seconds b. 1 small box or 1 mm = 0.04 seconds c. Five large boxes represent 1 full second 8. Label the parts of an ECG (P wave, QRS complex, T wave, P-R interval) a. Done in class 9. What are the 3 main risks of angiography? a. Risks associated with insertion of the catheter into a high-pressure artery include i. Bleeding from the insertion site ii. Clot formation at the insertion site iii. And impaired blood flow to the extremity 10. What do you need to tell a patient for whom the doctor has ordered a lipid profile to be done? a. These tests should be performed fasting. Instruct the client to refrain from eating or drinking (sips of water are allowed) for 12 hours before testing and to avoid alcohol intake for 24 hours before testing Chapter 16 1. What is the leading risk factor for CHD? a. Cigarette smoking is the leading independent risk factor for coronary heart disease. It is a primary target of risk factor management for people of all age groups. 2. Which lipoproteins are good and which are bad? a. High blood lipids (hyperlipidemia) increase the risk for CHD. Lipoproteins carry cholesterol in the blood. Low density lipoproteins (LDL) is the primary carrier of cholesterol. High levels of LDL promote atherosclerosis because LDL deposits cholesterol on the artery walls. In contrast, high density lipoprotein (HDL) helps clear cholesterol from the arteries, transporting it to the liver for excretion. HDL levels above 35 mg/dL reduce the risk of CHD. Document1 3/23/2016 2 b. To help you remember which lipoproteins are “good” or desirable, and which are “bad” or undesirable, use the following i. LDL = less healthy ii. HDL = highly healthy 3. What is the primary cause of CHD? a. Atherosclerosis is the primary cause of coronary heart disease 4. What is angina Pectoris? What is the primary cause? a. Angina pectoris is chest pain that occurs when there is a temporary imbalance between myocardial blood supply and demand. Angina often occurs in a pattern: exercise brings on pain, rest relives the pain. 5. What is the drug of choice to treat an angina attack? a. Sublingual nitroglycerin (NTG) is the drug of choice to treat acute angina attacks, acting within 1 to 2 minutes. 6. What long term angina medication is contraindicated in a patient with asthma or COPD? a. Beta blockers may significantly slow the heart rate and are contraindicated for clients with asthma or severe chronic obstructive pulmonary disease (COPD) because they may cause severe bronchospasm in these clients. 7. What medication is frequently prescribed to patients with angina to decrease the risk of clot formation? a. The client with angina, particularly unstable angina, is at risk for myocardial infarction because of significant narrowing of the coronary arteries. Low-dose aspirin (81 mg/day) is often prescribed to reduce the risk that clots will form in narrowed arteries, causing myocardial infarction. 8. Why is giving oxygen part of the nursing interventions for a patient with a nursing diagnosis of decreased cardiac tissue perfusion? a. Supplemental oxygen reduces myocardial hypoxia 9. What procedures would the nurse perform before a client had an angiography or angioplasty procedure? a. Assess knowledge and understanding of the procedure. Reinforce teaching and provide additional information as needed. b. Provide routine preoperative care as ordered c. Administer ordered cardiac medications with a small sip of water before the procedure unless contraindicated Document1 3/23/2016 3 d. Document and report any allergies to iodine, radiographic dyes or seafood e. Explain that client will remain away during the procedure, which lasts 1 – 2 hours. Sedation may be given, and a local anesthetic will be used where the catheter is inserted. A sensations of warmth (a “hot flash”) and metallic taste may be experiences as the dye is injected. A rapid pulse or a few “skipped beats” also are common during the procedure. 10. What procedures would the nurse perform after a client had an angiography or angioplasty procedure? a. Provide routine postoperative care b. Monitor vital signs, distal pulses, color, movement sensation, temperature and capillary refill of affected extremity as ordered, usually every 15 minutes for the first hour, 30 minutes the next hour, hourly for 8 hours and then every 4 hours. c. Monitor cardiac rhythm continuously. Report dysrhythmias, ECG changes or chest pain to the charge nurse or physician d. Maintain bed rest with the affect extremity extended and the head of the bed elevated no more than 30 degrees e. Keep pressure dressing in place over the arterial access sites. Place a 5 pound sandbag over the access site for 6 hours or as ordered. Check frequently for bleeding (if the access site is in the groin, check for bleeding under the buttocks) f. Unless contraindicated, encourage liberal fluid consumption g. Administer medications as ordered h. Monitor intake and output, and laboratory values. Report abnormal values to the physician. Document1 3/23/2016 4