Colon Cancer Screening in an Age of Molecular Genetics and
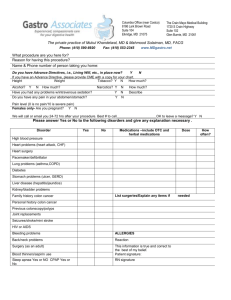
advertisement

Translational Molecular Genetics Harold Frucht, M.D. Division of Digestive and Liver Diseases Columbia University April 14, 2005 Cases with Familial Risk (~25%) Hereditary NonPolyposis Colorectal Cancer (3-5%) Familial Adenomatous Polyposis (<1%) Hamartomatous Polyposis Syndromes (<1%) Sporadic Cases (~70%) Disease-Associated Mutations Alter Protein Function Gene Mutations Somatic Mutation - Sporadic Cancer Germ Line Mutation - Inherited Syndrome Mechanisms of Cancer Gene Action M (mitosis) G1 (cell growth) Oncogenes: promote cell growth G2 S (synthesis) G0 (resting) Mismatch repair genes: correct replication errors Modifier genes: influence cell function Suppressor genes: inhibit cell cycle; promote apoptosis Calvert & Frucht, Ann Int Med, 2002;137:603-613 Somatic Mutation (Sporadic Disease) 2 normal copies of the gene in every cell One copy mutated in cell (1st hit is acquired) Second copy mutated in cell (2nd hit is also acquired) Calvert & Frucht, Ann Int Med, 2002;137:603-613 Germline Mutation (Inherited Disease) One copy mutated in every cell (1st hit is inherited) Second copy mutated in cell (2nd hit is acquired) Calvert & Frucht, Ann Int Med, 2002;137:603-613 Chung, DC. Gastroenterology 2000; 119: 854-865 CIMP = CpG Island Methylator Phenotype • epigenetic phenomenom • hypermethylation of the promoter region of the hMLH1 gene • responsible for MSI in 15% of sporadic colon cancers Polymorphism APC Gene I1307K Mutation Germline Mutation of Codon 1307 T-A Transversion (Leucine - Isoleucine Substitution) Causes hypermutability in adjacent sequences resulting in somatic alterations which predispose to colon cancer Incidence in Ashkenzai Jews 6.1 % Lifetime risk of colon cancer in people with mutation 18-30 % Non-Jewish population All Ashkenazi Jews 0% 6% Unselected Ashkenazi Jews w/ CRC 10% Ashkenazi Jews w/ CRC and family history of CRC 0% 28% 10% 20% 30% % with mutation Calvert & Frucht, Ann Int Med, 2002;137:603-613 Inherited Syndromes Predisposing to Colon Cancer Gene Lifetime Risk of CRC apc ~100% Hereditary Non-Polyposis Colon Cancer MMR >80% Peutz-Jeghers Syndrome STK11 2-13% Juvenile Polyposis SMAD4 ~<50% Cowden Syndrome PTEN small Familial Adenomatous Polyposis Correlations between the APC Genotype and the Clinical Phenotype NEJM 2003; 349:1750-1760 Clinical Criteria for Hereditary Non-Polyposis Colorectal Cancer Amsterdam criteria At least three relatives with colon cancer and all of the following: •One should be the first-degree relative of the other two •Two successive generations should be affected •At least one colon cancer should be diagnosed before the age of 50 •FAP should be excluded Modified Amsterdam criteria As for the Amsterdam criteria except that the cnacers need to be an HNPCCassociated cancer (colon, endometrium, small bowel, ureter, renal pelvis) instead of specifically colon cancer. Bethesda criteria Families meeting the Amsterdam criteria Individuals with 2 HNPCC-associated cancers, including synchronous or metachronous cancers Individuals with colon cancer and a first-degree relative with an HNPCCassociated cancer and/or colonic adenoma; 1 cancer diagnosed at age < 45 years and the adenoma diagnosed at age < 40 years Individuals with colon or endometrial cancer diagnosed at < 45 years Individuals with right-sided colon cancer having an undifferentiated pattern (solid/cribiform) or signet cell histopathology diagnosed at <45 years Individuals with adenomas diagnosed at < 40 years Calvert & Frucht, Ann Int Med, 2002;137:603-613 Autosomal Dominant Inheritance • Each child has 50% chance of inheriting the mutation • No “skipped generations” • Equally transmitted by men and women Normal Affected HNPCC: Direct Mutation Testing hMLH1 hMSH2 hMSH3 hPMS1 hMSH6 hPMS2 HEREDITARY COLON CANCER - Germline Mutation SPORADIC COLON CANCER - Somatic Mutation FAMILIAL COLON CANCER - Germline Mutation Causing Hypermutability and Subsequent Somatic Mutation Germline Mutations - Inherited Disease APC - Familial Polyposis Coli MMR - HNPCC (Lynch Syndrome) MYH- Familial Polyposis Coli Somatic Mutations - Sporadic Disease Oncogenes: myc, ras, src Tumor Suppressors: p53, DCC, APC, MCC Mismatch Repair Genes: MSH2, MSH3, MSH6, MLH1, PMS1, PMS2 “Genetic Polymorphisms” - Familial Disease APC - Familial Colon Cancer APC Gene Germline Mutation - Familial Polyposis Coli Somatic Mutation - Sporadic Colon Cancer I1307K Germline Mutation - Familial Colon Cancer GENETIC COUNSELING GENETIC TESTING Failure to Diagnose Hereditary Colorectal Cancer and Its Medicolegal Implications A Hereditary Nonpolyposis Colorectal Cancer Case Henry T. Lynch, M.D.,* Jane Paulson, J.D.,† Matthew Severin, J.D., Ph.D.,* Jane Lynch, B.S.N.,* Patrick Lynch, J.D., M.D.‡ From the *Department of Preventive Medicine, Creighton University School of Medicine, Omaha, Nebraska, †Paulson & Baisch, Portland, Oregon, and ‡Department of GI Oncology/Digestive Diseases, MD Anderson Cancer Center, Houston, Texas Diseases of the Colon & Rectum 1999: Jan 42(1); 31-35 The Use and Interpretation of Commercial APC Gene Testing for Familial Adenomatous Polyposis Francis M. Giardiello, M.D., Jill D. Brensinger, M.S., Gloria M. Petersen, Ph.D., Michael C. Luce, Ph.D., Linda M. Hylind, B.S., R.N., Judith A. Bacon, B.S., Susan V. Booker, B.A., Rodger D. Parker, Ph.D., and Stanley R. Hamilton, M.D. From the Departments of Medicine (F.M.G., J.D.B., L.M.H., J.A.B., S.V.B.) and Pathology (S.R.H.) and the Oncology Center (F.M.G., G.M.P., S.R.H.), John Hopkins University School of Medicine, Baltimore; the Departments of Epidemiology (G.M.P.) and Health Policy and Management (R.D.P.), John Hopkins University School of Hygiene and Public Health, Baltimore; and the Department of Molecular Biology, LabCorp, Research Triangle Park, N.C. (M.C.L.). Address reprint requests to Dr. Giardiello at Blalock 935, Johns Hopkins Hospital, 600 N. Wofe St., Baltimore, MD 21287-4461. Background The use of commercially available tests for genes linked to familial cancer has aroused concern about the impact of these tests on patients. Familial adenomatous polyposis is an autosomal dominant disease caused by a germ-line mutation of the adenomatous polyposis coli (APC ) gene that causes colorectal cancer if prophylactic colectomy is not performed. We evaluated the clinical use of commercial APC gene testing. Methods We assessed indications for APC gene testing, whether informed consent was obtained and genetic counseling was offered before testing, and the interpretation of the results through telephone interviews with physicians and genetic counselors in a nationwide sample of 177 patients from 125 families who underwent testing during 1995. Results Of the 177 patients tested, 83.0 percent had clinical features of familial adenomatous polyposis or were at risk for the disease — both valid indications for being tested. The appropriate strategy for presymptomatic testing was used in 79.4 percent (50 of 63 patients). Only 18.6 percent (33 of 177) received genetic counseling before the test, and only 16.9 percent (28 of 166) provided written informed consent. In 31.6 percent of the cases the physicians misinterpreted the test results. Among the patients with unconventional indications for testing, the rate of positive results was only 2.3 percent (1 of 44). Conclusions Patients who underwent genetic tests for familial adenomatous polyposis often received inadequate counseling and would have been given incorrectly interpreted results. Physicians should be prepared to offer genetic counseling if they order genetic tests. NEJM 1997; 336:823-27 Microsatellite Instability (MSI) • 10% - 15% of sporadic tumors have MSI • 95% of HNPCC tumors have MSI • Routine MSI assays soon available Normal Electrophoresis gel MSI tumor Genetic Testing Lab Methods Normal DNA Mutated Linkage Analysis: Probability of Inheritance. MSI Assays: Highly predictive for MMR mutation. Gene Sequencing: Approaches 100%. DGGE: Highly sensitive (>90%). SSCP: Detects 60%-95% of mutations. mRNA Protein Protein Truncation: Point of mutation dependent. Immunohistochemistry: Antibody dependent. Gel Calvert & Frucht, Ann Int Med, 2002;137:603-613 History Suggestive of Inherited Colon Cancer Probable FAP Probable HNPCC APC genetic test of an affected individual negative positive annual endoscopy APC gene testing of family members for all family members positive negative no adenomas annual endoscopy Genetic test of an affected individual annual endoscopy adenomas no adenomas prophylactic colectomy Colon Cancer screening as recommended for the general population positive negative HNPCC genetic testing of family members continued high risk colon cancer screening of the individual and all family members negative positive positive for colon cancer negative colectomy continued survellance for rectal adenomas and extra-colonic tumors. consider chemoprevention. Calvert & Frucht, Ann Int Med, 2002:137;603-613 FAMILY JW-39 11-17-94 60 heart disease 70’s BR, 70 70’s BR, 70 88 48 heart disease 32 85 60’s LU, 60 84 72 90 52 uBR, 54 CO, 72 53 50 EN, 45 29 EN, 42 27 25 CO, 26 ascending, Dukes, C Legend: = male; = female; = deceased; = proband Solid figures = cancer; BR = breast cancer; CO = colon cancer; LU = lung cancer; EN = endometrial cancer; number refers to age diagnosis Calvert & Frucht, Ann Int Med, 2002:137;603-613 FAMILY JW-37 9-7-94 70 77 75 CO, 59 EN, 76 68 RE, 68 67 73 73 65 CO, 39 BL, 66 BO, 73 CO, 39 CO, 64 46 49 CO, 37 27 21 90 65 60’s, 70’s EN, 65 47 12 Legend: = male; = female; = deceased; = proband Solid figures = cancer; CO = colon cancer; EN = Endometrial cancer; BL = Bladder cancer; BO = Bone cancer; RE = Rectal cancer; number refers to age diagnosis Calvert & Frucht, Ann Int Med, 2002:137;603-613 Incidence of Pancreatic Cancer by Number of Affected First Degree Relatives • 10% of patients with pancreatic cancer have a familial aggregation or an inherited predisposition Number of FDRs with Pancreatic Cancer Incidence (per 100,000) in the U.S. Population General U.S. (reference) 9 1 41 2 58 3 or more 288 Klein AP, et al., Cancer Research 2004; 64: 2634-2638 END OF PRESENTATION Clinical Features of Inherited Cancer Syndromes Feature FAP HNPCC Age of onset Early Early No. of adenomas > 100 < 10 Adenoma distribution Total Mainly right side Cancer distribution Random Mainly right side Other cancers Periampullary Endometrial, other Lynch HT et al, Clinical Risk Factors for Colorectal Cancer Cancer Family Syndromes Colon Endometrium Gastric Biliopancreatic Genitourinary Ovary Breast Sarcomas Skin Small Bowel Lung Other (63 %) (8/28 %) (6 %) (4 %) (2 %) (1/3 %) (2/6 %) (2 %) (2 %) (1 %) (1 %) (2 %) GENETIC TESTING FOR FAP 1. Linkage Analysis 2. In vitro truncated protein testing (transcription translation method) 3. Mutation Testing GENETIC TESTING FOR HNPCC 1. Linkage Analysis 2. Truncated Protein Testing 3. Mutation Testing 4. Microsatellite Instability Testing Clincial Cancer Screening Recommendations* Colon Cancer Screening Recommendations RISK SCREENING MODALITY AGE AT WHICH TO BEGIN FREQUENCY Average FOBT Sigmoidoscopy FOBT and Sigmoidoscopy DCBE Colonoscopy 50 50 50 50 50 annually every 5 years every 5 years every 5-10 years every 10 years First-degree relative with colon cancer or adenomatous polyp at age 60 years Same as for average risk individuals 40 same as for average risk individuals Two or more first-degree relatives with colon cancer or adenomatous polyp at age < 60 years Colonoscopy preferred FAP Sigmoidoscopy HNPCC Colonoscopy 40 or 10 years younger than the earlier diagnosis 10-12 years 20-25 years or 10 years younger than the earliest colon cancer diagnosis every 3-5 years annually every 1-2 years Extracolonic Cancer Screening Recommendations FAP: Duodenal cancer EGD 20-25 years every 1-3 years HNPCC: Endometrial and ovarian cancer Pelvic exam Trans vaginal ultrasound 25-35 years every 1-2 years Gastric cancer EGD 30-35 years every 1-2 yeas *DCBE = double contrast barium enema; EGD = esophagogastroduodenoscopy; FOBT = fecal occult blood test. Columbia Colon Cancer Prevention Program (C3P2) History and Physical Risk Assessment Screening Guidelines Genetic Counseling and Testing Chemoprevention