Headache forum Oct 28 thefemalemigraineur
advertisement

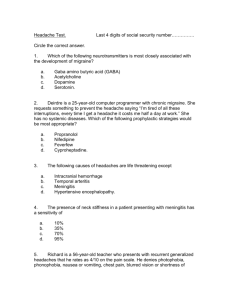
Migraine in the Female Life Cycle Headache Forum October 2007 Lucy Vieira MD Objectives Describe the changes in migraine prevalence and characteristics throughout the female lifecycle. Discuss the factors to consider in the treatment of the female migraineur. Perimenstrual migraine Perimenopausal migraine Migraine and the risk of stroke Incidence of migraine peaks in adolescence. Peak incidence females Migraine with aura: 12-13yo (14/1000 person-years) Migraine without aura: 14-17yo (19/1000 person-years) Stewart et. al. 1993. Amer J Epidemiol 34:1111-20 – the reported age of migraine incidence in a prevalence study Peak Incidence males •Migraine with aura: 5yo (6.6/1000) •Migraine without aura: 10-11yo(10/1000) Prevalence of Migraine •Before puberty: prevalence higher in boys •Until early adulthood incidence and prevalence continue to increase •Prevalence highest from 25-55 yo. Prevalence is stable in the USA over time. American migraine study-I- info from 15,000 homes in 1989 AMS-II – 1999. AMPP – 2005. prevalence mig: 18%F 6%M Lipton Headache 38:87-96 1998. Lipton Headache 41:646-57. Lipton Headache 45:792 2005 Burden of Migraine Individual: 25% of female migraineurs have>4 severe attacks/m - this associated with significant disability (need bed rest) Societal: loss of work productivity (13 billion/y) - healthcare use: 4% of all visits for headache -accounts for 1/3 of all OTC analgesic use. Lipton 2001 Headache 41: 638-45. Hu 1999 Arch Intern Med 159:813-18. Holmes 2001 Neurology 56(s 1):13-19 Case Study: Julia 27 year old Med Student Migraine since age 13 No Phx. No meds. Attacks are stereotypical migraine without aura. Occur once or twice a month, usually but not exclusively around menstruation. Menstrual migraine Pure menstrual migraine: migraine without aura that occurs on day 1+2 (d-2to+3) most cycles and no migraine at other times 10% Menstrually-related Migraine: as above but additional attacks with or without aura at other times of the cycle 40% Non-menstrual migraine 50% MacGregor EA Cephalalgia 1990 and 1996 Figure 117"> MacGregor, E. A. et al. Neurology 2006;67:2154-2158 Chance of migraine 2.5X more during days 1-3 of the cycle Figure 217"> MacGregor, E. A. et al. Neurology 2006;67:2154-2158 MacGregor E.A. et al., Neurology 2004;63:351-53 Pathophysiology of this incr. Risk of Migraine estrogen withdrawal – incr. Neuronal excitability Prostaglandin release Magnesium deficiency Martin VT Headache 2006;46:3-23 and 365-86 Martin V et al., Headache 2006;46:365-86 Estrogen and neuronal excitability Treatment with estradiol increases dendritic spine density in hippocampal neurons (female rat): incr. Excitatory input Cell membrane receptors (progesterone metabolite) Effects of estrogen on Purkinje cell response to glutamate (female rats) Smith Brain Res. 1988;475:272-282 Summary Martin and Behbehani. Headache 2006;46:365-86 PNAS 2001: 98:4687-4692 Ann Neurol 2004;55:276-80 Hormonal treatmentspremenopausal woman Goals: -prevent drop in estradiol? -produce anovulation? -add estrogen or progesterone that may have preventative effects? Estrogen and migraine Medical oophorectomy alone worsened headache while add back Estradiol improved headache. 100 mcg Estradiol patch is much better than 50 mcg Fluctuations in serum estrogen may be very important Martin V. Headache 2003;43:309-21 Perimenstrual Estradiol patch/gel 28 day cycle 28 day cycle Estradiol patch/gel days –2 to +7 •100 mcg patch better than 25 mcg – need to achieve plasma estradiol levels of 60-80 pg/ml. •May cause spotting and irregular menses. •Migraine shifted to when take off gel/patch. Granella F Cephalalgia 17:35-38,1997. MacGregor A Neurology 2006; 67:2159-63 Figure 118"> MacGregor, E. A. et al. Neurology 2006;67:2159-2163 Oral contraceptives Most composed of Ethinyl estradiol (synthetic estrogen that inhibits gonadotropin release) Progestins – derivatives of 10-Nortestesterone 1st gen – norethisterone 2nd gen – norgestrel, levonorgestrel 3rd gen – desogestrel, others 4th gen – drospirenone (anti-mineralocorticocoid effect) -derivative of spironolactone Formulations – triphasic, monophasic, extended duration Migraine and OCPs 1. Unchanged in half, worse in 30% and improved in 6% 2. Patients with aura more likely to worsen (50% vs 25%) 3. Aura may develop for the first time with OCPs. Martin V. Headache 2006; 46:365-86 Effect on MWA Patients experiencing attacks of MWA are more likely to worsen with administration of OCPs than those with MWoA. case reports have demonstrated that visual, sensory, and motor aura may develop for the first time in those receiving OCPs. Some patients with "new onset aura" or a "crescendo pattern" to their migraines after the start of OCPs have progressed to develop cerebrovascular accidents (CVAs). (Granella Cephalalgia 2000;20:701-7; Cupini Cephalalgia 1995;15(2):140144. Mousa Am J Optom Physiol Opt. 1982;59:821-23 ). Case#2 18 year old woman who is known to you for migraine with aura. She would like to take the BCP. Aura consists of progressive bright visual phenomena that evolve then disappear after 30 minutes. She has these about 4 times a year. She also has migraine without aura around the time of her period each month. Phx: negative Smoking: none Neurological exam and blood tests normal. How would you manage this patient? Migraine and stroke risk •Past studies have reported an increased risk of CVAs in patients with migraine headache •Esp. young women and MWA. •A recent meta-analysis reviewed 14 studies (11 case control and 3 cohort studies) to determine the relationship between migraine and risk of ischemic CVA. (Etminan M et al., BMJ 2005;330(7482):63) Stang PE, et al. Neurology. 2005;64(9):1573-1577. Tzourio C, Bousser MG. Stroke. 1997;28(12):2569-2570. Tzourio C, et al.,BMJ. 1993;307(6899):289-292. Chang CL, et al., BMJ. 1999;318(7175):13-18. Velentgas P, Headache. 2004;44(7):642-651. Pooled rel. risks of stroke stratified by migraine type, oral contraceptive use, and age Relative risk (95% CI) Ri* P value† All studies 14 2.16 (1.89 to 2.48) 0.00 0.77 Etminan, M Case-control studies 11 2.18 (1.86 to 2.56) 0.00 0.51 BMJ 2005;330:63 Cohort studies 3 2.10 (1.61 to 2.75) 0.00 0.96 2.27 (1.61 to 3.19) 0.49 0.08 1.83 (1.06 to 3.15) 0.60 0.04 8.72 (5.05 to 15.05) 0.26 0.28 No of studies Migraine (any) Migraine with aura Case-control studies 7 Migraine without aura Case-control studies 6 Migraine among oral contraceptive users Case-control studies 3 Migraine among men and women <45 years Case-control studies 9 2.36 (1.92 to 2.90) 0.07 0.38 Migraine among women <45 years Case-control studies 7 2.76 (2.17 to 3.52) 0.00 0.82 *Proportion of the total variance due to between study variance. Large values (>0.75) indicate large heterogeneity between studies; small values (<0.4) indicate lack of heterogeneity.7 Fig 1 Forest plot of the studies of migraine and ischaemic stroke Etminan, M. et al. BMJ 2005;330:63 Copyright ©2005 BMJ Publishing Group Ltd. Migraine as a risk factor for Stroke in young women (<45) (Absolute risk is about 2/100000/year) Migraine without aura Migraine with aura No aura + BCP* Aura + BCP* Aura + smoking Aura + BCP* + smoking Bousser, MG Stroke.2004;35(suppl I):2651-56 RR 3 6 6 12 12 35 *low estrogen+progesterone In migraineurs No absolute contraindication for the use of the BCP. Should be avoided in patients who smoke and esp. if there is aura. Stop or switch if aura develops or increases or if headache worsens after the first few weeks. In this patient Evaluate and discuss the risks of stroke. Use a low estrogen or progesterone only pill Monitor for the development of a more complicated or frequent aura – stop the pill Cardiovascular Safety of Triptans Contraindicated in pts with uncontrolled HTN, CAD, CVA, complicated aura Avoid in those with >2 risk factors Incidence of serious cardiovascular events is extremely low. Risk-benefit profile favors use in the absence of vascular risk factors. Triptan cardiovascular safety expert panel of the American Headache society – consensus statement. Headache 44(5):414, 2004 Management of Menstrual Migraine Acute therapy: NSAIDS or triptans Mini-prophylaxis starting 48 hours before expected headache or 10 days after ovulation and continuing up to one week: Increase dose of usual prophylactic Naproxen 500 mg BID triptans Estradiol gel 1.5 mg Qday Estradiol patch 100 mcg q3-4days Acute Rx: triptans Sumatriptan 100mg PO, 6mg s/c, rizatriptan, zolmitriptan, Naratriptan All effective in placebo controlled trials Short-term MM prophylaxis Mg Naproxen DHE-45 NS Estradiol gel Estradiol patch Sumatriptan Naratriptan Zolmitriptan 360 mg/d 550 mg BID NS q8h 1.5 mg Qday 100 mg 25 mg TID 1 mg BID 2.5 mg BID * Refers to before expected headache Day 15-menses Day -7 to +6 Day -2* to +4 Day -2* to +5 same day -2 to +3 Day -2 to +3 Day -2 to +4 Other treatments Increase the dose of the usual prophylactic meds Continuous OCP: elimination of the placebo week across 3-4 cycles (Silberstein Headache in clinical practice 2002: 100-107) Extended duration OCPs Sulak Headache 2007;47:27-37 Pregnancy Preexisting migraine most often improves with pregnancy. 48% to 79% of women with a history of preexisting migraine improve during pregnancy, particularly during the second and third trimesters Aura symptoms occur frequently during pregnancy in those with a past history of migraine. Several studies have reported "new onset" visual, sensory, and motor aura during pregnancy. the "high estrogen milieu" of pregnancy could play a role in initiating attacks of MWA. pts with "exclusively" MWA were less likely to have an improvement in migraine during pregnancy. Perimenopause: time period 2 to 8 yrs prior to menopause +1 year (WHO) menstrual cycles var., heavier menstrual bleeding, anovulation, and intermittent amenorrhea during this time. Levels of ovarian hormones may differ: lower progesterone No longitudinal diary studies Cross-sectional studies suggest: prevalence of migraine higher during perimenopause in pts with MWoA and premenstrual syndrome. (Mattsson Headache 003;43:27-35) Exogenous hormones: Postmenopausal women 50 year old woman with a past history of migraine without aura. Attacks were well controlled with Ibuprofen until last 12 months. Now occur 5-6 times per month. She thinks it’s due to the fact that her sleep is disturbed by hot flushes. She had one menstrual period in the last 6 months. She is constantly tired and feels sleep deprived. Her gynecologist does not want to give her hormone therapy because of her migraines. Hormone replacement therapy Effect on migraine depends on: 1. Preparation used and route of delivery 2. Dose used 3. Constancy of dosing 4. Concomitant use of a progestin Menopause no longitudinal cohort studies retrospective questionnaires of the effect of menopause on headaches: migraine improves in 8% to 36%, worsens in 9% to 42%, and remains unchanged in 27% to 64% at the time of menopause 8 to 13% develop migraine denovo Patients with a surgical menopause may do worse: 38% to 87% worsening of existing migraine. abrupt withdrawal of estrogen (surgical oophorectomy may be more provocative) Another potential explanation may be that the dose of estrogen replacement therapy used in surgically oophorectomized patients was too low to prevent migraine ( Martin 2006) Hodson J, Climacteric. 2000;3(2):119-124. Granella F,. Headache. 1993;33(7):385-389 HRT HORMONE REPLACEMENT THERAPY: natural, conjugated, and synthetic estrogens.(lower potency than those generally found in OCPs.) Natural estrogen preparations contain estrogens normally found with women (eg, β-estradiol). Conjugated estrogens are produced from animal and/or plant sources synthetic estrogens are synthesized estrogen derivatives (eg, ethinyl estradiol). The oral progestins include natural progesterone (eg, micronized progesterone) as well as synthetic progestins (eg, medroxyprogesterone). Oral progestins may be administered daily or for 10 to 12 days each month to prevent endometrial hyperplasia. routes of delivery of HRT include pills, transdermal patches/gels, subcutaneous implants or injections, and vaginal suppositories. HRT can improve migraine in 22% to 23%, worsen migraine in 21%, and leave it unchanged in 57% In a cross-sectional study of 17,107 postmenopausal women from the Women's Health Study: diagnosis of migraine was 1.44 times more likely in HRT users aura symptoms can develop secondary to estrogen replacement therapy in some patients. lowering the dosage of estrogen or changing to another type of estrogen replacement may lead to an abatement of aura symptoms. Hodson J Climacteric. 2000;3(2):119-124. Greendale GA, Obstet Gynecol. 1998;92(6):982-988. MacGregor A. Headache. 1999;39(9):674-678. HRT Dose: women who had a medical menopause only the 100-mcg patch was preventative of migraine. Type and Route of Administration: headache outcome worsened in patients receiving an oral conjugated estrogen and medroxyprogesterone, while they did not change as compared to baseline in those receiving a 50-mcg transdermal estradiol patch and medroxyprogesterone. HRTs containing conjugated estrogens are provocative for migraine, while those containing natural estrogens have less effect on migraine. transdermal routes of delivery may be superior to oral routes, since they maintain a more constant serum estradiol level HRT regimens using the same dosage of estrogens and progestins on a daily basis are superior to those using intermittent dosing of HRT. Nappi RE, Maturitas. 2001;38(2):157-163. Facchinetti F Headache.2002;42(9):924-929.