Other benign headaches
advertisement

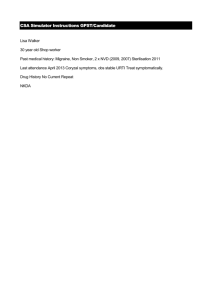
Pharmaceutical guidelines of patients with pathology of CNS organs. Symptomatic treatment of HEADACHE Headaches • Headache is an almost universal experience and one of the most common symptoms in medical practice. It varies from an infrequent and trivial nuisance to a pointer to serious disease. Mechanisms Pain receptors are located at the base of the brain in arteries and veins and throughout meninges, extracranial vessels, scalp, neck and facial muscles, paranasal sinuses, eyes and teeth. Curiously, brain substance is almost devoid of pain receptors. Head pain is mediated by mechanical and chemical receptors (e.g. stretching of meninges, 5-HT and histamine stimulation). Nerve impulses travel centrally via the Vth and IXth cranial nerves and upper cervical sensory roots. Most headaches are benign, but the diagnostic issue – and usual concern – is the question of serious disease. Chronic (benign) and recurrent headaches • Almost all recurring headaches lasting hours or days – band-like, generalized head pains, with a history for several years or months – are vaguely ascribed to muscle tension and/or migraine • Depression is a common accompaniment. • In localized pain of short duration (minutes to hours), sinusitis, glaucoma and migrainous neuralgia should be considered. • Headaches are not caused by essential hypertension; malignant hypertension, with arterial damage and brain swelling, occasionally causes headache. • Eyestrain from refractive error does not cause headache, though new prescription lenses sometimes provoke pain. Cluster Headache Tension headache The vast majority of chronic daily headaches and recurrent headaches are thought to be generated by neurovascular irritation and referred to scalp muscles and soft tissues, although the exact pathogenesis remains unclear. Tight band sensations, pressure behind the eyes, throbbing and bursting sensations are common. What is clear is that almost all headaches with these features are benign. There may be obvious precipitating factors such as worry, noise, concentrated visual effort or fumes. Depression is also a frequent co-morbid feature. Tension headaches are often attributed to cervical spondylosis, refractive errors or high blood pressure: evidence for such associations is poor. Headaches also follow even minor head injuries. Tenderness and tension in neck and scalp muscles are the only physical signs. Analgesic overuse is a prominent cause of headache. Pressure headaches • Intracranial mass lesions displace and stretch meninges and basal vessels. Pain is provoked when these structures are shifted either by a mass or by changes in cerebrospinal fluid (CSF) pressure, e.g. coughing. Cerebral oedema around brain tumours causes further shift. These ‘pressure headaches’ typically become worse on lying down. • Any headache present on waking and made worse by coughing, straining or sneezing may be due to a mass lesion. • Vomiting often accompanies pressure headaches. Such headaches are caused early, over days or weeks, by posterior fossa masses, but over a longer time scale – months or years – by hemisphere tumours. • A rare cause of prostrating headache with lower limb weakness is an intraventricular tumour causing intermittent hydrocephalus. Headache of subacute onset • The onset and progression of a headache over days or weeks with or without features of a pressure headache should always raise suspicion of an intracranial mass or serious intracranial disease. • Encephalitis, viral meningitis and chronic meningitis should also be considered. Headaches with scalp tenderness • Patches of exquisite tenderness overlying superficial scalp arteries are caused by giant cell arteritis in patients over 50. Headache following head injury • The majority of post-trauma headaches lasting days, weeks or months are not caused by any serious intracranial pathology. • However, subdural haematoma must be considered. A single episode of severe headache • This common emergency is caused by one of the following: ■ subarachnoid haemorrhage (SAH) and cervical arterial dissection ■ migraine, or other benign headaches ■ meningitis (occasionally). • Particular attention should be paid to • suddenness of onset (suggestive of SAH). • The exact time of onset, • time to peak, duration, • associated symptoms and previous headache history should be documented. • Neck stiffness, vomiting (meningeal irritation) and a rash and/or fever suggest bacterial meningitis. Management Headache management involves: ■ explanation (imaging is often needed) ■ avoiding evident causes, e.g. bright lights ■ physical treatments – massage, ice packs, relaxation ■ antidepressants – when indicated ■ drugs for recurrent headache/migraine. Migraine • Migraine is recurrent headache associated with visual and gastrointestinal disturbance. • The borderland between migraine and tension headaches can be indistinct. Over 20% of any population world-wide report migrainous symptoms; in 90%, these began before 40 years of age. Migraine. Mechanisms • Precise mechanisms remain unclear. Genetic factors play some part – a rare form of familial migraine is associated with mutation in the alpha-1 subunit of the P/Q-type voltagegated calcium channel on chromosome 19. • The pathophysiology of migraine is now thought to involve changes in the brainstem blood flow which have been found on PET scanning during migraine attacks. • This leads to an unstable trigeminal nerve nucleus and nuclei in the basal thalamus. This results in release of calcitonin-related peptide (CGR8), substance P and other vasoactive peptides, leading to neurogenic inflammation, which gives rise to pain, and vasodilation of cerebral and dural vessels which also contribute towards the headache. • Cortical spreading depression is also proposed as a mechanism for the aura. Some patients recognize precipitating factors: ■ weekend migraine (a time of relaxation) ■ chocolate (high in phenylethylamine) ■ cheese (high in tyramine) ■ noise and irritating lights ■ association with premenstrual symptoms. Migraine is common around puberty and at the menopause and sometimes increases in severity or frequency with hormonal contraceptives, in pregnancy and occasionally with the onset of hypertension or following minor head trauma. Migraine is not suggestive of any serious intracranial lesion. However, since migraine is so common, an intracranial mass and migraine sometimes occur together by coincidence. Clinical patterns • Migraine attacks vary from intermittent headaches indistinguishable from tension headaches to discrete episodes that mimic thromboembolic cerebral ischaemia. • Distinction between variants is somewhat artificial. • Migraine can beseparated into phases: ■ well-being before an attack (occasional) ■ prodromal symptoms ■ the main attack – headache, nausea, vomiting ■ sleep and feeling drained afterwards. Migraine with aura (classical migraine) • Prodromal symptoms are usually visual and related to depression • of visual cortical function or retinal function. • Transient aphasia sometimes occurs, with tingling, numbness, vague weakness of one side and nausea. • The prodrome persists for a few minutes to about an hour. • Headache then follows. This is occasionally hemicranial (i.e. splitting the head) but often begins locally and becomes generalized. • Nausea increases and vomiting follows. The patient is irritable and prefers the dark. • Superficial scalp arteries are engorged and pulsating. • After several hours the migraine settles, sometimes with a diuresis. • Deep sleep often ensues. Migraine without aura (common migraine) • This is the usual variety. Prodromal visual symptoms are vague. • There is a similar headache often accompanied by nausea and malaise. Basilar migraine • Prodromal symptoms include circumoral and tongue tingling, vertigo, diplopia, transient visual disturbance, syncope, dysarthria and ataxia. • These occur alone or progress to a typical migraine. Hemiparetic migraine • This rarity is classical migraine with hemiparetic features, i.e. resembling a stroke, but with recovery within 24 hours. • Exceptionally, cerebral infarction occurs. Ophthalmoplegic and facioplegic migraine • These rarities are a IIIrd, VIth or VIIth nerve palsy with a migraine, and they are difficult to diagnose without investigation to exclude other conditions. Differential diagnosis • A sudden migraine headache may resemble SAH or the onset of meningitis. • Hemiplegic, visual and hemisensory symptoms must be distinguished from thromboembolic TIAs • In TIAs maximum deficit is present immediately and headache is unusual. • Unilateral tingling or numbness may resemble sensory epilepsy (partial seizures). In epilepsy, distinct march (progression) of symptoms is usual. Management General measures include: ■ avoidance of dietary factors – rarely helpful. • Patients taking hormonal contraceptives may benefit from a brand change, or trying without. Depot oestrogens are sometimes used. Severe hemiparetic symptoms are a potential reason to stop hormonal contraceptives. • Premenstrual migraine sometimes responds to diuretics. At the start of an attack • Paracetamol or other analgesics should be taken, with an antiemetic such as metoclopramide if necessary. Repeated use of analgesics leads to further headaches. • Triptans (5HT1 agonists) are also widely used, sometimes aborting an attack effectively. Sumatriptan was the first marketed; almotriptan, eletriptan, frovatriptan, naratriptan, rizatriptan and zolmitriptan are now available, with various routes of administration. • Triptans should be avoided when there is vascular disease, and not overused. Ergot Derivatives • cause constriction of cranial blood vessels and decrease the pulsation of cranial arteries. As a result, they reduce the hyperperfusion of the basilar artery vascular bed. • Because these agents are associated with many systemic adverse effects, their usefulness is limited in some patients. The ergots are contraindicated during pregnancy because of the potential for adverse effects in the mother and fetus. • Dihydroergotamine (Migranal) can be used in the IM or IV form or as a nasal spray to provide rapid relief from migraine headache. This agent is the drug of choice if the oral route of administration is not possible. In 2003, the parenteral form was approved for the treatment of cluster headaches. Ergot Derivatives (cont’d) • Ergotamine(generic), the prototype drug in this class, was the mainstay of migraine headache treatment before the triptans became available. This agent is administered sublingually for rapid absorption. Cafergot, the very popular oral form, combines ergotamine with caffeine to increase its absorption from the GI tract. Contraindications and Cautions • Ergot derivatives are contraindicated in the following circumstances: presence of allergy to ergot preparations; CAD, hypertension, or peripheral vascular disease, which could be exacerbated by the CV effects of these drugs; impaired liver function, which could alter the metabolism and excretion of these drugs; and pregnancy or lactation because of the potential for adverse effects on the fetus and neonate. Ergotism (vomiting, diarrhea, seizures) has been reported in affected infants. • Caution should be used in two instances: with pruritus, which could become worse with drug-induced vascular constriction, and with malnutrition because ergot derivatives stimulate the CTZ and can cause severe GI reactions, possibly worsening malnutrition. Adverse Effects • The adverse effects of ergot derivatives can be related to the drug-induced vascular constriction. • CNS effects include numbness, tingling of extremities, and muscle pain; • CV effects such as pulselessness, weakness, chest pain, arrhythmias, localized edema and itching, and MI may also occur. • the direct stimulation of the CTZ can cause GI upset, nausea, vomiting, and diarrhea. Ergotism, a syndrome associated with the use of these drugs, causes nausea, vomiting, severe thirst, hypoperfusion, chest pain, blood pressure changes, confusion, drug dependency (with prolonged use), and a drug withdrawal syndrome. Headaches are distributed in the general population in a definite gender-related pattern • Migraine headaches are three times more likely to occur in women than men. • Cluster headaches are more likely to occur in men than in women. • Tension headaches are more likely to occur in women than in men. • There is some speculation that the female predisposition to migraine headaches may be related to the vascular sensitivity to hormones. Some women can directly plot migraine occurrence to periods of fluctuations in their menstrual cycle. The introduction of the triptan class of antimigraine drugs has been beneficial for many of these women. Prophylaxis • The following are used continuously when attacks are frequent: ■ pizotifen (5HT antagonist) 0.5 mg at night for several days, increasing to 1.5 mg (common side-effects are weight gain and drowsiness) ■ propranolol 10 mg three times daily, increasing to 40– 80 mg three times daily ■ amitriptyline 10 mg (or more) at night. • Sodium valproate, methysergide, SSRIs, verapamil, topiramate, nifedipine and naproxen are also used. • Gap junction blockers are being used in trials. Other benign headaches ■ Ice-cream headache. Sufferers describe intense, retropharyngeal head pain lasting for a few seconds or minutes following ice-cream or very cold foods. ■ Primary cough headache is a sudden sharp head pain on coughing. No underlying cause is found but intracranial pathology should be excluded. The problem often resolves spontaneously. Very rarely, for severe headache, a lumbar puncture with removal of CSF can help. ■ Primary low CSF volume headaches, seen typically on standing up, are also well recognized. The patient may give a history of some event, such as straining or orgasm, but these headaches sometimes arise spontaneously. Treatment with an autologous intrathecal blood patch can be helpful. Secondary low CSF volume can follow lumbar puncture Other benign headaches (cont’d) ■ Primary sex headache describes varieties of head pain that typically rise to a crescendo at orgasm, largely in males. Treatment with propranolol or diltiazem is said to be helpful, but these pains often resolve spontaneously after several attacks. Exceptionally, sex headaches occur with an unruptured intracranial aneurysm. ■ Many other varieties of primary headache are listed in the international classification, e.g. hemicrania continua, primary stabbing headache, primary exertional headache, hypnic headache, and primary thunderclap headache. ■ Post-traumatic headache is also a common problem. Headaches do sometimes follow a minor blow to the head; they tend to resolve, typically within 6–8 weeks. However, when there is third party involvement, and especially with litigation, these headaches can persist for long periods. Opinions vary about their cause.