22-breaking bad news..
advertisement

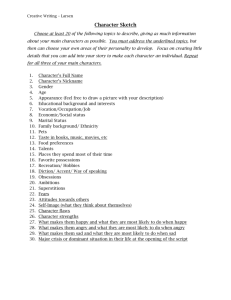
BREAKING BAD NEWS Saleh al-zahrany Rajab al-zahrany Khalaf al-amery Mohareb al-reshedy Abdul-rahman al-serhani Abdul-rahman al-howiti Breaking Bad News Objectives Understand why this is an important part of communication skills. Understand the definition of bad news. The students should become aware of: What to do? How to do it? What not to do? Students should become familiar with certain illnesses/ problems which may require giving bad news. Introduction : By Saleh alzahrani قال رسول هللا:عن أبي يحيى صهيب بن سنان رضي هللا عنه قال :صلى هللا عليه وسلم إن:(( عجبا ألمر المؤمن إن أمره كله له خير وليس ذلك إال للمؤمن وإن أصابته ضراء صبر فكان خيرا،أصابته سراء شكر فكان خيرا له له)) رواه مسلم The Prophet (Peace be upon him) said : “How wonderful is the affair of the believer, for his affairs are all good, and this applies to no one but the believer. If something good happens to him, he is thankful for it and that is good for him. If something bad happens to him, he bears it with patience and that is good for him.” Case Scenario During morning clinic, you receive a phone call from the radiologist at your local hospital. A chest x-ray carried out on Mr. khaled shows features highly suggestive of lung cancer. You remember that Mr. khaled is a 50 year old in your practice area. • From this scenario what is the bad news ? Bad News definition Bad news can mean different things to different people. There have been numerous definitions of bad news including : "any information, which adversely and seriously affects an individuals view of his or her future" Buckman R. (1992) Breaking Bad News: A Guide for Health Care Professionals. Or “any news that drastically and negatively alters the patients view towards future.” Buckman R. BMJ1984 Examples : A patient who is told they are HIV positive. The man who is told his partner has Alzheimer's disease. The patient who is told the lump has been diagnosed as cancer. The couple who are told they cannot have children. Life long illness: Diabetes , epilepsy Why braking bad news is an important part of communication skills ? It is a difficult but fundamentally important task for all health care professionals, yet little formal education & training is offered for this daunting task. Simple Video : http://www.youtube.com/watch?v=Q5Q-isP-JqY References : Prof : Riaz Qureshi presentation . DR:YOUSEF AL TURKI presentation. Department of Health, Social Services and Public Safety , Castle Buildings, Belfast BT4 3SJ Buckman R. (1992) Breaking Bad News: A Guide for Health Care Professionals. Buckman R. BMJ1984 You tube Psychosocial Context Patients response is influenced by previous experiences & current social circumstances--inappropriate timing Even simple diagnosis being incompatible with one’s profession---tremors in cardiac surgeon. Varying needs of patient & family---patients wishes to know more himself & less information to pass on to family, family wishes vice versa. Barriers to effective disclosure It is referred by some physicians like “dropping the bomb” Baile W F, oncologist 2000 common Barriers include Physicians fears of Being blamed by patient Not knowing all the answers Inflicting pain & sufferings Own illness & death Lack of training Lack of time Multiple physician---who should perform the task Patient’s perspective Most important factors for patients include Physician’s competence, honesty & attention The time allowed for question Straightforward & understandable diagnosis The use of clear language Parker PA, Baile WF j.clinical onc 2001 Family's perspective Family members prefer privacy Attitude of person who gave the bad news Clarity of message Competency of physicians Time for questions Jurkovich GJ, et al. J Trauma 200 Delivering Bad News “It is not an isolated skill but a particular form of communication.” Frank A. Eur J of Palliat care 1997 Rabow & Mcphee (West J. Med 1999) described: “Clinician focus often on relieving patients’ bodily pain, less often on their emotional distress & seldom on their suffering.” Delivering Bad News Rabow & Mcphee (West J. Med 1999) synthesized comprehensive model from multiple resources that uses a simple mnemonic of ABCDE Advance Preparation Build a therapeutic environment/relationship Communicate well Deal with patient & family reactions Encourage and validate emotions Advance Preparation Familiarize yourself with the relevant clinical information (investigations, hospital report) arrange for adequate time in private, comfortable environment Instruct staff not to interrupt Be prepared to provide at least basic information about prognosis and treatment options (so do read it up) Advance Preparation Mentally rehearse how you will deliver the news. You may wish to practice out loud, as you would prepare for public speaking. Script specific words & phrases to use or avoid. Be prepared emotionally Build a therapeutic environment/relationship Introduce yourself to everyone present and ask for names & relationships to the patient Summarise where things have got to date, check with patient Discover what has happened since last seen Judge how the patient is feeling/thinking Determine the patient’s preferences for what and how much they want to know Build a therapeutic environment/relationship Warning shot “I’m afraid it looks more serious than we had hoped” Use touch where appropriate Pay attention to verbal & non verbal cues Avoid inappropriate humour or flippant comments Assure patient you will be available Communicate well Speak frankly but compassionately Avoid euphemisms & medical jargon Allow silence & tears; proceed at patient’s pace Have the patient describe his/her understanding of the information given Encourage questions & allow time Write things down & provide written information Conclude each visit with a summary & follow up plan Deal with patient and family reactions Assess & respond to emotional reactions Be aware of cognitive coping (denial, blame, guilt, disbelief, acceptance, intellectualization) Allow for “shut down”, when patient turns off & stops listening Be empathetic; it is appropriate to say “I’m sorry or I don’t know. Crying may be appropriate Don’t argue or criticize colleagues Encourage and validate emotions Offer realistic hope and encouragement about options available Give adequate information to facilitate decision making Explore what the news means to the patient & inquire about spiritual needs Inquire about the support systems they have in place Encourage and validate emotions Attend to your own needs during and following the delivery of bad news (counter-transference: triggering poorly understood but powerful feelings) Use multidisciplinary services to enhance patient care ( hospice) Formal or informal debriefing session with concerned team members may be appropriate to review patient management & their feelings WHAT TO DO? WHAT NOT TO DO? HOW TO DO IT? By Abdul-Rahman Awad Al-Serhani Case Scenario A 73 year old male patient has been admitted via ER with increasing shortness of breath. A chest X-ray confirms a large right sided pleural effusion. A diagnostic and therapeutic tap is performed. The cytology confirms cancerous cells, primary unknown. What and How to do? Preparation Know the personal details of the patient. Have all the information readily available. Determine what the patient already knows. Prepare yourself for what you will say. Have someone else present if necessary - if possible, someone who has had prior contact with patient, or a relative/friend. Assess/ask who they would like to have with them. Appropriate time Look to comfort and privacy Introduction Introduce yourself properly. Spend a few minutes establishing rapport. Ask for information from the recipient to establish their knowledge of the situation. Mistake: Hurry Achieving understanding Speak clearly, other language. using non-medical terminology. Repeat. Regularly check understanding. Mistake: Use medical terminology or unclear language/words. Identify the patient’s main concern. Warn the patient that bad news is coming. Tell them how very sorry you yourself are about what has happened: "I cannot begin to imagine how you may be feeling at the moment." "May I say how very sorry I am about what has happened." Break the Bad News Give information in small chunks Mistakes: Give all the information in one go Give too much information Be blunt. Words can be like loaded pistols/guns Pacing and shared control Try to lead the patient towards making the diagnosis. Let the patient take some of the lead - involve them in the management decisions. Allow for pauses - silences are useful. Do not be afraid of silence or tears. Allow them to ask questions. Responding to emotions Be sensitive Touch the patient/relative if appropriate. Reassure them that is alright for them to cry. Allow expression of emotion. Maintain eye contact and non-verbal communication. Show your own emotion. Offer realistic hope (Honesty) Offer both worst and best scenarios. If appropriate, leave the recipient of the news with some hope. Take responsibility for any mistakes. Do not be afraid to say things like "sorry" and "I don't know" - more useful to be honest if you do not have the full clinical knowledge Mistakes: Lie or be economical with the truth Guess the prognosis (She has got 6 months, may be 7) Support Highlight any positive help eg. pain relief. Offer continuing support/ practical advice. Have a plan for the future - help the patient/relative to plan. Summarize and check understanding (Closure) Summarize at the end of the discussion. Finish with any positive points. Close discussion by inviting questions. Make sure the patient can get home OK. If the patient can’t, make sure that some one is with the patient when he leaves. Set the next meeting and arrange follow up Give a telephone number Things not to say Do not say: "I know how you feel" or "Are you happy with that?" You cannot know how they feel. The words "happy" and death are not compatible. Do not try to finish off anyone's sentences. Let them formulate what they want to say, even if this takes some time. Don't ask them to fill in any forms at this point — e.g. on National Insurance, death certificates etc. Videos http://www.youtube.com/watch?v=Q5Q-isP-JqY http://www.youtube.com/watch?v=Q5Q-isPJqY&feature=related References Prof. Riaz Qurishi presentation. Medical education 1995,29,430-435. Update July 1996 . Breaking bad news – BMJ Jul 2002 Communicating Bad News A guidance Pack dart centre for journalism and trauma Youtube . Angry patient By Abdul-Rahman Al-howiti Angry patient Angry patients and families pose one of the biggest challenges for a clinician Our natural tendency is to respond to anger with more anger, which always makes everything worse. Angry is usually obvious but sometimes you should look for angry signs such as changes in body language, including a tightened jaw, tense posture, clenched fists, fidgeting, and any other significant change from earlier behavior. Angry Patient WHAT TO DO? remain calm and professional Try to calm down the patient Understand the reason of being angry Listen to him carefully Let him ventilate his anger or any feelings that led to his anger Offer to do something or for him to do something Express empathy for the patient Stay curious about the patient's story Find out the specifics of the story--encourage the patient to give the details Angry Patient HOW TO DO IT? Pause and be attentive Sit at the same level as the patient, not too close and not too far, with eye contact Speak calmly without raising your voice Avoid dismissive or threatening body language Encourage the person to speak with open ended questions Empathize as much as you can with verbal and non verbal cues Be aware of your own safety Angry patient WHAT NOT TO DO? Glare at the person Confront him or interrupt him Patronize him or touch him Put the blame on others/seek to exonerate yourself Make unreasonable promises Block his exit If the person is a patient,s relative,be mindful about confidentiality Being defensive