File
advertisement

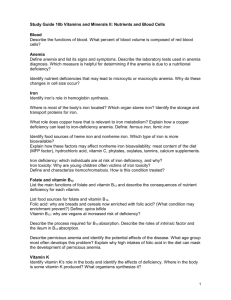
hematopoeisis Bone marow examination Normal bone marrow 1. Haemopoietic cells. Morphology of haemopoietic cells Granulocytes & their precursors – 60% Erythroid precursors – 20 % Lymphocytes & Monocytes & their precursors – 10% Unidentified or disintegrating cells – 10% 2. Myeloid : erythroid ratio – 3-4 :1 Anaemia Anaemia may be defined as a state in which the blood Hg is below the normal range fro the age & sex of the patient Normal count/Range Hemoglobin Male – 13 –18 gm/dl Female -11.5 – 16.5 gm/dl Red cell count – Male - 4.5–6.5 million/cu mm of blood Female – 3.8–4.8 Reticulocyte count - 0.2–2.0% Hemoglobin (Hb) Red cell count Reticulocyte count g/dL 13.6-17.2 12.0-15.0 ×106/mm3 % 4.3-5.9 0.5-1.5 3.5-5.0 0.5-1.5 Factors necessary for Erythropoiesis. A] General Factors 1] Diet-Protein is essential for synthesis of Globin in of Haemoglobin Iron-essential for heam production Others-Cu, Mg, Cobalt, Ca etc. 2] Hypoxia-hypoxia causes Liberation of hormone Erythropoietin which stimulate bone marrow for Erythropoiesis 3] Erythropoietin 4] Endocrine gland- Adrenal Gland, Pituitary Gland, Thyroid Gland. B] Maturation factors 1] Vit. B12 2] Folic Acid 3] Intrinsic Factor of Castle-It helps in absorption of Vit. B12 from gut and thus indirectly help in maturation. Classification of Anemia Morphological & Aetiological Classification Morphological classification Based mainly on MCV & MCHC. MCH may be included 1.Microcytic Hypochromic aneamia MCV, MCHC & MCH are below normal E.g. – IDA, thalassaemia, anaemia of chronic diseases 2. Macrocytic anaemia MCV is above normal . MCHC is normal E.g. megaloblastic anaemia 3. Normocytic Normochromic anaemia MCV, MCHC MCH are within normal range E.g. acute blood loss, haemolytic anemia Aetiological Classification This classification is based on pathophysiology & cause Impaired RBC production Hemolytic anemia Blood Loss Impaired RBC production A. Deficiency of essential nutrients (Deficiency anaemia) Iron deficiency – most common cause Vitamin B12 deficiency Folic acid deficiency Combined deficiency Others – protein calorie malnutrition , vitamin C deficiency B. Depression of erythropoiesis Anemia of chronic disease – Chronic renal failure . Liver diseases, Malignancy Invasion of bone marrow – leukaemia , secondary carcinoma Aplastic anemia B. Haemolytic anemia Intracorpuscular defect Extracorpuscular defect C. Blood Loss Acute Blood loss – loss of large volume of blood over a short period Chronic blood loss e.g hookworm infestation, bleeding peptic ulcer, piles, menorrhagia Clinical features of anemia Tiredness , Fatigue Lethargy Palpitaion Pallor is the most important physical sign Laboratory diagnosis of anemia Hb estimation Diagnosis of Morphological type of anaemia Diagnosis of aetiological type of anemia – discussed under individual type of anemia Packed cell volume (PCV) Is the volume of red cells in relation to that of whole blood PCV = MCV X red cell count Normal values 40 – 45 % male 37- 47 % female MCV (Mean corpuscular volumes ) Indicates the average volume red cells Normal 76 - 96 fl (femolitre) MCH (mean corpuscular hemoglobin ) Indicates average weight of Hb contained in each cell Does not take into count cell size Obtained by dividing Hb by red cell /liter & multiplied by 1013 If Hb 15g/dl Red cell – 5X1012/L MCH = 15X1013 / 5X1012 = 30 pg Normal 27-32 pg MCHC (mean corpuscular haemoglobin concentration) Indicates the average concentration of Hb within average red cells Usually 3 times higher that the whole blood Hb conc. Obtained by dividing Hb by PCV /liter If Hb 15g/dl PCV – 0.45l/l MCHC = 15/0.45 = 33.3g/dl Normal – 31-35 g/dl Diagnosis of morphological type of anemia 1. Examination of peripheral blood film 2. Determination of Red cell absolute value MCV & MCHC are below normal values – microcytic hypochromic anemia MCV is above normal & MCHC is normal – macrocytic anemia MCV & MCHC are normal – normocytic normochromic aneamia Iron deficiency anemia Most common type of anemia Total body iron content Male – upto 6gm Female – 2gm 80% of functional body iron is found in hemoglobin, rest found in myoglobin and iron-containing enzymes (e.g.catalase & cytochromes). The iron storage pool, represented by hemosiderin and ferritin-bound iron (15% to 20% of total body iron.) Stored iron is found mainly in the liver, spleen, bone marrow, and skeletal muscle. Male Fem Absorption Most absorbed in Duodenum Causes /pathogenesi of iron deficiency 1. Inadequate iron intake Nutritional deficiency – deficient diet 2. Impaired absorbtion – coeliac disease, tropical sprue, gastrectomy or gastro-enterostomy Causes /pathogenesi of iron deficiency 3. Increased physiological demand During period of growth in children During reproductive life in female – menstruation, pregnancy, parturation & lactation increase the physiological requirement fro iron 4.Chronic blood loss – the gastrointestinal tract (e.g., peptic ulcers, colonic cancer, hemorrhoids, hookworm disease) or the female genital tract (e.g., menorrhagia, cancers) Laboratory diagnosis of IDA Investigation & findings 1. Blood Picture Hb – Variably reduced Blood film – hypochromic, microcytic, anisocytosis. Poikilocytosis in severe cases target, elliptical, oval & pencil cells Haematocrit – reduced MCV – reduced(microcytosis) MCHC – reduced (hypochromic) & MCH is reduced 2. biochemical findings (confirm IDA) Serum iron - reduced Serum ferritin - reduced Total iron binding capacity – increased Percentage saturation of iron binding protein – decreased 3. Bone marrow Although erythropoietin levels are increased, the marrow response is blunted by the iron deficiency, and thus the marrow cellularity is usually only slightly increased Diagnostic criteria include Anemia, hypochromic and microcytic red cell indices, low serum ferritin and serum iron levels, low transferrin saturation, increased total iron-binding capacity, and, ultimately, response to iron therapy 4. Further Investigation Stool examination for Ova of hookworm & Occult blood Urine examination for haematuria Other investigations depending on clinical findings Megaloblastic aneamia MA are characterized by formation of morphologically abnormal (enlarged) nucleated red cell precursors called megaloblasts in the bone marrow. The change occurs due to deficiency of vitamin B12 or folate Vitamin B12 Abundant in all animal foods, including eggs and dairy products, and is resistant to cooking and boiling. Even bacterial contamination of water and non animal foods can provide adequate amounts. It is stored in the liver, which normally contains reserves that are sufficient to support bodily needs for 5 to 20 years As a result, deficiencies due to diet are rare and are virtually confined to strict vegans Metabolism of vitamin B12 Peptic digestion release dietary vitamin B12, Binds to salivary B12-binding proteins called R binders. R-B12 complexes transported to duodenum Processed by pancreatic proteases to releases B12, Attaches to intrinsic factor (gastric juice) The intrinsic factor-B12 complex passes to the distal ileum Attaches to the epithelial intrinsic factor receptors - absorption of vitamin B12. B12 bound to transport proteins called transcobalamins, which then deliver it to the liver and other cells of the body. Causes of Megaloblastic Anemia Vitamin B12 Deficiency Decreased intake Inadequate diet, vegetarianism Impaired absorption Intrinsic factor deficiency - Pernicious anemia, Gastrectomy Malabsorption states Diffuse intestinal disease e.g. lymphoma Ileal resection, ileitis Competitive parasitic uptake - Fish tapeworm infestation Bacterial overgrowth in blind loops and diverticula of bowel Increased requirement Pregnancy, hyperthyroidism, disseminated cancer Folate metabolism Best sources - fresh uncooked vegetables and fruits. The principal site of intestinal absorption is the upper third of the small intestine Conversion from dihydrofolate to tetrahydrofolate by the enzyme dihydrofolate reductase is particularly important. Tetrahydrofolate involved in the synthesis of purines and thymidylate, the building blocks of DNA, Megaloblastic anemia Folic Acid Deficiency Decreased intake Inadequate diet—alcoholism, infancy Impaired absorption Malabsorption states Intrinsic intestinal disease Increased metabolism Anticonvulsants, oral contraceptives Increased loss Hemodialysis Increased requirement Pregnancy, infancy, disseminated cancer, markedly increased hematopoiesis Impaired use Folic acid antagonists – e.g.Methotrxate Pathogenesis of Megaloblastic anemia Deficiency of Vit B12/folic acid Impairment of DNA synthesis, Results in a delay in nuclear maturation and cell division. Synthesis of RNA and cytoplasmic elements proceeds at a normal rate Hematopoietic precursors show nuclear-cytoplasmic asynchrony Undergo apoptosis in the marrow (ineffective hematopoiesis) Laboratory diagnosis of MA Blood Hb– reduced Blood film RBC- many oval macrocytes, Anisocytosis, poikilocytosis, Polychromatic & stippled cells, howell-jolly bodies White cells – hypersegmented neutrophils are always present (49 lobes) Megaloblastic blood compared to normal blood hypersegmented neutrophil with a six-lobed nucleus Haematocrit (PCV)– reduced Red cell count – reduced MCV is high, MCH is high, MCHC is normal WBC – leucopenia (neutropenia) Platelets – thrombocytopenia Reticulocyte count – increased 2. Biochemical findings Serum iron & ferritin – increased Serum bilirubin – may be slightly increased in Vit B12 deficiency Lactate dehydrogenase – increased Male Fem 3. Bone marrow Cellularity – Hypercellular (increased numbers of megaloblasts) M:E ratio is reduced or even reversed Erythropoiesis - Megaloblastic erythropoiesis Granulopoiesis is active – giant metamyelocyte with u shaped nucleus Iron in large amount. Sideroblast – increased A to C, Megaloblasts-various stages of differentiation 4. Special tests for vitamin B12 deficiency Serum vitamin B12 assay Schilling test – detects ability of the body to absorb vit B12 after correction. Radioactive cobalt labeled vit B12 is used for the test . A small oral dose is given . Radioactivity in the urine is measured Methylmelonic acid excretion in urine - increased Therapeutic trail - Response to vit B12 administration 5. Special Tests for folate deficiency Serum folate assay Red cell folate assay Theurapeutic trail - Response to folic acid administration Pernicious anemia PA is a vitamin B 12 deficiency megaloblastic anaemia Pathogenesis PA occurs due to failure of secretion of Intrinsic factor by the stomach due to permanent gastric atrophy Vit B12 in food not absorbed (gastrectomy, resection of ileum ) Special tests Pentagastrin fast achlohydria Anti-intrinsic factor & anti-parietal cell antibodies in serum Diagnosis is made by (1) low serum vitamin B12 levels, (2) normal or elevated serum folate levels, (3) serum antibodies to intrinsic factor, (4) moderate to severe megaloblastic anemia, (5) leukopenia with hypersegmented granulocytes, and (6) a dramatic reticulocytic response (within 2-3 days) to parenteral administration of vitamin B12.