CHEMICAL MEDIATORS OF INFLAMMATION
advertisement

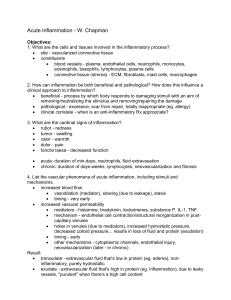
CHEMICAL MEDIATORS OF INFLAMMATION Definition: Any messenger that acts on blood vessels, inflammatory cells, or other cells to contribute to an inflammatory response. (Pretty much anything...) • Exogenous – Endotoxins • Endogenous – – – – Plasma Leukocytes Endothelial cells Fibroblasts CHEMICAL MEDIATORS OF INFLAMMATION Facts • Mechanism of action – Receptor-ligand interactions (1o) – Direct enzymatic activity – Mediate oxidative damage • Extensive network of interacting chemicals • High degree of redundancy • Guarantees amplification and maintenance of inflammatory response • Short t ½ and are harmful CHEMICAL MEDIATORS • Vasodilation – Prostaglandins, Nitric Oxide • Increased Vascular Permeability – Vasoactive amines (histamine, serotonin), C3a and C5a, Bradykinin, Leukotrienes, PAF, • Chemotaxic Leukocyte Activation – C5a, LTB4, Chemokines CHEMICAL MEDIATORS OF INFLAMMATION The Basics • Fever – IL-1, IL-6, TNF, Prostaglandins • Pain – Prostaglandins, Bradykinin • Tissue Damage – Neutrophil and Macrophage products – Lysosomal enzymes – Oxygen metabolites – NO VASOACTIVE AMINES • Increase Vascular Permeability and Vascular Permeability • Histamine and Serotonin – Mediators in the immediate active phase of increased permeability – Promotes contraction of smooth muscle – Stimulates to cells to produce eotaxins – Serotonin found in rodent mast cells Vasoactive Amines Continued • Releasing Stimulators – Direct physical or chemical injury – Binding of IgE- Agcomplexes – Fragments of C3a and C5a – Histamine releasing factors (pmn’s and θ) – Cytokines (IL-1, IL-8) PLASMA PROTEASES 3 interrelated systems are active within this category 1. Kinin system – Highly vasoactive 2. Complement system • Vasoactive • Chemotactic 3. Clotting system • Vasoactive • Cleaves C3 COMPLEMENT SYSTEM • Plasma proteins - act against microbial agents • Products of activated complement – – – – Vascular permeability Chemotaxis Opsonization Lysis COMPLEMENT SYSTEM Few reminders • • • • Classical pathway Alternate pathway Common pathway Important inflammatory mediators – C3a and C5a (anaphylatoxins) – Cause release of histamine from mast cells – Lysosomal enzyme release in inflammatory cells – C5a – Activates lipoxygenase pathway – Chemotactic many inflammatory cells – Increases adhesion of leukocytes COMPLEMENT SYSTEM And Inflammation • C5b-9 membrane attack complex – Lyses cells – Stimulates arachidonic acid metabolism – Produces reactive oxygen metabolites KININ SYSTEM BRADYKININ • Activated by Hageman factor (XIIa) • Bradykinin – Release of vasoactive nonapeptide bradykinin – Generated from the plasma • • • • • • Potent vasodilator Increased vascular permeability Contraction of smooth muscle Produce pain Stimulates release of histamine Activates the arachidonic acid cascade COMPLEMENT SYSTEM Few reminders • • • • Classical pathway Alternate pathway Common pathway Important inflammatory mediators – C3a and C5a (anaphylatoxins) – Cause release of histamine from mast cells – Lysosomal enzyme release in inflammatory cells – C5a – Activates lipoxygenase pathway – Chemotactic many inflammatory cells – Increases adhesion of leukocytes COMPLEMENT SYSTEM And Inflammation • C5b-9 membrane attack complex – Lyses cells – Stimulates arachidonic acid metabolism – Produces reactive oxygen metabolites COAGULATION SYSTEM Clotting system • Plasma proteins – Can be activated by Hageman factor • Thrombin converts fibrinogen to fibrin – Fibrinopeptides are formed – ↑vascular permeability – Chemotactic for leucocytes • Plasmin is important in lysing fibrin clots, – Activates Hageman factor (XII) ⇨ bradykinin – Cleaves C3 ⇨ C3a – "fibrin-split products" formed from fibrin breakdown – ↑ vascular permeability COAGULATION SYSTEM Clotting system • Plasma proteins – Can be activated by Hageman factor • Thrombin converts fibrinogen to fibrin – Fibrinopeptides are formed – ↑vascular permeability – Chemotactic for leucocytes • Plasmin is important in lysing fibrin clots, – Activates Hageman factor (XII) ⇨ bradykinin – Cleaves C3 ⇨ C3a – "fibrin-split products" formed from fibrin breakdown – ↑ vascular permeability HAGEMAN FACTOR Dependent Factors • Factor XII of intrinsic coagulation cascade • Activated by – Negatively charged surfaces – Platelets – Proteases from inflammatory cells • Causes – – – – – Coagulation Activation of fibrinolytic system Produces bradykinin Activates complement Provides an amplification system IMPORTANT NOTE • Activated Hageman factor (factor XIIA) initiates the clotting, fibrinolytic and kinin systems. The products of this initiation (kallikrein, factor XIIA, and plasmin, but particularly, kallikrein) can, by feedback, activate Hageman factor, resulting in significant amplification of the effects of the initial stimulus. ARACHIDONIC ACID METABOLITES • Roles in many biologic and pathologic processes – Inflammation • 20-carbon polyunsaturated fatty acid – Derived directly from dietary sources or by conversion of essential fatty acid linoleic acid • Esterified in membrane phospholipids – Must first be released from phospholipids • Via activation of cellular phospholipases – By mechanical, chemical and physical stimuli or by other mediators • 2 major pathways – Cyclooxygenase pathway – Lipoxygenase pathway. CYCLOOXYGENASE PATHWAY • 2 cyclooxygenase enzymes – COX-1 – COX-2 • 3 important products – Thromboxane A2 – Aggregates platelets and causes vasoconstriction – Prostacyclin (PGI2) – Endothelial cells inhibits platelet aggregation and causes vasodilation – Prostaglandins PGE2, PGF2 and PGD2 – Variety of actions on vascular tone and permeability LIPOXYGENASE PATHWAY Leukotrienes • Leukotrienes • Leukotriene B4 is a potent chemotactic agent • Leukotrienes C4, D4, E4 – Potent vasoconstrictors – Potent mediators of increased vascular permeability on venules only – Up to 1000 times as potent as histamine in producing increased vascular permeability • NOTE: – Some anti-inflammatory properties interfere with arachidonic acid metabolism – Corticosteroids interfere with phospholipase – Aspirin interferes with cyclooxygenase • • • • • PLATELET ACTIVATING FACTOR Aggregate platelets and cause release Bronchoconstriction and Vasoconstriction Vasodilation and ↑ vascular permeability ↑ leukocyte adhesion Leukocyte chemotaxis CYTOKINES • Transmitters for cell-to-cell chatting – Modulate cell function • Primarily from activated macrophages and lymphocytes • IL-1, IL-8, TNF IL-I and TNF “Master Cytokines” • Origin – Monocytes – Macrophages • • • • Similar in action Endothelium Acute phase proteins Fibroblasts Other Cytokines Chemokines??? • IL-5 – Eosinophils • IL-6 – B and T cells • IL-8 – Neutrophils – Lesser degree monocytes and eosinophils GROWTH FACTORS • Platelet derived growth factor • Transforming growth factor β – Chemokines - Leukocytes and Mesenchymal Cells • Important in regeneration and repair NITRIC OXIDE (NO) Just say NO! • Nitric oxide is synthesized from L-arginine • 2 enzymes and many factors produce NO • 3 effects – – – – – ♥♥ physical mediator of vascular tone Host defense (forms perroxynitrite) Signaling molecule – especially brain Reduces platelet aggregation and adhesion Inhibits several features of mast cell induced inflammation • Uncontrolled NO production – Can lead to massive peripheral -Vasodilation -Shock LYSOSOMAL CONSTITUENTS • Neutrophils, Monocyte/Macrophages – Enzymes and proteins within granules • Cationic proteins – ↑ vascular permeability – Chemotactic • Neutral proteases – Degrade ECM OXYGEN-DERIVED FREE RADICALS • • • • Cause endothelial damage Protein destruction by inhibiting antiproteases Injury to variety of cells Don’t forget the antioxidants – Ceruloplasmin – Transferrin – Superoxide dismutase – Catalase – Glutathione peroxidase