Introduction to Pediatric Nursing
advertisement

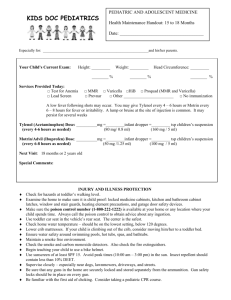
INTRODUCTION TO CHILD HEALTH NURSING WHO IS YOUR PATIENT? 6 year old female admitted to the hospital with a medical diagnosis of pneumonia Currently in 1st grade Lives at home with Mother, Father, and 2 year old sibling Both parents work full time outside the home Grandparents live in near by town and assist with child care ANSWER: PEDIATRIC NURSING A parent-nurse partnership Nurse’s goals are to promote therapeutic relationship between parent and child continued growth and development GROWTH AND DEVELOPMENT DEFINITIONS OF GROWTH AND DEVELOPMENT Growth Increase in physical size of a whole or any of its parts Increase in number and size of cells Growth can be measured Development A continuous, orderly series of conditions leads to activities and patterns of behavior PACE OF GROWTH A rapid pace from birth to 1 ½-2 years A slower pace from 2 years to puberty Expected 4-6 lb/year A rapid pace from puberty to approximately 15 years A sharp decline from 16 years to approximately 24 years when full adult size is reached STAGES OF GROWTH AND DEVELOPMENT Neonate first 28 days of life Infancy birth to 12 months Toddler 1 to 3 years Preschooler 4 to 5 years School-ager 6 to 10 years Prepubertal 11 to 12 years Adolescent 13 to 18 + years DEVELOPMENT PSYCHOSOCIAL & INTELLECTUAL THEORISTS ASSOCIATED WITH DEVELOPMENT Piaget Stages of cognitive development Erikson Stages of psychosocial development Kohlberg Stages of moral development Freud Stages of psychosexual development PSYCHOSOCIAL DEVELOPMENT Trust vs. Mistrust (birth to 1 year) Establishes a sense of trust when basic needs are Nurses should provide consistent, loving care Autonomy vs. Shame & Doubt: (1-3 yrs) Increasingly independent in many spheres of life Nurses should allow for choices and self care PSYCHOSOCIAL DEVELOPMENT Initiative vs. Guilt (3-6 yrs) Learns to initiate play activities, imitate adult behavior Nurses should encourage to explore environment with senses, promote imagination Industry vs. Inferiority (6-12 yrs) Learns self worth as workers & producers Nurses should promote children to compete and cooperate PSYCHOSOCIAL DEVELOPMENT Identity vs. Role Confusion (12-18 yrs) Forms identity and establishment of autonomy from parents Peers and society big influence Nurses should encourage peer visitation, texting, phone calls INTELLECTUAL DEVELOPMENT Sensorimotor (birth to 2) Learns from movement and sensory input Learns cause & effect Preoperational (2 to 7 years) Increasing curiosity and explorative behavior Thinking is concrete Egocentrism is dominant INTELLECTUAL DEVELOPMENT Concrete Operational (7 to 11 years) Logical & coherent thought Can now distinguish fact from fantasy Formal Operations (11 to adulthood) Acquisition of abstract reasoning leading to Analytical thinking Problem solving Planning for the future FACTORS INFLUENCING GROWTH AND DEVELOPMENT Genetics Environment Culture Nutrition Health status Family Parental attitudes Child-rearing philosophies PLAY PURPOSE OF PLAY Sensorimotor development Intellectual development Socialization Creativity Self-awareness Moral value Therapeutic value TYPES OF PLAY Solitary Parallel Associative Cooperative Onlooker Dramatic Familiarization COMMUNICATING WITH CHILDREN INFANCY Responds to physical contact Use a gentle voice Sing-song quality High pitched Need to be held, cuddled EARLY CHILDHOOD < 7 YRS Remember they are egocentric and interpret words literally Tell them what “children” can do Let them touch equipment Nonverbal messages should be clear Maintain eye level Use quiet, calm voice Be specific, use simple words, short sentences, be honest SCHOOL AGE Wants to know why an object exists How it works Why it is being done to them Concerned about body integrity ADOLESCENTS Needs undivided attention o Listen, be open-minded o Avoid criticizing o Make expectations clear o PHYSICAL & DEVELOPMENTAL ASSESSMENT PHYSICAL EXAM GUIDELINES Non-threatening environment Place frightening equipment out of sight Provide privacy Provide time for play (stuffed animals, dolls) Observe for behaviors re: child’s readiness to cooperate Begin with the least intrusive examination (observation) AGE-SPECIFIC APPROACHES TO EXAM Infant: auscultate heart, lungs first (head to toe NOT always appropriate) Toddler: inspect body area through play, introduce equipment slowly Preschool: if cooperative: proceed head to toe, if not: same as toddler School-age and Adolescents: head to toe, genitalia last, respect privacy PEDIATRIC PHYSICAL EXAM Growth measurements Height, weight, head circumference (<3 yrs) Physiologic measurements (VS) General appearance (hygiene, posture, behavior) Body Systems (heart, lungs, abdomen are key areas) DENVER DEVELOPMENTAL SCREENING TEST (DDST-II) Evaluates development for children 0-6 in four areas Personal-social Fine-motor Language Gross motor Child’s mood must be typical for results to be valid Results may be altered if child is not feeling well, sedated DENVER DEVELOPMENTAL SCREENING TEST (DDST-II) Provides a clinical impression on child’s overall development Not a predictor of future development, not an IQ test Used for noting problems, monitoring, and to base a referral for additional developmental testing NURSING INTERVENTIONS BASED ON DEVELOPMENTAL AGE (NOT CHRONOLOGICAL AGE) Infants (0-12m) Use soft voice, sing-song, Talk to and describe procedures as they are done Toddlers (1-3 yr) Separation anxiety peaks (nurse is a stranger) Preparation for a procedure should begin immediately before the event NURSING INTERVENTIONS BASED ON DEVELOPMENTAL AGE (NOT CHRONOLOGICAL AGE) Preschool (4-5 yr) Explain procedures according to senses (what child will feel, see, hear) Imagination is active...may see procedures as a consequence for misbehavior School-age (6-10 yr) Use books, pictures to explain procedures Developmentally ready for detailed explanations Organizing and collecting is an enjoyed activity Peers become more important, parents still main influence NURSING INTERVENTIONS BASED ON DEVELOPMENTAL AGE (NOT CHRONOLOGICAL AGE) Pre-Adolescents/Adolescents (11 & up) Value privacy, group identification is important May have an need for independence Older adolescent can understand adult concepts Can be prepared for a procedure up to a week in advance DISCIPLINE (LIMIT SETTING) Reinforcement of desired behaviors is most effective Consequences for negative behaviors Teaching parents how to discipline avoids problems related to incorrect use Appropriate limit setting Consistency Consequences should be told in advance Include truthful explanation of why behavior is unacceptable Physical punishment is the least effective LIMIT SETTING AND THE TODDLER Discipline must be consistent, immediate, realistic, age-appropriate, and related to the incident Clearly explain limits and give time for toddlers to respond Avoid arguments and extensive explanations Avoid withdrawing love as punishment Separate toddler from behavior Praise toddler for good behavior NUTRITION INFANCY 0-6 MONTHS Breastmilk most desirable Fe fortified formula alternative No whole milk until 1 year old Altered ability to be digested Increased risk of contamination Lack of components needed for appropriate growth INFANCY 6-12 MONTHS Breast milk or formula remains the primary source of nutrition May begin addition of solids b/c: GI tract is mature to handle complex nutrients GI tract is less sensitive to allergenic foods Extrusion reflex has disappeared Swallowing is more coordinated Head control is well developed, voluntary grasping begins INFANCY 6-12 MONTHS 4- 6 months infant cereal mixed with formula or Breast milk (Rice, then oatmeal, barley) 6 months can introduce crackers as a teething food. 6 months fruit juice to substitute for one milk feeding Baby food (pureed fruits and vegetables) Introduce one food at a time at 4-7 day intervals No strawberries, eggs, peanuts until after 12 months of age INFANCY 0-6 MONTHS No solids before 4-6 months of age b/c: Solids are not compatible with GI tract Exposure to food antigens that may produce a food-protein allergy Extrusion reflex still present (pushes food out of mouth) INFANCY 6-12 MONTHS By 8-9 months junior foods & finger foods By 1-year well-cooked table foods TODDLERHOOD From 12-18 months rate of growth slows At 18 months decreased nutritional need, appetite declines, picky eaters At 18 months may be able to adeptly use spoon, prefer fingers Do not force food TODDLERHOOD Mealtime should be pleasant What is eaten is more important than how much is eaten General serving size is ¼ to 1/3 of the adult portion May have a hard time sitting through an entire meal PRESCHOOL Needs are similar to toddler Average More daily intake: 1800 calories agreeable to try new foods Ready to socialize during meals General serving size is ½ of an adult’s portion SCHOOL AGE YEARS Food likes and dislikes are established Important for parents to choose foods that promotes growth Children eat away from home Important to teach Food Pyramid Guide for nutrition instruction Encourage the child to make good choices ADOLESCENCE Caloric and protein requirements are higher than almost any time in life Eating habits easily influenced by peers Fad diets, high caloric foods low in nutritional value popular CARE OF THE HOSPITALIZED CHILD “ATRAUMATIC CARE” Interventions that eliminate or minimize psychological and physical distress experienced by children and their families in the health care system STRESSORS OF HOSPITALIZATION Separation Anxiety Loss of Control Bodily Injury & Pain STAGES OF SEPARATION ANXIETY (Universal fear of toddler) Protest Despair loud, demanding cries, rejects comfort measures lies on abdomen, flat facial expression, weight loss, insomnia, loss of developmental skills Denial or Detachment silent expressionless child, deterioration of developmental milestones, may have trouble forming close relationships NURSING INTERVENTIONS Limit admissions Limit hospital stay Reduce pain Adequately prepare child for procedures Open visiting (include siblings) Primary nursing Use of play Hospital bed = “safe area” Increase control LOSS OF CONTROL Children loose control over their Routine Body Basic decisions Loss of school, boredom Ability to socialize INTERVENTIONS Infants Provide consistent care Toddlers Maintain consistent routine Encourage brining security objects (stuffed anima)l that help them feel safe and secure Preschoolers Need adequate preparation to unfamiliar experiences Fear bodily injury School-age, pre-adolescent and adolescents Provide schoolwork, social time, privacy INTERVENTIONS: PLAY! Provides diversion, brings about relaxation Helps child feel more secure in strange environment Helps lessen stress of separation Means for release of tension & fears Means for accomplishing therapeutic goals Allows making choices & being in control BODILY INJURY Procedures are uncomfortable Disease processes are painful Postoperative pain can be very severe ASSESS FOR PAIN Infants and Toddlers Grimace, clench teeth, restless Preschoolers Can locate pain, use face scale Fear bodily injury & mutilation School-age Fear disability & death Pain is seen as punishment “Magical quality” of germs Can use faces scale Adolescents Use same pain scale as adults PEDIATRIC PAIN ASSESSMENT “Pain is whatever the child experiencing it says it is”. CHILDREN ARE UNDER-MEDICATED BECAUSE OF THESE MYTHS: o infants don’t feel pain o children tolerate pain better than adults o children cannot tell you where it hurts o children always tell the truth about pain o children become accustomed to painful procedures o parents do not want to be involved in child’s pain control INTERVENTIONS Nurses have an ethical obligation to relieve a child’s suffering Adequate pain relief leads to earlier mobilization shortened hospital stays reduced costs ASSESS THE CHILD USING QUESTT: Question the child Use pain rating scales Evaluate behavior & physiologic changes Secure the parents’ involvement Take into consideration: cause of pain Take action & evaluate results INTERVENTIONS Medicate for Pain Non Pharmacological Therapy Cutaneous Stimulation Distraction Guided Imagery Hot or Cold application Relaxation HOSPITALIZATION FOR ALL PEDIATRIC PATIENTS 1. 2. 3. 4. Child will be prepared Child will experience little or no separation Child will maintain sense of control Child will exhibit decreased fear of bodily injury PRACTICE QUESTIONS! The nurse is administering the Denver Developmental Screening test to an infant. The mother expresses concern that her baby is “not doing well”. Which response is most appropriate for the nurse to make? 1. Why are you so worried? Have you been having problems at home too? 2. Please let me finish this test before you start worrying, Maybe the baby will do better on the rest of the test 3. You really sound worried. Please keep in mind that no baby is expected to do all the things on this test 4. Unfortunately, your concerns seem to be valid. I will write up a consult with the child development specialist The RN observes a nursing student entering a toddler’s room to check vital signs and begins to take the child’s BP first. The RN should: 1. 2. 3. 4. Say nothing, this action is appropriate Suggest the student start with the pulse Suggest the student start with the temperature Suggest the student start with respirations The nurse teaches parents of a 4-year-old about the best way to assist their child in completing the core developmental task of the preschooler by: 1. Encouraging the child to remove and put on own clothes 2. Knocking on door before entering the child’s bedroom 3. Planning for playtime and offer a variety of materials from which to choose 4. Singing, rocking, and holding the child consistently A toddler who is to be hospitalized brings a dirty, ragged Elmo stuffed animal with him. The nurse’s most appropriate action is: 1. Ask the toddler’s parents to find an identical new Elmo stuffed animal 2. Allow the toddler to keep the Elmo stuffed animal 3. Remove Elmo while the child is sleeping and tell the child when he wakes that Elmo is lost 4. Distract the toddler by taking him to the The mother of a preschooler expresses disappointment when her child’s weight has increased “only” 4 pounds since the child’s physical 1 year ago. The nurse should advise this mother that: 1. A weight gain of 4-6 pounds/year is normal for a preschooler 2. The poor weight gain may be a result of poor nutrition 3. The poor weight gain may indicate a more serious problem 4. The weight gain is not ideal but may be nothing to worry about The nurse should suggest the best way for a toddler’s parents to assist their child to complete the core developmental task of the toddler years is to: 1. Allow the toddler to make simple decisions 2. Allow the toddler to “help” with chores 3. Assign the toddler simple tasks or errands The nurse is preparing to change a toddler’s wound for the first time. Prior to the dressing change the nurse uses a gauze as a “blanket” for the child’s action figure. This is known as: 1. Dramatic play 2. Familiarization 3. Cooperative play 4. Onlooker actions A mother of a toddler is frustrated and states “ I can’t get this child to eat!”. The nurse should help by reviewing the portion size for toddlers is _____ of an adult’s portion. 1. ¼ 2. 2/3 3. 4. ½ ¾