Nuclear Medicine Diagnoses What?
advertisement
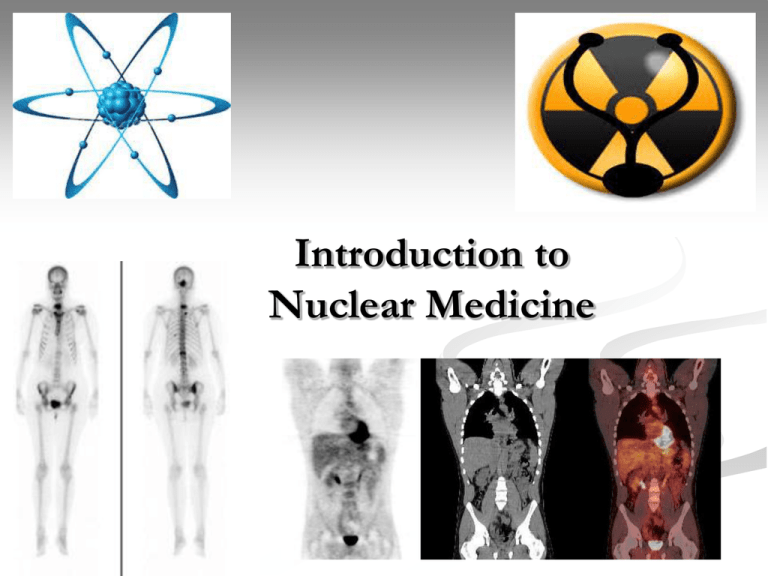
Introduction to Nuclear Medicine What is Nuclear medicine? It is the use of radioactive materials in medicine. It may be either diagnostic or therapeutic In the therapeutic issue we must differentiate between Brachytherapy (internal radiotherapy) sealed source radiotherapy is a form of radiotherapy where a radiation source is placed inside or next to the area requiring treatment. Brachytherapy is commonly used as an effective treatment for cervical, prostate, breast, and skin cancer and Teletheraby (External beam radiotherapy). Kilovoltage ("superficial") X-rays are used for treating skin cancer and superficial structures. Megavoltage ("deep") X-rays are used to treat deep-seated tumors (e.g. bladder, bowel, prostate, lung, or brain). Nuclear Medicine Procedures Nuclear medicine procedures may be: diagnostic studies, which are tests of body function therapeutic procedures in which the radiation is used to treat disease. Radionuclide therapy is used in the treatment of both benign disease (eg hyperthyroidism and arthritis) and malignant disease (eg thyroid cancer, Suprarenal gland tumors and hepatocellular carcinoma) Nuclear Medicine Diagnoses What? Radiopharmaceuticals The radioactive materials administered to patients are known as radiopharmaceuticals. These consist of : a chemical molecule which determines the behavior of the radiopharmaceutical in the body a radionuclide. The radiation emitted by the radionuclide may be detected from outside the body by a radionuclide imaging device (a gamma camera) or may be detected in a sample of a body fluid (eg plasma or urine) Radiopharmaceuticals Diagnostic radiopharmaceuticals must deliver the minimum possible radiation dose to the patient while still obtaining the required diagnostic information. Therapy radiopharmaceuticals must deliver the maximum radiation dose to the diseased organ or tumor, while minimizing the radiation dose to nontarget tissues such as the bone marrow. The Ideal Radionuclide for In-vivo Imaging It must emit photons in high abundance in energies which can be efficiently detected by the gamma camera (100 keV - 300 keV) It should not emit charged particles as these are absorbed within a few millimetres of tissue. These can not be detected outside of the body and greatly increase the radiation dose to the patient. It should have a short half-life, again to keep the radiation dose as low as possible. The Ideal Radionuclide for Therapy Must emit energetic charged particles. These are usually beta particles but may be Auger electrons, internal conversion electrons or even alpha particles. Low cost, available, safe. A fairly short half-life, typically several days. Targeting the Right Tissue or Organ The metabolism of the radiopharmaceutical in the body will depend on its chemical properties. Some are simple ions, such as 67Ga citrate and sodium 131Iodide Some are particles or aggregates of molecules labelled with a radionuclide Some are radio-labelled blood cells (red cells or white cells) The remainder are labelled complex molecules, such as phosphonates, peptides and antibodies. Clinical applications Bone scintigraphy: is a study of the skeletal system that uses a form 99mTc injected intravenously absorbed by the bone. Genitourinary studies: provides both an anatomic and functional evaluation of the kidneys especially after transplantation. Brain scan: evaluate various neurologic conditions as Alzheimer and Parkinson disease. Thyroid uptake study: to evaluate functions of the thyroid gland using sodium iodide 131I. Radionuclides in Common Use Four radionuclides account for the large majority of clinical procedures. These are : principal g energy 140 keV 99mTc T½ 6 hours 131I T½ 8 days 67Ga T½ 3.3 days principal g energies 93 keV, 184 keV and 296 keV T½ 3 days x-ray emission at 70-80 keV 201Tl principal g energy 360 keV Nuclear Medicine Team Nuclear medicine technologist: responsible for handling, assessment, and administration of radionuclides, patient safety, statistical analysis for digitally processed images, decontaminate the area. Nuclear medicine physician: radiologist has received training in the performance and interpretation of nuclear medicine procedures. Medical nuclear physicist: received advanced training in nuclear physics, computers, and radiation safety. Responsible for preparing radioactive materials and calibration and maintenance of imaging equipment. Radionuclide Imaging and Radiation Safety (1) Unlike Diagnostic Radiology and Radiotherapy, Nuclear Medicine imaging devices do not emit radiation. The technologist may take as many images as required to provide the diagnosis without changing the radiation exposure of the patient. Radionuclide Imaging and Radiation Safety (2) However, a malfunctioning gamma camera may result in errors in diagnosis or an non-interpretive study so that the patient gets no benefit from the radiation exposure arising from the administered radiopharmaceutical. It is therefore essential that the principles of radionuclide imaging are well understood, that the quality control procedures are routinely performed and that the gamma camera is serviced when required. Advantages of Nuclear medicine imaging Functional Sensitive, quantitative. Very safe. Low radiation. Screening & Follow up Whole body evaluation without increased radiation dose to the patient. Very high specificity (no natural radioactivity from the body). Disadvantages of Nuclear medicine imaging Not widely available. Poor SNR. Require NM instruments & radiopharmaceuticals. Relatively higher cost than X-ray or US. Radiation exposure to the patient. Low spatial resolution (5-10mm). Slow image acquisition.