Chapter_10-CV_normal_responses
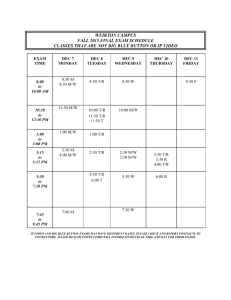
advertisement

CVS Resp to Phys Stresses Heller – 9.28.09 1 of the CVS response to phys stresses should be evaluated in terms of the initial effects primary disturbance and subsequent effects of the reflex compensatory responses. EFFECT OF RESP ACTIVITY -normal sinus arrhythmia = fluctuations in HR due to resp - Δ in intrathoracic P (ITP) due to resp have sig effects on CVS by affecting CO & VR -P falls during inspiration and rises during expiration = Respiratory Pump -inc venous return facilitated by CVP fluctuations due to respirations -transient cyclical changes VR transient changes in CO and PA (see L) - dec in ITP cardiopulmonary barorecp firing reflex adjust to lower PA Para Sympt -CVS effect of resp key in: exercise (deep, rapid breathing inc VR), yawning (dec in ITP inc VR), coughing fit (inc ITP, dec CO faint) -Valsalva Maneuver: bearing down (pooping/lifting), Inc in ITP -during: initial inc in PA, dec VR, Inc HR, peripheral constriction -stop: fall in PA from dec ITP, inc VR inc SV inc CO PA reflexive bradycardia. -dangerous in eldery stroke -Ventilators: positive pressure vents (inflate = inc ITP dec VR; compress pulmonary vessels R vent Afterload. EFFECTS OF GRAVITY Response to Changes in Body Position -Gravity, and hence body position, has a sig effect on the CVS, and various reflex compensatory mech are required to overcome venous pooling that accompanies standing upright. -standing = 90 mmHg P inc in feet (doesn’t change Q cuz equal changed in Art and Vein) Standing: inc venous P and inc art P dec barorecp firing reflexive adjustment of bp by ANS - 2 big effects of standing: 1. inc in venous transmural P distends veins inc in peripheral venous vol 2. inc in capillary transmural hydrostatic P inc filtration rate edema Compensation for standing: -Inc sympt reflex vasoconstriction of arteriole (little effect on cap filtration due to high venous P) -“skeletal musc pump”: musc contraction expels venous bld and lymph, valve prevent backflow post-contraction. lower venous pressure and dec cap filtration. -short term cardio compensation never completely correct the initial disturbance (SV and CO dec standing even though we are trying to inc them) -MAP inc from laying standing (odd cuz sympt are high) due to: 1. arterial barorecp rate dec despite small inc in MAP IF PP is large 2. MAP estimated from blood pressure cuff on arm overestimates MAP sensed by barorecp in carotid due to gravity. 3. influences on medullary cardivasc centers from cardiopulmonary recp is interpreted as dec in blood vol and may inc PA. -Every reflex alt in Sympt has effect on kidney and fluid balance (long-term) -Standing inc Sympt fluid retention in bld Vol dec mag of reflex alt standing Response to long-term Bed Rest (or Zero-Gravity) Long term bed rest causes dec in circ bld vol that contribute to othrostatic hypotension -immediate: fluid shift from lower upper extremity (face edema, inc leg vol, nasal stuffiness, etc) -inc central bld vol stim cardiopulmonary mechanorecp renal func by neural/horm/dec sympt promote fluid loss. -Pt loses weight, hypovolemic in a few days. -standing fainting cuz lower bld circ vol exaggerated above issues. (orthostatic hypotension) -limited Tx but sitting up, lower legs, salt and water loading. EFFECTS OF EXERCISE Resp to Acute Exercise -Specific Alt in CV func depend on: exercise type (isotonic/isometric), intensity/duration, age & fitness level 1° CV disturbances of exercise (central command & musc vasodialation) evoke immediate reflex compensatory activity, which permits major changes in musc bld flow and CO -Central command is a set-pt-raising influence in medullary CV centers higher MAP -info from chemo/mechanorecp in skeletal musc influence MAP set-pt too -Metabolic vasodialator accumulation Musc vasodialation Dec TPR triggers sympt through strong arterial barorecp reflex. -Although MAP is high, TPR causes it to fall arterial barorecp reflex inc sympt (odd cuz PA is already higher than normal, w/o it MAP would fall below normal) EFFECTS OF EXERCISE CONT. -Thermal reflexes: inc Q to skin cuz thermal reflex overrides sympt vasoconstriction vasodialation, dec heat CVS Resp to Phys Stresses -Coronary bld flow inc during exercise due to local metabolic vasodialators. 2 Heller – 9.28.09 - isotonic (dynamic) exercise --2 key CV mech of response to it: 1. Skeletal musc pump: VR = CO, maintains CVP 2. Resp pump: promote VR, deep breathing inc effectiveness during exercise -Central venous pressure doesn’t change cuz VR = CO (both curves shift up) -large inc in skeletal musc blood flow due to inc CO and dec bld flow to kidneys and splanchnic organs -recovery: norm bld flow within mins, active hyperemia -training: vent chamber enlargement -Isometric (static/weight lifting) exercise: -TPR: same or falls due to musc compressing vessels as they contract -1 °dist: set-pt-raising from chemo/mechanorecp in contracting musc – “exercise pressor response” -CV effects: inc HR, CO, PA from inc sympt, but less of HR and CO inc than isotonic -more inc Diastolic, systolic, MAP due to higher afterload – cardiac work is higher -recovery: bld flow rises normal due to reactive hyperemia. -training: inc myocardial mass and vent wall thickness Response to Chronic Exercise: Chronic exercise (training) evokes compensatory adjustments in CV chara and musc metabolic process, permitting greater exercise effiency. -training inc circ bld vol, dec HR, inc SV, dec PA at rest -during exercise: achieve CO with lower HR and higher SV dec heart oxygen demands, inc cardiac reserve (pot for inc CO) -heart changes: vent chamber enlargement w/isotonic; inc myocardial mass and vent wall thickness w/isometric AGE DEPENDENT CV CHANGES: Pregnancy: Placenta: low resistance in parallel w/other organs dec TPR of system. Pa = CO x TPR (mean arterial pressure may fall early in preg) -huge inc in circ blood vol!!! Allows for inc SV will over come the fall in TPR and maintain CO and bp where it should be. Fetal Circ & Changes at Birth: Fetus: -placenta: site of exchange of nutrients, gases, waste; low R, high Q -lungs: no Q due to high R -heart: R & L vent work in parallel, fill in unison via foramen ovale -bypass pulmonary art via ductus arteriosis Birth: -dec pulmonary R with ventilation inc Q to lungs! -inc TPR w/loss of placenta -inc aortic pressure dec Q ductus arteriosis (closes) -all these changes inc L heart afterload inc L atrium P, dec R heart P close foramen ovale valve. Pediatrics CV Chara: - neonate: high HR, low bp dec until reach adult level in teens -Pulmonary vasc R dec during first year due to vessel remodeling -L vent hypertrophy from inc afterload over time (switch from R vent dominate L vent dominate on EKG) -innocent heart murmurs from rapid filling and ejection CV changes w/normal aging: Age results in a dec in maximal capabilities of CV responses that are distinct from any disease process. -slower, stiffer and drier w/age -Age dept heart changes: 1. Dec cardiac index 2. Dec max HR 3. Inc in contraction, relaxation time of heart musc 4. Inc myocardial stiffness during diastole 5. Dec # func myocyte 6. Accumulation of pigment in myocardial cells -vascular changes: dec cap density, dec art compliance, inc TPR inc MAP and Pulse Pressure -arterial barorecp induced responses to changes in bp are blunted age-dept sluggishness in res to posture/exercise changes afferents: dec barorecp activity, inc art stiffness efferents: dec NE sympt nerve endings, dec myocardial response to catecholamines Age changes are different from disease processes (Atherosclerosis, hypertension common in elderly – not universal to aging) Effect of Gender: -Gender influences several CV charac & disease susceptibility particularly before the age of menopause in women -Pre-menopausal women: estrogen is protective (lower L vent mass, lower afterload, lower bp, inc arterial compliance, better vasodialation. -post-menopausal women = men -electrical dif: women have lower HR, longer QT intervals (inc risk for long –QT, Torsades) CVS Resp to Phys Stresses Heller – 9.28.09 Study Q: 1. Average central venous pressure _________ with isotonic exercise compared to resting. A. Increases B. Decreases C. No change 2. Many of the effects of exercise training are due to: A. inc bld vol B. reactive hyperemia C. inc # cardiac musc cells 3. Which of the following are important pumps in the body: A. Resp pump B. Skeletal musc pump C. Heart D. All of the above 4. Increase in peripheral venous volume and edema are 2 big effects of: A. bed rest B. Standing C. placenta D. Vasovagal hypotension 5. Normal cardiovascular age changes include all of the following EXCEPT: A. dec HR until teen yrs B. dec pulmonary resistance C. R vent hypertrophy D. Arteriosclerosis Answers: 1. C, No change 2. A, inc blood vol 3. D, all of the above (know how and in what situations the resp and skeletal musc pump work) 4. B, Standing 5. C, R vent hypertrophy – the L vent hypertrophies due to greater afterload 3