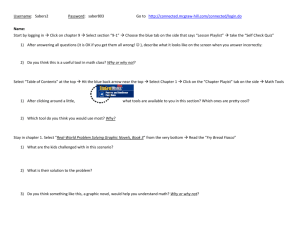
Philippine General Hospital University of the Philippines Manila The
advertisement

DFCM Cell Phone: 09052642659/ 09228943434 Local Number: 2521 Hospice: 09276542185/09228943332 GP in: Michelle ACR: Alex SASOD: Ruby AMBU AM: annie PM: Grace Pay Endorsement: 1. Complete admitting papers 2. CUT OFF BATCH 2014: 4PM 3. Philhealth CF3 Philippine General Hospital University of the Philippines Manila The Health Sciences Center Taft Avenue, Manila Department of Family and Community Medicine Pay Ward Daily Patient Census March 30-31, 2014 Rm # 702 700 568-5 568-4 553 552-2 552-1 454-1 436-2 406-2 CENICU 12 Dengue I (DF & DHF 1&II) 8k Dengue II (DHF III&IV) 16k Pneumonia I (MR) 15k Pneumonia II (HR) 32k Essential Hypertension 9k Cerebral Infarct (CVA I) 28k Cerebrovascular Accident (CVA II) 38k AGE 6k Asthma 9k Typhoid Fever 14k Newborn care package in hospital and lying in 1750 Dr. Tordesillas’ Clinic/Jesicca:: 524-0264 Rm 303 UDL Bldg. Taft Ave. (Sharmaine) UPHS Mon PM (708-0000 loc 160) FMAB schedule W-Th-Sat 1-4pm (Ava) Philhealth# 1201-98122464 TIN # 141-719-845 Dr. Ang’s Clinic: 310 West-East Center, Taft Avenue (beside KFC) 5281330 MW 9-4 F 1-4 FMAB T-Th 1-4pm; F 9-12 am Philhealth #: 1201-0600628-6 Dr. Nicodemus’ Clinic: 310 West-East Center, T aft Ave (beside KFC) 5281330 UPHSMon AM Philhealth# 1201-0817470-0 Dr. Josefina Isidro Philhealth #: 1201-9501621-0 UPHS Thurs PM Dr. A.JB. Alip, Jr. Philhealth #: 1201-9803950-0 Dr. Agnes Bausa-Claudio Philhealth #: 1100-05010606 Dr. Doris Camagay Philhealth #: 1201-9900024-5 Dr. Anna GuiaLimpoco PhilHealth #: 1201-1225191-3 Dr. Karin Estepa-Garcia Philhealth #: 1201-1121439-4 Dr. Pumanes (St. Paul) 5245687 loc 226 PhilHealth #: 1501-980-8329-5 DOH Hotline 711-1001 to 02 PNRC: 5270000 loc 0861 ASIAN Hospital: 771-9000 Makati Med: 888-8999 Manila Doctor’s Hospital: 5243011 Patient Casing, Bonifacio Fernandez, Karen Angela Guiron Rolando Terrenal, Romeo Lachica Benjamin Escalderon Danilo Magno, Joeriz Bandalan, Michael Shann Pedraja, Gilda Dimaculangan, Josefina Matias, Cristeta REFERRALS Serra, Ignacio Lachica, Benjamin CO-MANAGEMENT Rola, Eliezer CI Ronquillo, Milagros Reyes, Remedios TRANSFERRED DISCHARGED Manuta Buena Arriesgado, Premitiva MORTALITY 745 553 568-2 CI Bed 28 39 CI Bed 27 W2B28 606-2 416-6 Total no of patients 16 CENICU Received 18 Primary 11 Discharged/TOS/HAA/HPR 2/0/0/0 Consultant Limpoco Tordesillas Garcia Ang Ang Tordesillas Tordesillas Limpoco Tordesillas Ang Tordesillas Ang Ang Bausa Sianghio Sianghio Tordesillas Limpoco 1 Transfer 1 Admission 0 New referral 0 Co-Managed/Referral ½ Hospice (CI) 2 Mortality 0 Employees 5 LCB 401-404: 3494 LCB 405-409: 3494 (524-9849) LCB 410-412: 3492 LCB 413-418: 3492 521-9534 LCB 419-426: 3496 RCB 427-433: 3496 RCB 433-439: 3496 (523-3888)/3497 RCB 440-451: 3498 (447- 4504)/3499 452-500 3498 LCB 501-512: 3592 LCB 513-518: 3593 (526-0065) LCB 519-536: 3594 RCB 537-553 3596/3597 RCB 554-565 3598 RCB 566-569 3599 RCB 601-644: 3696/3697/3698 RCB 645-649: 3696 RCB 650-659: 3698 (522-1801) RCB 658-665: 3699 LCB700-713: 3792(522-2002) LCB714-732: 3792 RCB733-763: 3796 (09154993391) PGH TRUNKLINE: 554-8400 ACU: 2511/2517/2508 Admitting Section: 2067/ 567-3116 Ambu: 2514 Blood Bank: 3214 CENICU: 3252 CI: 4203 Chairman’s Ofc: 2522/2523 Col Public Health 525-5874 CT scan 3118 ECG: 3154 FMAB 7080000 FMC 5110 Lab Info/Hema 3209/3213 MRL: 3233 PACU: 3328 Radiology Info: 3106 UPHS: 2077 /2076 SHPM: 5302 TOX: 2311 2D Echo 3610 Billing: 2015/3132 Info: 2012 EHRO: 2064 702 CN 3526692 CASING, BONIFACIO 86/M 3/14: Michelle Dr. Limpoco/Dr.Anonuevo(CVS)Dr.Santiguel (Pulmo)/Dr. Ong (GI) CAP, LR Hypertension Hand Tremors prob sec Parkinsons with depression vs. MDD DOA right knee CVS: CHF FC III sec to IHD, HHD Consider chronic lung disease(COPD, PTB w/ restrictive lung component) Chronic AF w/ RVR Pulmo: Pneumonia in the elderly COPD suspect PTB GI: UGIB sec to 1. BPUD 2. ASA/warfarin induced 3. SRMI Pneumonia in the elderly Cor pulmonale Chronic AF from ischemic heart disease CC: DOB IVF: PNSS 1l x 16h HPI: 5 days PTA—(+) DOB, associated with cough productive of yellowish phlegm, no fever, no chest pain noted. 4days PTA—consulted a private MD where labs and CXR were done. CXR showed pneumonia, patient was given unrecalled antbiotics and was advised admission. 1 day PTA—seen by Dr. Limpoco at FMAB—advised admission Diet: low salt, low fat diet, 1 glass Nutren everyday Sputum GSCS Enterobacter cloacaecplx: S> Meropenem </=0.25, Imipenem 0.5 Candida guillermondii: S> Voriconazole </=0.12, Fluconazole </=1, Amphotericin B 0.5 Antibiotics: Meds: NAC 600mg tab BID Digoxin 0.25mg tab, 1 tab OD Aspirin 80mg tab, 1 tab OD pc Salbu + ipra neb q 12 Celecoxib 200 mg cap OD Omep 40 IV q 12 Furosemide 40mg/IV post BT Colchicine .5mg BID ---500mcg BID Atorvastatin 40mg ODHS Salmeterol+Fluticasone 250/25 1 puff BID Ketoprofen gel BID Discontinued: Cefuroxime 750mg IV q8 D3+2 Azithromycitidn 500mg tab OD x 5 days D3 Pip Tazo 4.5g IV q8 NAC 200mg TID Losartan 50mg tab, 1tab OD Hold Carvedilol 6.25mg tab, ½ tab OD- Hold Coumadin 1 mg/tab OD Hold Folic acid + Ferrous Sulfate tab- HOLD Voricozole 50mg/cap I cap BID D0+1 Meropenem 1 gm q8 D10 D/c Omeprazole drip CBC: 3/30: 115, 0.386/8.27/0.79/0.13/174 3/27: 63/0.203/7.772/209 3/25: 96/0.308/7.14/176/ S 7.14/L 0.18 3/23 144/0.457/6.93/0.76/0.17/0.05/0.02/193 3/20: 134/0.435/8.86/0.83/161 128/0.391/6.69/0.86/0.08/242 For EGD tom 7am s/p 3u PRBc (+) knee pain, (-) BM x 2 days Post BT CBC On nasal canula, comfortable Blood Chem: 3/30 Uric Acid 0.29 Na 138 k 4.5 Cl 101 BUN 9.4 Crea 136 3/18 chole 158/TG 108/HDL 32/LDL 104/FBS 92/BUN 30.62/crea 1.24/Na 142/K 3.8 ECG: AF in RVR, RAD, LPHB, CRBBB, RVH, LVH, old septal wall infarct Still with knee pain fundoscopy Cataract bilateral with optic disc sweeling. Cant sppreciate other fidings Still for otoscopy CXR: official:multichanbered cardiomegaly, likely to be secondary to mitral valve pathology w/ pulmonary hypertension, consider minimal pleural effusion, left vs pleural reaction Urinalysis 3/18 yellow,clear pH 5.5, 1.027, gluc(-),alb(tr), RBC 0, PC 0 PT/PTT 3/30: 13.3/28.6/29%/2.61/30/44.1 3/25 PT 13.30/PT 27.7/% 30/INR 231 3/22: 13.3/17/62/1.36/29/35.8 3/18 : PT 13.3/15.7/72/1.24 PTT 29/79 Sputum AFB Negative Sputum GS PMN > 100 Sq EC >100 Yc>25 Gram (-) bacilli >25 Gram (+) bacilli 2-10 Chest UTZ: 3/20:Left: Minimal pleural effusion, (-) safe window (-) isoechoic complex over left hemidiaphragm (consolidation vs mass); Right: well aerated lung (+) Depression symptoms more than 5 based on the depression scale FF up: Official CXR (repeat) 2D echo Aortic stenosis, mild to moderate with moderate aortic regurgitation. Concentric left ventricular with segmental wall motion abnormality and mildly depressed global systolic function. Increased right ventricular dimension with decreased contractility and evidence of volume overload. EF 50% Continuing with possible C0r Pulmonale w CAD 700 CN 4018246 FERNANDEZ, KAREN ANGELA 24/F CC: fever IVF: PNSS 1L x 8hrs --- D5NM 1L x 8hrs HPI: 5 days PTA—(+) fevr associated with headache. No abdominal pain, bleeding episodes noted. 1 day PTA—consulted at FMAB, CBC done showed low platelet hence advised admission DAT Meds: Paracetamol 500mg tab prn for fever t/s Ceftriaxone 1g OD ABG 3/29 7.454/46.4/81.6/32.3/8.696.2/34.2/32.3 3/25 7.491/49.3/102/38.5//13.7/98 3/19: 7.356/50.2/62.2/28.3/90.4 CBC: 3/30: 126, 0.395, 4.1, 0.54, 0.29, 0.15, 107 3/29 130. 0.397, 2.97, 0.64, 0.29, 108 129/0.378/115/3.24/0.57/0.34 Salmonella IgG and IgM: Non reactive Dengue titers IgG reactive, IgM non reactive 3/28: Michelle 48/M Dr. Garcia/Janus Ong (GI) 3/29 Alex PEG replacement HIE sec to CP arrest s/p tracheostomy S/p PEG HPN For: Repeat Salmonella Titer Repeat CBC today pm (3/31) Ff up Blood CSx2 Dengue Fever GURION, ROLANDO No bleeding episodes Blood Chem Na 135/K 3.6 Dr. Tordesillas 568-5 CN 388066 (+) fever episodes 38-40 CXR Normal Known case of HIE sec to CP arrest S/p Tracheostomy S/P PEG HPN 3 days PTA, peg was removed 2 days PTA, patient was advised PEG replacement, TPN was started IVF : D5NM 1lX 8 hours U/a Yellow clear, blood +2, RBC 2, WBC 1, Bacteria 10, MT 3 CBC 128/.399/6.91/306/0.68 Diet: None for now, On TPN Meds: NAC 100mg/ml Duovent neb now then 2x a day Baclofen 20mg/tab Carvedilol 6.25mg ½ tab once a day Clopidogrel 75mg/tan OD Senokot forte ODS Calmoseptine aplle 2x a day Dulcolax suppository Tranexamic Acid tab q8 PT/PTT 13.30/14.3/ % 85 INR 1.1/APTT 30/ PTT 30 Awaiting dietary input Awaiting Anes clearance prior to discharge Once with PEG to start paracetamol 300mg /iv before procedure then Paracetamol 300mgIV after procedure Cbg: 126, 127, 165 568-4 CN 4018251 TERRENAL, ROMEO 53/M 3/28: Michelle Dr. Ang/Dr. Lopez (GS3)/Dr. Sandoval (Endo) Acalcoulous cholecystitis `DM type 2 CC: RUQ pain IVF: PNSS 1L + 40meqs Kcl x 8hrs for 4 cycles HPI: 5 days PTA – (+) RUQ pain 10/10, no fever, no jaundice, no vomiting. 3 days PTA – admitted to a private hospital. On UTZ (+) acalculous cholecystitis, advised operation. However decided to transfer to PGH. Meds: Pip-Taz 4.5g IV q8 Demerol 2gmg IV q6 Omeprazole 40mg tab OD Tramadol 50mg IV RTC x 24 hours Paracetamol 600mgIVx1 dose Buscopan 10mg IV q8 Glargine 14u q 24 --- 16 u q 24 Ca+Vit D OD 10% Oral KCl soln 30cc q 8h Regular insulin 4 u TID pre meals Cholangitis S/P Cholecystectomy AKI on top of CKD sec to DM KD Labs done outside: Attached to chart CBC 157/.530/13.27/187/0.66/.28 On going K correction (+) improvement of upper extremities weakness (-) febrile episode s/p Choleccystomy Blood Chem 3/30: Na 148, K 2.0, Ca 1.90, Albumin 19, ALT 191, Crea 136 Hbaic 13.7/TB 67.3/DV 31.7/IB 35.6/BUN 11.6/Crea 118H/AsT 224/ALT 471/Alk Phosp 613/Amylase 244/Na 136/K 3.4 HA UTZ (c/o GS) Emphyema GB with 0.9 cm hyperechoic foci with definitive PSS GB dilated CBD non dilated Ff up: UA CBG q 12 and HS 3/29 4-235, 8-303, 12-223 3/30/14 12- 173, 4 295 Monitor JP1 and JP2 CBG monitoring 173, 245, 285, 256, 272, 172 t/c Emphyema GB with acute cholecystitis ABG: 7.364, 22.7, 95.5, 13.1, 9.7, 97.4 CXR Bilateral TB infiltrates Cranial CT Scan: initial unremarkable CT, no bleed, no shift, polysinusitis 553 CN 4018197 Know case of PTB treated last 1993 IVF: PNSS x 16h consume then shift to D5NM x 16 h Diet: DAT LACHICA, BENJAMIN 56/m 3/26 ALEX Dr. Ang Pulmo mass prob malignancy PTB r/o reactivation Anemia of Chronic Disease Pneumonia in ICH Tinea faciae HPI: Oct 2012 patient started to have hemoptysis with cough productive with dyspnea 2013, cough, dyspnea with productive, wieght loss and decrease appeptite CXr and CT scan was done and right pulmo mass 7x9x7cm w/ lymphadenopathy Meds: Pip-Tazo 4.5g IV q8 D5 Sincod forte TID Tramadol + Paracetamol 37.5/325 q 6 RTC --- Tramadol 100mg tab q6 RTC MV + Iron OD Buclizine Fluconazole 200mg OD x 2 weeks Nystatin oral solution TID x 5 days Lactulose ---HOLD Dexamethasone 4mg tab OD Omeprazole 20mg OD ECG 3/31: NSSTTWC can not rule out ischemia Post op: NSSTTWC RSR NPSSTWC CBC: 3/29 105/0.349/651/30.19/0.89 80/0.30/26.40/812/ PT/PTT PT 13, 15 % 73, 1.22 APTT 29/35 Blood Type: B+ Blood Chem 3/29: K 4.8 3/26: Na 130, K 3.2, Cl 95, RBS 100, BUN 6.18, Crea 0.45, Alb 17, Ca 2.47, Mg 0.79 AST 27, ALT 8, ALK phop 92. s/p BT 2u PRBC Referred to Hospice for palliative care Bedsore precaution Discontinued: Levofloxacin 500mg/tab OD 552-2 CN ESCALDERON DANILLO 35/M Dr. Tordesillas/Dr. Hernandez(ORL) 3/30 Alex Multiple injury sec VA Right zygomatic arch and latertal orbitals fracutres Impacted Cerumen, AS CC: VA IVF: PNSS 1l x16h MOI: hit by a car and was drag TOI: 11:45pm DOI: March 21 Place: South wood DAT Admitted at laguna unconsicous, work-up was done and revealed fractures at facial area. Patient had episodes of epitaxis and nasal congestion hence admission Meds Celexocib 200mg/tab BID Tramadol 50mg/tab q8 Na docusate 3 drops AU TID Urinalysis: Straw/clear/glucose trace/blood +1/6.5/1.003/RBC 0/ WBC 4 CBC: 3/30: 129, 0.406, 9.16, 0.66, 0.24, 412 (-) chest pain Urinalysis 3/30: yellow clear, alb normal, glu (-), pH 5.0, SpGr 1.021, RBC 0, WBC 0, EC 0, Bact 44, MT 440 Blood Chem` 3/30: Na 136, K 3.9, Cl 103, BUN 4.6, Crea 75, BUA 0.25, AST 30, ALT 42, Alk Phos 111, Alb 30, Ca 2.33, P 1.44, Mg 0.89 T-Cage: Bone island vs pulmo nodule 5th posterior rib left ECG: RSR, NA, NSSTTWC 527 CN 4018279 NARAG, JIMMY 56/M 3/31: Michelle Dr. Tordesillas/Dr. Lopez (GS III)/Dr. Sandoval (Endo) Calculous Cholecystitis Complicated UTI t/c DM type 2 with nephropathy HTN St. II 552-1 CN 4018085 MAGNO, JOERIZ 37/M 3/25: Jen Dr. Tordesillas/Dr. Grosman(Ortho CC: RUQ pain Cleared by Endo For OR tom HPI: 3 mos history of intermittent RUQ oain. 1 week PTA – RUQ pain severe, no fever, no jaundice, no vomiting. HBT UTZ done showed distended GB with cholecystitis. Advised operation. Referred to Philcare coordinator, Dr. Tordesillas Cc: leg pain both IVF: Heplock 5 month PTA, patient with leg pain, both, on and off, NPS 5/10 not aggravated by activity relieved by massage with tinglng sensation and no limitation of movt no consult and self med with unrecalled med Diet: DM diet Meds: Metformin 500mg tab BID Pregabalin 75mg tab OD HS BID Celecoxib 200mg tab BID prn Sitagliptin 50mg/tab once a day CBC ??/0.437/9.53/0.68/276 U/A Yellow orange/clear/6.0/1.031/+2 glu/+1 blood/RBC 0/WBC 0/bact 189/ CaOx 4/MT 686 Blood CHem Na 138 K 3.4 Cl 102 Chole 5.33 Trigly 1.17 HDL (+) leg pain 5/10 For rehab referral c/ Dr Mojica for conservative managemtn Spine) Peripheral Neuropathy secondary to DM neuropathy DM type 2 NIR,NO 1 month PTA, increase frequency and severity of bilateral leg pin, on and off, NPS 10/10 with same characteristic still with tingling sensation no weakness no limitation of movt hence consult Tramadol IV PRN Discontinued: Gliclazide 80 mg tab OD 1.40 LDL 3.4 FBS 11.7 BUN 5.4 Crea 58 AST 15 ALT 25 alb 40 uric acid 0.20 Ca 2.33 Mg 0.77 HBA1c 10.6 Ortho: Neurogenic claudication sec to narrowed spaces L5-S1 CXR: normal LS xray: retrolisthesis S1 over L5, degenerative osseous changes L5 radiculopathybsec to HNP ECG: normal MRI: L5S1 HNP central causing mild to moderate central foraminal stenosis 454-1 CN 4018253 BANDALAN, MICHAEL SHANN 2/M 3/28: Michelle Dr.Limpoco/Dr. Cu (Pedia) AGE UTI CC: fever IVF: D5LR 1L x 100cc/hr (FM + 30%) decrease to 70cc CBC 3/29: 124/0.358.4.59.267.N .59/K .29/M .10 (-) febrile episodes (+) coughing and bloatedness (+) BM formed HPI: 5 days PTA—fever Tmax 39.0C associated with cough, colds and sore throat. Consulted a private hospital, given Natravox and Paracetamol. 4 days PTA—noted LBM after intake of NAtravox. Consulted a private pediatrician, given Metronidazole. 3 days PTA—still with LBM consulted again a private hospital however not admiited. 2 days PTA—noted vomiting and dysuria, persistence prompted consult and admission DAT Antibiotic:: Ceftriaxone 100 950mgIV q12 D1+2 Blood Chem 3/30: Na 136, K 4.2, Cl 102, BUN 2.1, Crea 50, Ca 2.37 Meds: PAracetamol Simeticone 40mg/chew tab now Salmonella titers igG reactive igM reactive FFup Blood CS x 1 site Stool CS Urine /CS CXR Fecalysis: Brown, soft/mucoid RBC 0-2, WBC 2-5 NOPS, Fat Globule 1+ Urinalysis: Yellow, cloudy, 6.5, blood +3, glucose normal, albumin trace, RBC 2, WBC 2, Bact 25, MT 30 Urine GS PMN 0-1, gram + cocci in pairs 436-2 4018136 PEDRAJA, GILDA 41/F 3/23: Arvie Dr. Tordesillas/Del Rosario (gyne)/Dr. Cc: hypogastric pain IVF: PNSS 1L x 12h 2 month history recurrent UTI by UA, hypogastric pain radiating to back 8/10, no vaginal discharge, (+) dysuria, (-) hematuria, (-) oliguria, (-) fever, (-) LBM. Given courses of Ciprofloxacin and Unasyn with no relief. Noted retroverted uterus Antibiotic: Ciprofloxacin 500mg tab 1 tab BID x 7 days D1 Medications: HNBB 20mg IV q 8h PRN Celecoxib 200mg BID - HOLD Tramadol 50mg IV prn Blood GS: (+) for G(+) cocci in pairs after 1536hrs of incubation CBC 3/23 129/0.415/9.59/0.66/0.25/0.06/0.02/0.01/420 Blood chem. 3/23 Na 139/K 4.2/Cl 107/Chole 213/TG 98/HDL 37/LDL 157/FBS 98/BUN 11.80/crea 0.55/BUA 5.42/AST 26/ALT 29/alb 3.80/Ca 9.20/PO4 3.66/Mg 2.19 No hypograstic pain MGH Uro and OB wise Whole abd UTz: 3/24: Mild Fatty liver, Cholecystolithiasis Lapitan(Uro) UTI Myoma Uteri Obese I and myoma uteri on UTS and CT. persistence of symptoms hence admission. Discontinued: Ceftriaxone 1g IV OD D3 Urinalysis 3/23 yellow, clear pH 5.0, sg 1.022,gluc(-),alb(),RC 2,WBC 19 Urine GS: PMN 0-1 Gram (+) bacilli 2-6 Gram (+) cocci 4-6 406-2 CN 4018180 DIMACULANGAN, JOSEFINA 53/F Cc: stroke with right residual IVF: PNSS x KVO 24 days PTA, patient with sudden weakness of the right side of the body and sought consult at Calamba Doctors with BP 240/120 and Dx with CVD bleed and manage with unknown medication Diet:OF feeding 1800 kcal Dr. Ang/ Anlacan (neuro) 3/24: Jen CVD bleed with right residual HAP HPN stage 2 uncontrolled Neuro: s/p ICH, L BG ~__ cc (3/1/14) t/c HAP HTN st II Neuro: CVA bleed L putamen 2 days PTA, patient was discharge with right sided residual, unable to ambulate and unable to talk with home meds of cataprres, atenolol, cefixine, flumucil and salbu neb with unknown dosage and days of treatment hence consult for opinion and management Antibiotics: Piper-Tazo 4.5 gm TIV q 8 D6 Meds: Flumucil NAC 600 ODHS Salbu +ipra neb q 8 to consume stock Paracetamol 300mg TIV q 4 prn Paracetamol 500mg tab q 4 prn Mannitol 50cc q 4h --- q6 Donepezil 5mg ½ tab OD Captopril 25mg ½ tab OD PRN BP 160/100 Salb + Ipra neb q 8h Carvedilol 6.25 mg tab BID Fusidin ointment on bed sore q8 Telmisartan 80mg/tab Amlodipine 5mg/tan --- 10mg OD Omeprazole 40mg IV q 12h Piracetam 1.2g TID Discontinued: Losartan 50mg tab OD BID D/c Transrectal UTZ 3/24: normal sized uterus with small myoma uteri intramural with subserous component, normal ovaries with dominant follicle, right Proliferative phase endometrium Urine Culture E.Coli S ceftriaxone CT scan: Myoma uteri Right adexal cystic foci, likely ovarian in origin Renal cyst L Bosniak CBC 135/0.40/12.3/463 (-) coffee ground material per NGT For referral to Rehab/Dr.nacio once cleared by neuro BP range 140-160/90-200 U/A Yellow, turbid, RBC 150/WBC 200/ EC 1/Bacteria 500 Blood CHem Na 138 K 4.6 Cl 101 BUN 7.7 Crea 47 uric acid 0.27 AST 35 ALT 29 alb 30 Ca 2.55 Mg 1.01 Choles 4.14 Trigly 1.28 HDL 0.96 LDL 2.60 FBS 6.2 FT4: 18.5 TSH 1.5 CXR Normal fiding ECG Sinus tachycardia, NSSTTWC PT/PTT 13/13/99/1/29/26.7 Cranial CT scan CVA bleed L putamen 2D echo EF 72% Concentric remodelling of the left ventricle with good wall motion and contractility and preserved overall systolic function Ff up official CXR (+) crackle L lower, decreased BS R Refer to rehab c/o Dr.Ignacio if ok with neuro once BP stable Dr. Anlacan OOT(528-30), Dr.Astejada to cover For: FOBT FF.up: Repeat CBC CENICU 12 CN 4017812 MATIAS, CRISTETA 65/F 3/7: Michelle Dr. Tordesillas/ Dr. Pasco (neuro)/Dr.Dimacali(renal)/ Reyes (CVS)/Dr.Satiaguel (pulmo) Admitting Impresion: Encephalopathy pob. 1. Metabolic 2. Septic CAP, MR r/o CVD HTN DM Neuro: Encephalopathy 1. Metabolic AKI prob sec to poor intake on top of chronic disease secondary to hypertensive/ diabetic nephropathy CVS: Encephalopathy resolving proib metabolic AKI on top of CKI 2 HPN HPN DM 2 BANIAE Anemia, multifactorial 1 nutritional, 2 chronic disease t/c atrophy of disuse Pulmo: ARF sec to CAP with aspiration component BANIAE cannot rule out PulmoEmbo AKI on top of CKD sec to HTN/DM nephropathy HTN DM CC; decrease sensorium Patient known hypertensive, diabetic, and asthmatic HPI: sudden onset of decrease sensorium, described as difficulty to ariuse and no verbal output. Phone order fro Family friend MD – hook to LR. 3 hrs PTA noted CBG to be low 63. Advised to shift IVF to D5W, however no improvement, hence consult. IVF: Diet: OF via NGT 1600 kcal in 6 equal feedingsAntibiotics: Meropenem 1g IV q 12h Piptazo 2.25g IV q 8H (D2) Azithromycin 500mg (D3) Meds: Salb neb q6 Insulin Aspart 14 u PB, 8u PL 8u PD - HOLD Imdur 30mg Clopidogrel 75mg Vastarel 35 mg Amlodipine 5mg Paracetamol 500mg/tab q6 RTC Salbutamol neb q 4h Citicholine 1g q12 NAC ASA 80mg OD Enoxaparin 0.4cc SC OD Omeprazole ?? Furosemide IV 60mg due to decreas output CBC: 3/30: 98/0.333/9.33/0.89/0.07/372 3/24: 100/0.328/12.8/0.89/0.08/204 3/10: 99/0.332/15.92/274 3/8: 99/0.330/9.85/0.86/0.09/290 Blood Chem: 3/19: K 3.0 3/16 Crea 310, K 4.2 3/14 Mg 1.13, K 7.9- 5.6 3/13: Na 140 K 2.9 Cl 112 Crea 299 Ca 1.85 Mg ).59 3/10: Na 143 K 5.4 Cl 116 Crea 283 alb 24 Ca (2.36) Mg ).83 3/9: Chole 4.34 Trig 0.93 HDL 1.65 LDL 2.27 FBS 4.2 Crea 257 K 2.8 CO2 28,7 Hba1c 8.5 3/8: Na 149,K 3.8 Cl 112 BUN 21.3 Crea 309 AST 35 ALT 19 alb 28 Ca 2.32 Mg 1.05 Urine chem. 3/23 Na 22.09/K 18.88/Cl 26.71/crea 133.48/TP 536/TV470 HBA1c: 8.5 Discontinued Inotropes: Dopamine 2 amps in 250 D5W x 22cc/hr Unasyn 750mg IV q8 (D1+2) MgSO4 3g in 250 D5W x 24 hrs d/c Pip tazo D10 Dobutamine 2 amps in 250 D5W x 18 cc/hr – OFF Norepinephrine 2 amps in 250 D5W x 16 cc/hr - OFF Oral KCl 20cc TID x 4doses ABG: 3/30 b: 7.513/32.2/57.2/26.2/4.2/92.2 3/30 a: 7.518/35.8/186.4/29.4/6.9/99.7 7.402/34.5/155.2/21.6/99.3 PT: 13.30/12.6/112/0.94 PTT: 29/23.5 CXR Provisional – pneumonia, R, bilat pleural effusion L>R, cannot rule out congestive changes Chest UTZ: Right: Hypoechoic ICJ 290ml Left Hypoechoic area ICJ 140ml 2d echo Provisional: 37% EF, wth moderate wall hypokinesia Re-intubated (desat 88-89%, dyspnea tachypnea) s/p BT 1u PRBC? s/p intubation s/p arrest 11 minutes (+) watery stools, total of 10x since feeding was resumed, non-bloody, no fever Latest VS 110/80 80 20 afebrile CBG while OFF feeding 180/ 113/115 DNR status FF up: ETA GS/CS Repeat CBC Sputum GS/CS Sputum AFB Blood CS CBG 3/14: 104 3/13: 118/113 3/12: 67/118/87/109/ 100/142/113/105 3/11: 269/240 3/10: 122 3/9: 421/340/271/135 MV: AC, IFR 50, FiO2 25%, TV 360, PEEP 5, BUR 12 REFERRALS 745 CN 4018042 SERRA, IGNACIO 40/M Dr. Roa(pulmo)/Dr. Pasco(Neuro)Dr. Ang CC: Dyspnea IVF: For home care preparation c/o Hospice Known case CVD with pneumonia unable to wean. S/p PEG and Tracheostomy last February and was discharged Diet: OF Including mech vent RE addmited last March due to dyspnea and increase productive CVD bleead Basal Ganglia/Pons and Midbrain Pneumonia resolved s/p PEG s/P Tracheostomy Unresponsive, stable Meds: Acetazolomide 250mg/tab Methimazole Nac 60mg/tab Esomeprazole 40mg/tab Lactulose 30cc OD ODHS Levetiracetam 5mil BID per peg Amlodipine 10mg/tab per peg Salbutamol + Ip Bromide For home CO-MANAGEMENT 568-2 CN ROLA, ELIEZER 68/M Dr. Ignacio/Dr. Bausa Pancreatic CA w/ intestinal mets s/p EGD CC: UGIB HPI: Known case of Pancretic CA with intestinal mets s/p surgery, s/p Chemotherapy 3 months PTA, patient had melena and hematemesis which was followed by gen body weakness Meds: Morphine 10mg ½ tab q 6 RTC If tab is not available give Morphone 3mgIV q4 Metoclopramide 1omg/tab Omeprazole 40mg/IV q8-> 40 mg PO BID HNBB 10mg IV q8 Tramadol 50mg/IV Tranexamic acid 1amp TID PRN Norspan 5mg patch q 7 days Levofloxacin 750mg tab OD Senna Forete 374mg tab OD HS CBC 95/0.241/7.89/445 MGH once settled PF 4.6K Blood Chem BUN 108/Crea 104/AST 27/ALT 10/ALb 29/Ca 2.17/ Na 132/ K 4.6 (+)abdominal pain and distention, black tinged vomitus, nausea EGD result: infiltrating mass at the junction of D1/D2, no active bleeding or ulcers s/p BT1 unit PRBC For BT 1u PRBC CBG 215, 186 For: CXR Sputum gs/cs CI CI 27 B49 CN 3987619 REYES, REMEDIOS 50F 3/14: Sianghio Breast CA Pathologic fracture 2 BRCA metsprobsubtrochantrealacrea Pleural effusion, left 606-2 CI 28 B39 3921342 Known case breast CA with pulmo mets(?) s/p 8 cycle chemo s/p CTT IVF: heplock DOI: 2/17/14 TOI: 10:30AM MOI: fall POI: valenzuela city Antibiotcs: Meropenem 1 grm TIV q 8 D5 Patient had a dental procedure and was about to be transferred to a wheelchair when a cracking sound was heard and patient was noted to have deformity and pain on right thigh CC: Abdominal pain, epigastric CC: Weakness Diet: OF feeding at 1125 kcal Meds: Appebon tab OD Doxophylline 200mg tab BID Morphine Silfate 2 tab q 4 RTC, I tab for BTP Senna 2 tab ODHS Dulcolax supp if no BM for 3 days Furosemide +Kcl tab OD for 7 days DISCHARGED Metoclopromide 10mg tab q 8 prn HNBB 1omg TIV q 6 PRN Calmoseptine ointment IVF: PNSS 1l x 12h BID Salmeterol + Fluticasone 200 ,cg I puff BID Salbu + ipra neb q 4 prn Gaviscon q8 PRN KCl 10% 30cc 1 of 4 IVF: PNSS 1L 8 hours for 1 cycle PNSS 1L x12 hours HPI: RONQUILLO, MILAGROS CERVANTES 61/F 3/6 Shianghio Breast CA stage IV S/p Chemo 6 cycles Known Case of Breast CA stage IV with bleeding, S/P Chemo 6 cycles, HPN stage, Tyoe 2 DM 1 month Patient had general body weakness and pale looking. CBC was done and revealed a 85 hemoglobin Few hours PTA, patient fainted after walking at the stair in PGh. Hold Enalapril 10mg/tab OD Gliclazide 80mg/tab Simvastatin 10mg ODHS Tamoxifen 20mg/OD Vitamin D + Caco3 tab Bisacodyl ODHS Metformin 500mg/tab BID Ferrous Sulfate tab Gabapenin 300mg/tab BID Tranexamic acid 500mg/tab Tramadol 50mg q8 MoSO4 10mg a tab q 4 RTC CBC: 3/18: 125/0.380/4.82/0.76/0.09/328 3/6: 108/0.340/4.06/0.83/0.09/413 Blood chem: 3/17: Na 125 K 3.1 Cl 95 Crea 23 AST 44 ALT 19 alb 23 Ca 1.82 TP: 60 LDH 1342 Clear CTT output DNR/DNI status No chemo No radio Refer to GS, still awaiting entry Refer for Dietary for upbuilding Blood CS: NG2D PT/PTT: 2/21: 13.3/12.4/116/0/92 29/25.8 ECG: RSR, NA, LAE, NSSTTWC CBC 3/22 119/0.371/6.31/0.84/0.11/0.04/0.01/381 3/9: 113, 0.354, 6.11, 0.63, 0.26 3/5: 71/0.237/6.61/0.55/0.38/599 (-) bloody discharge per CTT s/p BT 2 u PRBC For: U/A Post correction Mg, K, Cl Chest UTZ s/p Open Chole (3/28) s/p 6/10 RT Complains of dizziness and stress, hip pain 4/10 relieved by analgesic With BTP 1x and unable to proceed with RT PT/PTT 3/5: 13.3/12.6/112/0.94 29/28.5 Bloodchem: 3/10: BUN 3.3, Crea 70 3/6:Chole 3.02 TG 0.78 HDL 1.13 LDL 1.54 FBS 5.5 HBa1c: 5.0 Na 143 K 2.8 Cl 105 cra 92 AST 40 ALT 14 alb 34 Ca 2.39 ECG: RSR, NA, NSSTTWCs Urinalysis 3/6: 5.5/1.020/neg/neg/rbc 0. Wbc 205 CT scan provisional No mass, increase hemidiagram left Positive consolidation left Follow-up Chest CT scan with Contrast For rehab referral for possible bracing Bone scan: 3/17: multiple bone metastasis with progression since 4/29/13 Wound GS Gram neg bacilli 3-5 Gram + cocci 2-4 E. Coli mod-heavy growth P. Aeruginosa S. Ceftazidime Gentamicin CN MANUTA, BUENA 60/f 3/25 ALEX Dr. Tordesillas/Dr. De Vera(GS3)/Dr. Dans (CVS) HPI: History of epigastric pain last 2012, relieved with unknown meds. Diet: DAT Few hours PTA, patient had epigastric pain, burning with reflux. Seen at ambu and given Ranitidine and Metoclopramide. Pain decrease but still persisted hence admission Meds Omeprazole 40mg/IV OD D/c HNBB 10mg/IV AlMg OH 2 sachet 3x a day Atorvastatin 10mg tab ODHS Cefuroxime 750mg IV q8 – d/c Simvastatin 40 mg ODHS (suggested by CVS) Arcoxia 120mg/tab once a day CC: hip pain HPI: 15 hrs PTA – (+) fall from the stairs allegedly falling on her buttocks and not hitting the head. Consulted at FMAB xray done showed (-) for fracture. IVF: heplock DAT CBC 126/0.401/201/9.24 Meds: Tramadol 50mg IV q12 shift 50mg/tab TID Amlodipine 5mg tab OD Colchicine 500mg tab OD Blood Chem Na 137/k 2.6/Cl 1000/Bun 2.3/Crea 73/Ca 2.13 GERD Calculous cholecystitis 416-4 CN ARRIESGADO, PREMITIVA HA-UTS: fatty liver changes, calculous cholecystitis CXR: provisional suboptimal inspiration, intercurrent pneumonia not ruled out Had back pain yesterday from previous history of Slip Disc For possible D/c today once with no symptoms Blood Chem: Na 136, K 3.8, Cl 103, Chole 245, TG 83, HDL 74, LDL 155, FBS 126 BUN 2.9 crea 72 BUA 0.33 AST 37 ALT 28 alb 39 Ca 2.38 Mg 0.87 HBA1c 5.7 Urinalysis: Yellow/clear/6.0/1.009/RBC 35/WBC 9 (+) hip pain decrease 3/10 For possible discharged 83/F No pain For: Uric acid, Lipd profile 3/28: Michelle Dr. Limpoco/Dr. Tee (Rheuma) Osteoarthritis HTN St II, controlled MORTALITY