Northumbria University. Northumberland NHS
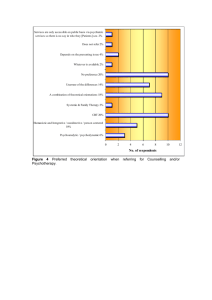
advertisement

CBT for Adults with Intellectual Disabilities: Adaptations and The Evidence Base IAPT: Evidence and Experience of Supporting People with Learning Disabilities Castle Green Hotel, Kendal, Friday, 23rd May 2013 John L Taylor Professor of Clinical Psychology/ Consultant Clinical Psychologist Northumbria University/ Northumberland, Tyne & Wear NHS Foundation Trust Mental Health Problems and People with ID - Vulnerability People with ID may be more likely to experience MH problems than the general population for a number of reasons (Deb et al., 2001; Moss et al., 1998). These include: • predisposing biological factors • limited psychological coping resources • increased exposure to psycho-social stressors e.g. - deprivation/poverty √√√ - stigmatisation - social isolation - traumatising abuse experiences Mental Health Problems and People with ID - Prevalence Prevalence studies of MH problems amongst people with ID report large variations in prevalence rates depending on: • Study design and methodology (e.g. case note review vs. clinical evaluation, sampling) • Location of the sample (e.g. in-patient vs. community vs. specialist service) • The type of assessment instrument used to detect MH problems (e.g. screening assessment vs. full diagnostic assessment) • The reliability and validity of the assessment instruments used to detect MH problems • Whether or not ‘challenging behaviour’ is included as a MH problem Mental Health Problems and People with ID Prevalence Rates using Screening Instruments Prevalence % Study N Total Affective/ Neurotic Organic Disorder Psychotic Disorder 1,155 20.1* 14 3.9 10.2 Iverson & Fox (1989) 165 36 (Random sample of service users) Reiss (1990) 205 39 (Random sample of service users) Roy et al. (1997) 127 33 (Consecutive sample from SSD register) Deb et al. (2001) 90 22.2 Taylor et al. (2004) (Random sample of service users) *Note. 4.4% were above threshold for >1 diagnostic category. Mental Health Problems and People with ID Prevalence Rates involving Clinical Assessments* Study N Prevalence % 1,023 18 Cooper & Bailey (2001) 207 22 Lund (1985) 302 17 Corbett (1979) 402 21 Cooper et al. (2007) *Note. Rates excluding behaviour problems calculated using data presented by Copper et al. (2007) in Table 6, p. 33 Lack of Awareness of Mental Health Problems and Needs of People with ID Despite the prevalence of these problems, there is a general lack of awareness of the needs of people with ID and MH problems (Taylor & Knapp, 2013). Reasons include: • Concern on the part of service commissioners and providers to act if these needs were better understood • A general lack of interest in the needs of people seen as different • People with ID are often considered not bright enough to understand to to benefit from psychological therapies • The ‘Unoffered Chair’ (Bender, 1993) therapists are reluctant to offer individual psychological therapy to people perceived as unattractive because of their disability – ‘therapeutic disdain’ Against Psychotherapy With People Who Have Mental Retardation Sturmey P. (February, 2005). Against Psychotherapy With People Who Have Mental Retardation. Mental Retardation, 43, 55-57. ‘Hence, we are unable to make any conclusions as to the effectiveness, ineffectiveness, or harmful effects of psychotherapy based on scientific evidence.’ (p. 56) Evidence-Based Practice in the New NHS • All NHS treatment (including psychological therapies) should be evidence-based (Department of Health (1999) Clinical Governance: Quality in the NHS) • NICE guidelines for depression, anxiety, panic, OCD, trauma, psychosis, etc. • So, what is the evidence for the effectiveness of psychotherapy for people with ID and MH problems? • There have been a number of reviews/commentaries/ critiques Evidence for Psychotherapy for People with ID - I Hatton, C. (2002). Psychosocial interventions for adults with ID and mental health problems: A review. J. of Mental Health • Depression – 2 case studies and 1 case series showed ↓symptoms for modified CBT • Anxiety – A small number of case studies and case series have showed ↓symptoms for modified CBT and relaxation training • Anger – 2 narrative reviews of psychological treatments – A number of case studies and case series showed ↓symptoms for modified CBT – 3 small trials of CBT have showed significant treatment effects • Psychosis – 2 case studies using behavioural interventions showed ↓ “psychotic speech” – 1 case study showed ↑ self-management of hallucinations for modified CBT Evidence for Psychotherapy for People with ID - II Prout, H.T. & Nowak-Drabik, K.M. (2003). Psychotherapy for persons who have mental retardation. Am. J. on Mental Retardation • Reviewed 92 studies published over a 30-year period • Used a clear definition of psychotherapy • Many studies lacked methodological rigour • In terms of the therapeutic approaches, the studies reviewed included: – – – – – 33% behavioural psychotherapy 15% analytic/dynamic 13% cognitive-behavioural 2% humanistic 37% other • Meta-analysis of treatment effectiveness – mean effect size of 1.01 • Results suggest that individual treatment, behaviourally orientated, and manual-guided provided the best outcomes Evidence for Psychotherapy for People with ID - III Beail, N. (2003). What works for people with MR? Critical commentary on CBT and psychotherapy research. Ment. Retardation • Reviewed and compared CBT and psychodynamic psychotherapy outcome research • For CBT numerous case studies and case series were found and a small number of uncontrolled group studies (mainly in the forensic ID field) • Only a few controlled studies were found : – 2 concerning CBT for problem-solving yielded mixed outcomes – 3 concerning CBT for anger problems yielded significant treatment outcomes • 4 pre-post open trials of psychodynamic psychotherapy were reviewed that were successful in reducing behavioural problems Evidence for Psychotherapy for People with ID - IV Sturmey, P. (2004). Cognitive therapy for people with ID: A selective review & critique. Clin. Psychology & Psychotherapy • Selective review of ‘cognitive therapy’ for anger, depression and sex offending • Suggests that in each of these problem areas the evidence for behavioural interventions is stronger than for cognitive therapy • Better research using controlled, randomised controlled trials and single subject experimental designs are required • Outcome measures require reliability, validity and ‘social validity’ • However, critique based on a “misunderstanding” of what defines psychotherapy (Prout & Browning, 2011) Evidence for Psychotherapy for People with ID - V Willner , P. (2005). The effectiveness of psycho-therapeutic interventions for people with LD: A Critical review. J. of Intell. Disability Research • CBT cognitive skills approaches show promise for a range of problems including: stereotyped behaviour, social anxiety, sexually inappropriate behaviour, anger control, and anxiety • CBT cognitive distortion approaches have quite limited evidence to support their use for anger, depression, anxiety and sexual behaviour problems • Conclusion was that there is a “wealth of evidence” (albeit from methodologically weak studies) that people with ID benefit from psycho-therapeutic interventions Evidence for Psychotherapy for People with ID - VI Prout, HT & Browning, BK (2011). The effectiveness of psychotherapy for persons with intellectual disabilities. In RJ Fletcher (ed). Psychotherapy for individuals with disability (pp 265-287). Kingston, NY: NADD Press. • Reviewed psychological treatment studies involving people with ID published between 2006-2011 • Published studies present generally positive results supporting psychological therapy for people with ID • Both individual and group interventions are beneficial • Anger reduction interventions have the most evidence • Doctoral dissertations completed betw. 1993-2009 provide further support for the effectiveness of psychological therapies for people with ID (‘file draw’ phenomenon) Evidence for Psychotherapy for People with ID - VII ‘Reviews of the Reviews’ • Gustafson et al. (2009). Rsch on Social Work Practice – Surveyed systematic reviews of psychosocial interventions for adults with ID – 55 reviews published between 1969-2005 – Only 2 reviews met the inclusion criterion – Concluded that CBT reduced anger at the end of treatment • Prout & Browning (2011). Adv. In Mental Health and Intellectual Disabilities – Narrative review of reviews on psychotherapy for people with ID – Included 7 reviews published between 200-2011 – Research continues to lack a critical mass of studies with robust designs – Psychotherapy is ‘moderately beneficial’ for people with ID and a range of mental health problems Prevalence of Aggression in People with ID Prevalence (%) Study Location n Tyrer et al. (2006) England 3065 16 - - Taylor et al. (2008) England 782 12 - - USA 2491 16 37 - Harris (1993) England 1362 11 38 - Sigafoos et al. (1994) Australia 2412 10 35 - Smith et al. (1996) England 2202 - 40 - Taylor et al. (2004) England 129 - - 47 McMillan et al. (2004) England 124 - - 47 Hill & Bruininks (1984) Community Institution Forensic Impact of Aggression in People with ID • Aggression is the 1° reason for people with ID to be (re)admitted to institutional care (Lakin et al., 1983) • Aggression is the 1° reason for people with ID to be prescribed antipsychotic medication (Aman et al., 1987; Robertson et al., 2000) • Physical violence has a significant negative impact on the rehabilitation of offenders with ID • Physical violence has significant costs staff and services (Jenkins et al., 1997; Kiely & Pankhurst, 1998) • Anger is strongly associated with aggression/violence (Novaco & Taylor, 2004) Cognitive-Behavioural Treatment of Anger for People with ID – Summary of Evidence • Research on anger treatment for people with ID is limited, but there is some evidence of successful CBT-based interventions (see Taylor & Novaco, 2005; Whitaker, 2001 for reviews) • Post-1985 there have been 35 studies published on the effectiveness of psychotherapeutic anger interventions for people with ID • There are 12 reports on small anger CBT outcome studies with ID clients that involved comparison groups (Benson et al., 1986; Hagiliassis et al., 2005; Lindsay et al., 2004; Rose et al., 2000, 2005, 2008, 2009; Taylor et al., 2002, 2004, 2005; Willner et al., 2002, 2005) Cognitive-Behavioural Treatment of Anger for People with ID – Summary of Evidence II • Cochrane Review ‘Behavioural and Cognitive-Behavioural Interventions for Outwardly-Directed Aggressive Behaviour in People with Learning Disabilities’ • Just 4 studies included in final analysis – McPhail & Chamove (1989). RCT, 12 particx, APR vs. no treat. – Nezu et al. (1991). RCT, 28 particx, problem-solving vs. wait list – Taylor et al. (2005). Quasi-RCT, 40 particx, individual AT vs. TAU – Willner et al. (2002). Quasi-RCT, 16 particx, group AM vs waitlist • Conclusions – scant evidence, some evidence of efficacy, could be preferable to drug treatment, more research trials required, cost effectiveness studies needed. Cognitive-Behavioural Treatment of Anger for People with ID – Summary of Evidence III • Nicoll, Beail & Saxon (2013). JARID – Systematic Review and meta-analysis of CBT for anger in adults with ID – 12 studies published between 1999-2011 met the inclusion criteria (10 UK; 2 Australia) – All studies utilised the Novaco CBT approach – Studies showed high levels of reporting and internal reliability – Studies showed lower levels of internal reliability sampling and external validity – 9 studies included in the meta-analysis – Overall large uncontrolled ES = 0.88; 6 group treatment studies ES = 0.84; 3 individual treatment studies ES = 1.01 – Review reveals an ‘emerging evidence base’ for CB anger interventions for adults with ID; studies show ‘a good level of methodological rigour’ Is ‘Therapeutic Disdain’ Still Justified? Probably not! 1) The need for psychological therapies is demonstrable given the prevalence of MH problems in this population 2) The evidence to support psychological therapies, particularly CBT, is limited, but is growing and is positive 3) The levels of professional interest and skills in this area are increasing, but requires more support 4) Clients with ID and enduring mental health problems can be successfully engaged in, and motivated to undertake CBT based on an individual analysis and formulation of their problems 5) In particular, clients complex problems and few psychological resources, can benefit from intensive individual manual guided cognitive-behavioural treatment.