Personal Protection
advertisement

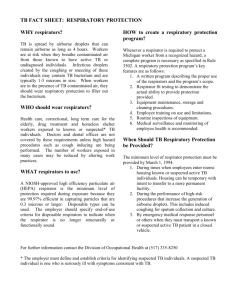
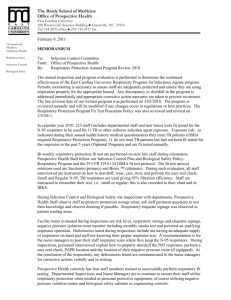
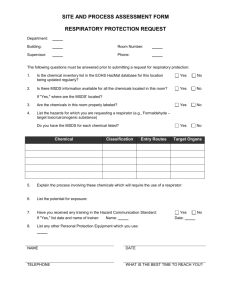
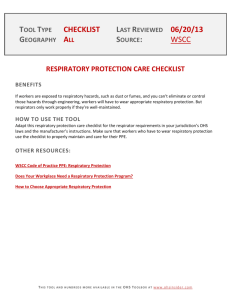
“Respiratory Protection for Public Health Workers” Infectious Diseases Division Public Health Initiatives Branch Department of Public Health State of Connecticut Acknowledgement This presentation is a revision of a training prepared by Anne Bracker, MPH, CIH University of Connecticut Health Center Division of Occupational and Environmental Medicine Farmington, CT Learning Objectives • Describe respiratory hazards and prevention methods • Describe key types of respirators, their indications, and limitations • Describe proper methods of donning, discarding, and storing N 95 masks • Identify three key steps in the ID Section Respiratory Protection plan • List the steps in the fit testing procedure Pathogen transmission routes: ID Section employee exposures Person- toPerson transmission Routes Aerosol anthrax smallpox √ √ √ √ ? √ √ √ √ √ √ ? √ √ √ √ √ √ √ Respiratory droplets Fomites √ Environmental surfaces √ plague Food/ water Blood/ Fecal/ Urine Respiratory Protection influenza √ tularemia √ √ SARS botulism TB VHF √ √ Control • What is the pathogen, source? • What is the route of exposure? • How can the exposure pathway be interrupted? Respiratory transmission: What is the route of exposure? • Direct contact with mucous membranes • Inhalation if aerosolized How can the pathways be interrupted • • • • • Isolate or remove the source Minimize the opportunities for transmission Observe good hygiene Make the unexposed individuals less vulnerable Wear protective equipment Isolate the sourceinfected people (if person to person) • Isolation- separate the ill in health care facilities with isolation rooms (community screening: temperature and symptom monitoring) • Cough Etiquette – Cover the nose/mouth when coughing or sneezing. Use tissues to contain respiratory secretions. Dispose of tissues in the nearest waste receptacle after use. Perform hand hygiene after contact with respiratory secretions and contaminated objects/materials. During transport- use surgical masks or respirators without exhalation valves. Minimize the opportunities for transmission • Physical separation - separate presumed exposed (and possibly infectious) from unexposed – Talk over the phone – Talk through the door Make the Unexposed Population Less Vulnerable • Vaccines – Availability and distribution – Effectiveness – Supply – Rely on more than one method of protection Observe good hygiene Hand hygiene Avoid touching contaminated surfaces Routinely clean contaminated surfaces Infection Control Precautions • Standard • Transmission-based –contact –droplet –aerosol Respiratory Protection • Purpose – protect from inhalation of infectious aerosols (e.g., Mycobacterium tuberculosis), droplet nuclei • PPE types for respiratory protection – Particulate respirators – Half- or full-face elastomeric respirators – Powered air purifying respirators (PAPR) CDC: PPE Use in Healthcare Settings Respirator type selection Atmosphere Supplying Air purifying • Tight or loose fitting • Clean the air- filters or chemical cartridges • Different protection factors • Not for certain environments: Robert Swanson www.internet-esq.com – Immediately Dangerous to Life and Health (IDLH), – O2 deficient, or – Other hazardous agents The N95 Respirator N: 95: • • • • not resistant to oil 95% efficient for 0.3 micron particles Filter penetration Protection factor Fit testing Re-use/Reaerosolization Rengasamy et al (2004) AJIC Surgical masks are not respirators appropriate for cough etiquette & protection from respiratory droplets (not aerosols) N95 respirator features: Which N95 respirators will you select? • Exhalation valves • Latex free, or not • Nose Clips • Prior successful fit How to Don a Particulate Respirator • • • • • • Select a fit tested respirator Place over nose, mouth and chin Fit flexible nose piece over nose bridge Secure on head with elastic Adjust to fit Perform a fit check – – Inhale – respirator should collapse – Exhale – check for leakage around face PPE Use in Healthcare Settings Removing a Particulate Respirator • Lift the bottom elastic over your head first • Then lift off the top elastic • Don’t touch the mask filter • Discard PPE Use in Healthcare Settings Where to Remove PPE • Gowns, gloves at doorway, before leaving patient room or in anteroom* • Remove respirator outside room, after door has been closed* * Ensure that hand hygiene facilities are available at the point needed, e.g., sink or alcohol-based hand rub CDC: PPE Use in Healthcare Settings Hand Hygiene • Perform hand hygiene immediately after removing PPE. – If hands become visibly contaminated during PPE removal, wash hands before continuing to remove PPE • Wash hands with soap and water or use an alcohol-based hand rub * Ensure that hand hygiene facilities are available at the point needed, e.g., sink or alcohol-based hand rub CDC: PPE Use in Healthcare Settings Problems while wearing: Words of Wisdom To avoid exposure to the pathogen, adjust or change respirator outside the area of possible exposure Medical signs and symptoms that limit or prevent respirator use • • • • • Wheezing Shortness of breath Dizziness Chest pain Discomfort wearing the respirator The most important point! If the risk agent (the pathogen) is unknown or you do not know whether the N95 protects, do NOT enter the area! Respiratory Protection (OSHA:1910.134) • Written Respiratory Protection Program elements; – – • • • • • • • Hazard analysis Selection Medical Evaluation Fit Testing Use Maintenance Training Evaluation Recordkeeping Written Respirator Program Purpose and Scope • Purpose - ensure that all health department employees are protected from person-to-person transmission of infectious inhalational agents • Covers employees identified as having risk in the plans Hazard Assessment (first step in the plan) How to get a copy of the plan • Accessible via: – U drive – Respiratory Program Administrator (Rich Melchreit for ID Section) Hazard assessment • Assessment/hazard analysis – Part of the respiratory protection plan • Anticipated employee risk during routine work and emergencies • Identifies which employees should be issued respiratory protection – Out in the field • Employee anticipates risk – Unknown hazards, and avoid the location, or – Need to don the respirator Medical Evaluations (before respirator use or fit testing) • Employee completes mandatory medical evaluation questionnaire • Questionnaire is reviewed by a Physician or Licensed Health Care Provider (PLHCP) at UCHC to determine the employee’s ability to wear the N95 respirator • The PLHCP completes a clearance review form and sends copies to DPH and employee Training • Respiratory hazards • Respirators: – choice – proper use: • donning • removing – limitations on their use • Maintenance Fit Testing (annual) and Use • Qualitative or Quantitative Methods • Features which compromise fit Beard growth Improper donning Humidity, Sweat Work Practices Facial disfigurement Eye glasses Excessive weight gain or loss Failure to complete a fit check Other considerations: • Should/could/would the N 95s be reused? • Not likely unless in short supply • If so, likely advice will be to cover them with a surgical mask • How should I store my personal respirators ? – Rigid tub – Zip lock plastic bag (temporarily) with air holes – Label with your name • Discard after use? – Discard in medical waste or sealed in plastic bag (no holes) in trash Program Evaluation and Record Keeping • Kept at UCHC – Medical evaluations • Kept at DPH – Plan (U drive/Branch Office Folder - Public Health Initiatives/Fit Testing Program/fit testing written program dph 02-02-09.doc, and with the RPA) – Employee tracking spreadsheet – TRAINing data – Fit testing evaluations • Kept by staff person – Laminated wallet cards Fit Testing protocol: • Very specific protocol and instructions • Sensitivity – Equipment • Hood • Sprayer – Taste test (saccharin or bitrex® for N95) • Fit test proper – Choose mask – Don mask (while wearing eyeglasses or anticipated “protective ware”) and check for coverage and user comfort – Don hood – Spray of test solution, check for taste – Go through the “paces” • Heavy breathing • Move head • Talk