الشريحة 1
advertisement

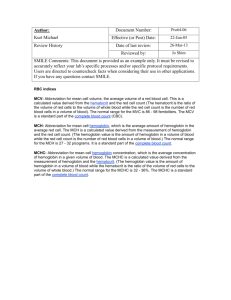
Packed Cell Volume of Whole Blood • Hematocrit is defined as the volume occupied by erythrocytes in a given volume of blood and is usually expressed as a percentage of the volume of the whole blood sample. • The hematocrit may also be referred to as Packed Cell Volume (PCV). Principle: • The hematocrit is usually determined by spinning a blood-filled capillary tube in a centrifuge. Specimen: • Venous blood anticoagulated with EDTA or capillary blood collected directly into heparinized capillary tubes can be used. Specimens should be centrifuged within 6 hours of collection. • Hemolyzed samples cannot be used for testing. Reagents and equipment: • Capillary tubes, heparinized for finger sticks (red tip) or plain for anticoagulated blood (blue tip) • Clay-type tube sealant • Microhematocrit centrifuge • Microhematocrit reader • Kimwipes or gauze Procedure: 1. Fill two capillary tubes approximately three quarters full with blood anti-coagulated with EDTA or heparin. Alternatively, blood for heparinized capillary tubes may be collected by capillary puncture. Wipe any excess blood from the outside of the tube. 2. Seal the end of the tube with the colored ring with nonabsorbent clay 3. 4. 5. 6. Balance the tubes in the centrifuge with the clay ends facing the outside away from the center, touching the rubber gasket. Tighten the head cover on the centrifuge and close the top. Activate the centrifuge for 5 minutes between 10,000 and 15,000 rpm (see comments). Do not use the brake to stop the centrifuge. Determine the HCT by using a microhematocrit reading device Read the level of RBC packing; do not include the buffy coat (leukocytes and platelets when reading. The values of the two Hcts should agree within 2% (0.02). Hematocrite Reader Reference ranges: •Newborn •Infant/child •Adult male •Adult female 53-65% 30-43% 42-52% 37-47% Sources of error and comments 1. Improper sealing of the capillary tube causes a decreased Hct reading as a result of loss of blood during centrifugation. a higher number of erythrocytes are lost in relation to the plasma. 2. An increased amount of anti-coagulant decreases the Hct reading as a result of erythrocyte shrinking. 3. A decreased or increased result may occur if the specimen was not properly mixed. 4. The time and speed of the centrifugation and the time when the results are read are very important. Insufficient centrifugation. Time for complete packing should be determined for each centrifuge and rechecked at regular intervals. 5. The microhematocrit centrifuge should never be forced to stop by applying pressure to the metal cover plate. This will cause the RBC layer to “sling” forward and results in a falsely elevated value. 6. If too much time elapses between when the centrifuge stops and the capillary tube is removed, the red cells can begin to settle out and cause a false reading of the hematocrit. 7. The buffy coat of the specimen should not be included in the Hct reading, because its inclusion falsely elevates the result. 8. A decrease or increase in the readings may be seen if the microhematocrit reader is not used properly. 9. A number of disorders such as: Sickle cell anemia Macrocytic anemia's Hypochromic anemia's Spherocytosis Thalassemia may cause plasma to be trapped in the erythrocytes even if the procedure was performed properly. 9. The trapping of the plasma causes the microhematocrit to be 1-3% (0.01-0.03 L/L) higher than that obtained on automated instruments, which calculate the Hct and are unaffected the trapped plasma. 10. A temporarily low Hct reading may result immediately after a blood loss, because plasma is replaced faster than erythrocytes. 11. Proper specimen collection is an important consideration. The introduction if interstitial fluid from a skin puncture or the improper flushing of a catheter causes decreased Hct readings. • are measurements that describe the size and oxygencarrying protein (hemoglobin) content of red blood cells. The indices are used to help in the differential diagnosis of anemia. • The relationships between the hematocrit, the hemoglobin level, and the RBC are converted to red blood cell indices through mathematical formulas. • The indices include these measurements: mean corpuscular volume (MCV); mean corpuscular hemoglobin (MCH); and mean corpuscular hemoglobin concentration (MCHC). Mean Corpuscular Volume • The MCV is the average volume of the RBC in femtoliters (fL), or 1015L: MCV = Hct (%) X 10 / RBC count (10-12/L). • Example: Hct = 45%, RBC count = 5.0x1012/L; therefore, • MCV = 45.0x10 / 5.0 = 90fL • Cells of normal size (MCV is 80-100fL) are called normocytic, smaller cells are microcytic, and larger cells are macrocytic. Microcytic cells are found in: Patients with iron deficiency anemia. Thalassemia. Macrocytic cells are found in: Patients with liver disease or hypothyroidism When there is asynchrony in RBC maturation (termed megaloblastic anemia's). Folate and vitamin B12 deficiencies. Mean Corpuscular Hemoglobin (MCH) • The MCH is the average weight of Hb in an RBC, expressed in the units of picograms (pg), or 10-12g: MCH = Hb (g/dL) X 10 / RBC count (1012/L). • The reference range for adults is 28-32pg. • The MCH is not generally considered in the classification of anemia's. Example: – Hb=16.0 g/fl. – RBC count=5.0x1012/l. – MCH=16.0x10 / 5.0 = 32.0pg Mean Corpuscular Hemoglobin Concentration (MCHC) • The MCHC is the average concentration of Hb in each individual erythrocyte. The • units used are gram per deciliter (formerly referred to as a percentage). MCHC = Hb (g/dL) X 100 / Hct (%). • Example: Hb =16 g /dl, Hct = 48%; • MCHC=16 X 100 / 48 = 33.3g/dL • Values of normochromic cells range from 32 to 37g/dL. • Hypochromic cells are less than 32g/dL, and those of hyperchromic cells are greater than 37g/dL. • Hypochromic erythrocytes occur in thalassemia and iron deficiency. • Because there is a physical limit to the amount of hemoglobin that can fit in a cell, there is no hyperchromic category, a cell does not really contain more than 37g/dL of Hb, but its shape may have become spherocytic, making the cell appear full.