MCRTP Responsible Conduct of Research
advertisement

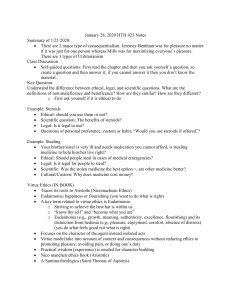
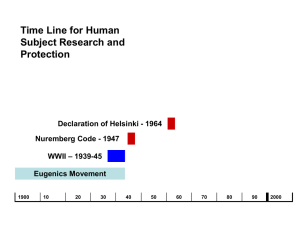
MCRTP Responsible Conduct of Research GENETICS AND HUMAN REPRODUCTION DR. BEN A. RICH PROF. LISA IKEMOTO Approach Review - history of biomedical ethics Discuss Review – history and practice of eugenics in the U.S. Discuss Case studies History of Biomedical Ethics Historical antecedents e.g. Hippocrates 19th century: development of clinical research Breakthroughs and abuses Early 20th century Observation to intervention Increase in private funding WWII Research as part of the war effort Federal funding History of Biomedical Ethics Key events Nazi War Crimes Trials: the Nazi Doctors and the Nuremberg Code Thalidomide (1957-1962) The Beecher article (1966) Jewish Chronic Disease Hospital (1963) and Willowbrook (1956-1971) Tuskegee (1932-1972) History of Biomedical Ethics Regulation of biomedical research Nuremberg Code (1946) Kefauver-Harris Amendments to the FDCA of 1938 (1962) National Research Act of 1974 >> Belmont Report (1979) >> Federal Regulation of Human Subject Research Federal Common Rule (1991) The Belmont Report (1979) Part A: Boundaries Between Practice & Research Part B: Basic Ethical Principles 1. Respect for Persons 2. Beneficence 3. Justice Belmont Report: Ethical Principles and Applications 1) Respect for persons Application: Informed Consent 2) Beneficence Application: Assessment of Risks and Benefits 3) Justice Application: Selection of Subjects History: Other Key Events – 1970s Roe v. Wade (U.S. 1973) – woman’s right to decide whether or not to terminate a pregnancy. In re Quinlan (N.J. 1976) – right to refuse treatment (ventilator) Birth of Louise Brown, 1978 – first child born as a result of IVF. Core Bioethical Principles . . . The “Georgetown Mantra” respect for individual autonomy beneficence nonmaleficence justice Benefit and harm Value-laden concepts Whose perspective? Core Principles … Respect for individual autonomy Etymological roots: self-rule Premised on dignity and moral worth of each person qua person Not a traditional core value of medicine Constitutional dimension – substantive due process (privacy as “the right to be let alone”) Underlying moral principle more aptly captured by term “authenticity” when patient lacks decisional capacity Balanced in so-called “right to die” litigation by “countervailing interests of the state” … Core Principles Beneficence/nonmaleficence Deep roots in Hippocratic medicine Primum non nocere (first do no harm) Critical moral question: who shall be the final arbiter of what constitutes benefit and harm? Query: Is life-sustaining treatment always beneficial? Is allowing a patient to die always harmful? – concept of a “medical fate worse than death” Tradition of medical paternalism presupposed that physician determined patient benefit and harm Hard vs. soft paternalism Alternative Ethical Approaches Virtue Ethics Roots in classical Greek philosophy Focus on character traits, e.g., integrity, honesty, fidelity, generosity, compassion Virtuous person not only acts morally, but does so out of authentic moral motivation and not to avoid sanction Ethics of Care Response to emotional detachment of traditional theories Particularly pertinent to bioethical analysis Casuistry Reliance on paradigm cases and precedent Application of principles to cases with discernment Elements of Sound Ethical Analysis Gather relevant data discussions with involved parties examination of medical records & other documentation review organizational policy/guidelines Clarify relevant concepts confidentiality, privacy, informed consent Clarify related normative issues societal values legal provisions (case law, statutes, etc.) Identify range of morally acceptable options Analytic Matrix Medical Indications Does the proposed measure/intervention fulfill any goal of health care? What is the likelihood of its success Quality of Life Describe from patient’s perspective Other qualitative considerations from patient’s perspective Patient Preferences Expressed in terms of goals, values, priorities Consistency of wishes with core values Indications of decisional capacity Contextual Features Social, economic, and institutional features, e.g., inability to cover cost of measures; inadequate social support Legal, regulatory, policy constraints/requirements An Ethics Workup Clearly and concisely state issue or issues Ascertain the legitimate decision makers (stakeholders) Describe pertinent facts – medical, psychosocial, situational, institutional Identify relevant interests – patient, family, professional, institutional – and their interrelationships Delineate the range of options for action Facilitate discussion among all parties in interest in pursuit of consensus Determine risks and benefits of acting without consensus if the dispute proves intractable Formulate and follow a process for acting without consensus that accurately reflects the basis for doing so History of Eugenics in the U.S. Francis Galton & Co. founded the eugenics movement >> Western Europe and U.S. Early 20th Century: Involuntary sterilization laws Race & ethnicity-based immigration restrictions Examples: Buck v. Bell (1927) Skinner v. Oklahoma (1942)