Health and Safety Awareness
advertisement

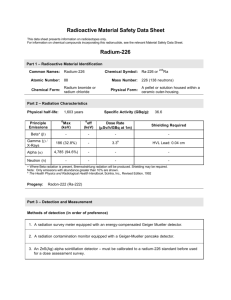
An Introduction to Radiation Safety 2014 Ian Williamson / Steve Clipstone Restricting Exposure • Alle Ding' sind Gift, und nichts ohn' Gift; allein die Dosis macht, daß ein Ding kein Gift ist. • "All things are poison and nothing is without poison, only the dose permits something not to be poisonous." (Paracelsus, 1493 - 1541) This course will cover • • • • • Main requirements of legislation Types of radiation Health effects Management arrangements Risk control measures 3 Aim The aim of the session is to • Introduce you to some basic radiation principles • Inform you of the arrangements and control measures in place to keep you safe when working with radiation • Not to make you an expert! Early uses of radioactivity • Radium and thorium Radiation Injuries • 1896 - first injuries due to radiation recorded • 1902 - first skin cancers seen • 1911 – 94 cases of skin carcinomas and sarcomas reported • H&S Legislation needed? Legislation • Ionising Radiation Regulations 1999 (IRRs) General and specific duties & rules about safe working practices, control measures, assessments, roles and responsibilities; Health and Safety Executive (HSE) enforcement • Environmental Permitting Regulations 2010 Regulates the holding, storage, accumulation and disposal of radioactive material; Environment Agency (EA) Enforcement Replaced the RSA93 Act The Ionising Radiation Regulations • • • • • • • • • Risk assessments Control of exposure to ALARP Maintenance of control measures Dose limitation Contingency Plans and Local Rules RPA and RPS defined roles Information. Instruction and Training Co-operation between employers Designation of areas Dose Limits – For Workers • • • • • • 1934 1937 1950 1956 1977 2000 2 mSv per day or 730 mSv per year 2 mSv per day or 10 mSv per week 3 mSv per week or 150 mSv per year 1 mSv per week or 50 mSv per year 50 mSv per year 20 mSv per year Average annual dose to UK population (2.6 mSv) Gamma rays from ground and buildings 14% Radon gas from the ground 50% Medical 14% Cosmic rays 10% Products 0.1% Food and drink 11.5% Fallout 0.2% Occupational 0.3% Nuclear discharges <0.1% Annual Dose Limits – UK (IRRs) Whole Body Extremities and skin Lens of the eye Employees aged 18 and over 20 mSv 500 mSv 150 mSv (20) Trainees aged 18 and under 6 mSv 150 mSv 50 mSv (15) Any other person ( e.g. Undergraduates) 1 mSv 50 mSv 15 mSv (15) (new proposed limits in brackets) Women of reproductive capacity - exposure of abdomen limited to 13 mSv in any consecutive 3 month period. Women are legally obliged to inform their employer Basic Radiological Safety Rules • All work must be risk assessed • You MUST work within the Local Rules and follow instructions • You MUST be a registered radiation worker • You MUST understand the instructions and comply with them – if in doubt ask The ALARP Principle • Minimise the time you spend near a source • Maximise the distance between you and a source of radiation • Maximise the shielding between you and a source of radiation Time • Before the work make sure you know and plan what you are going to do! Minimise the time • Practice the task beforehand • Do not linger in high dose rate areas Distance • Avoid working or standing in high dose rate areas, whenever possible by moving away from the source of radiation • Use remote handling equipment • Observe from a separate area • Use minimal amounts / samples Inverse Square Law Distance Double Treble Quadruple Radiation Dose rate Reduced to ¼ Reduced to 1/9 Reduced to 1/16 Shielding • Use shielding provided where possible • Do not tamper with equipment or defeat interlocks • View behind protective screening • Make sure sealed sources are in good repair • PPE Radiation Units Activity • Number disintegrations per second (Becquerel) – one Bq means one atom/nucleus decays and emits radiation every second • Characterised by the half life Absorbed dose • Mean energy per unit mass absorbed by any medium by any type of ionising radiation (Gray – Gy (or joules/kg)) Equivalent Dose • Dose allowing for type of radiation and effective biological damage (Sievert - Sv)- absorbed dose by weighting factor Old/US Units • Rad • Rem • Ci 100 Rads = 1 Gray 100 Rem = 1 Sievert 1 Curie = 3.7 x 1010 Bq (dps) Types of radiation alpha • 2 protons + 2 neutrons tightly bound together - Helium nucleus • High energy but low penetrating power • Range in air only a few cm • Internal hazard beta • • • • Smaller than alpha An electron (emitted from the nucleus) Variable energy Internal and external hazard Gamma and x-rays • • • • • • Electromagnetic radiation Variable energy with shorter wavelengths External hazard Penetrating – range in air m to km Gamma rays emitted from the nucleus X-rays emitted from electron orbital shells Radiation Penetration in air Stopped by Alpha 3 – 5 cm of air Thin sheet of paper, outer layers of skin Beta 3 m of air 1cm perspex 3mm of aluminium sheet Gamma Eventually stopped by air, depends on the energy of emission but can be big distances 40 cm of lead – stops almost all of the radiation Radioactive Half-Life Not all of the atoms of a radioisotope decay at the same time, but they decay at a rate that is characteristic to the isotope. The rate of decay is a fixed rate called a half-life. The half-life of a radioisotope describes how long it takes for half of the atoms in a given mass to decay. Some isotopes decay very rapidly and, therefore, have a high specific activity. Others decay at a much slower rate – so decay at an “average rate” After two half-lives, there will be one quarter the original sample, after three half-lives one eighth the original sample, and so forth. It is an exponential decay process = radioactive At start there are 16 radioisotopes 100% After 1 half life half have decayed. There are 8 remaining 50% = stable, although not a precise figure After 2 half lives another half have decayed. There are 4 remaining After 3 half lives another 2 have decayed. There are 2 remaining 25% 12.5% How can we work out the half-life of a radioisotope? We can plot a graph of activity against time 1 Half-Life 2 Half-Lives Routes of exposure Eye dose Inhalation Skin dose Ingestion Whole body dose Abdomen/Foetal Dose Extremity dose Injection Routes of Entry • • • • Ingestion Inhalation Puncture wounds or cuts Absorption through the skin Absorption of Nuclear Radiations The most massive of the radioactive emissions – alpha particles – have the shortest range. Due to their size they interact strongly with matter (lots of collisions with atoms) causing large amounts of ionization. This makes them very harmful to living tissue. Absorption of Radiation Beta particles being smaller have a weaker interaction but can still cause ionization as they interact with the electrons surrounding atoms. Since gamma radiation is electromagnetic waves it is the most penetrating and least ionizing. However the deep penetration makes it dangerous to living tissue. Biological Effects of Ionising Radiation • Health Effects are determined by the type and intensity of the radiation and the period of exposure. Biological Effects The occurrence of particular health effects from exposure to ionizing radiation is a complicated function of numerous factors including: •Type of radiation involved. All kinds of ionizing radiation can produce health effects. The main difference in the ability of alpha and beta particles and Gamma and X-rays to cause health effects is the amount of energy they have. Their energy determines how far they can penetrate into tissue and how much energy they are able to transmit directly or indirectly to tissues. •Size of dose received. The higher the dose of radiation received, the higher the likelihood of health effects. •Rate the dose is received. Tissue can receive larger dosages over a period of time. If the dosage occurs over a number of days or weeks, the results are often not as serious if a similar dose was received in a matter of minutes. •Part of the body exposed. Extremities such as the hands or feet are able to receive a greater amount of radiation with less resulting damage than blood forming organs housed in the torso. •The age of the individual. As a person ages, cell division slows and the body is less sensitive to the effects of ionizing radiation. Once cell division has slowed, the effects of radiation are somewhat less damaging than when cells were rapidly dividing. •Biological differences. Some individuals are more sensitive to the effects of radiation than others. Studies have not been able to conclusively determine the differences. Radiation Effects • Direct ionisation – Structural cell damage, weakens links between atoms – Affects cellular function – DNA mutations • Indirect ionisation – Damage to chemical constituents, e.g. water – Formation of free radicals Examples of various tissues and their relative radiosensitivities: High Radiosensitivity - Lymphoid organs, bone marrow, blood, testes, ovaries, intestines Fairly High Radiosensitivity- Skin and other organs with epithelial cell lining (cornea, oral cavity, esophagus, rectum, bladder, vagina, uterine cervix, ureters) Moderate Radiosensitivity - Optic lens, stomach, growing cartilage, fine vasculature, growing bone (note optic lens may move up to high radiosensitivity) Fairly Low Radiosensitivity - Mature cartilage or bones, salivary glands, respiratory organs, kidneys, liver, pancreas, thyroid, adrenal and pituitary glands Low Radiosensitivity - Muscle, brain, spinal cord Effects can take between 5 – 30 years Radiation effects • Stochastic effects – somatic and hereditary effects • No safe dose or threshold – governed by chance • Deterministic effects – loss of function • There is no such thing as a safe level of radiation. A single electron could damage a cell irreversibly and initiate cancer However the likelihood of damage and the severity of damage increases with the amount of radiation. Types of exposure • Acute exposure Takes place over a short period of time Usually high exposures • Chronic exposure Takes place over a long period of time Usually low level exposures Stochastic effects Probability Effect, e.g. malignancy and hereditary effects Not immediately observable Dose probability increase as dose received increases Deterministic Effects Severity Threshold Effect, e.g. cataracts, fetal damage, skin effects Large dose can be fatal Dose Degree of cells killed increases with dose impairing organ function Deterministic Effects • • • • 50 mSv body repairs itself 1 Sv nausea and vomiting 3 Sv Erythema, blistering and ulceration 6 Sv LD50 depletion white blood cells, 50% population exposed die of infection death • 10 Sv severe depletion of cells lining intestine, death due to secondary infections Radiation Detectors • Geiger counters, scintillation counters, ionisation chambers; • Count and sensitivity of the detector to interpret the readings Monitors • Use portable radiation detectors to monitor laboratory or facility radiation levels • Use film badges or TLDs for retrospective personal dose monitoring • Calibrated contamination monitors are only valid for a particular type of radiation – there is no universal monitor Work Areas • Controlled areas • Supervised Areas Dosimetry • In controlled areas radiation dose is measured using dose meters or badges – you must wear them every time you enter a controlled area • You will be given specific instructions by your RPS Restricting Exposure • All doses are kept to the ALARP principle Design – fail to safety and cannot be bypassed Engineered – shielded, fail to safety (interlocked), warning lights Administrative – Local Rules, supervision, disposal PPE – gloves , lab coats • Dose limits should not be exceeded Risk Assessment All work requires a risk assessment where the risk is significant and foreseeable. IRRs require: Nature and source of ionising radiation to be used Estimated dose rates to anyone exposed Likelihood of contamination arising and being spread Results of previous monitoring if relevant Control measures and design features Requirement to designate areas and personnel Planned systems of work Estimated levels of airborne or surface contamination likely to be encountered • Requirement for PPE Possible accident situations, potential severity Consequences of failure of control measures Steps to limit consequences of accident situations Local Rules • Brief and concise describing nature of work in the designated area • Identify key work instructions to restrict exposure • Covers normal circumstances and contingency plans • Contains realistic and achievable work instructions • Reviewed periodically to ensure effectiveness • Summary of arrangements for access restriction • Name / contact details of RPS should be in the local rules Waste • Consult with your RPS regarding waste issues Roles and responsibilities • • • • • • Keele University – VC and the Committee Structure Radiation Protection Advisor University Radiation Protection Officer Radiation Protection Supervisor Registered Radiation Worker Agencies / Regulatory bodies Radiation Protection Advisor • • • • Legal requirement Specialist role and appointed in writing Accredited Currently Radman Associates Radiation Protection Advisor Consulted on • Prior examination of plans for new facilities • Critical examination of equipment • Setting up of controlled or supervised areas • Calibration of monitoring equipment • Periodic examination and testing of control measures • Investigations • Compliance with IRRs Radiation Protection Supervisor • Legal requirement • Training and development of staff / students in correct working procedures • Some supervisory duties • Crucial role to ensure compliance with Local Rules, Contingency Plans and general arrangements etc • Familiar with work in their area • Regular checks and record keeping Key Contacts • Radiation Protection Supervisors – list available • University Radiation Protection Adviser (RPA)- Radman Associates • University Radiation Protection Officer – Steve Clipstone • Head of Occupational Health and Safety – Ian Williamson Further information • Keele webpages • HSE Any questions?