Pathophysiology
advertisement

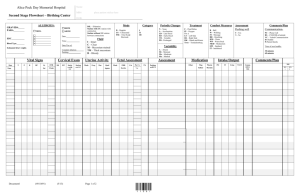
Legaspi, Luis Ontok, Abdul-Aziz Payumo, Edelissa Pelayo, May Angela Rodriguez, Melissa Samson, Edgardo Baby Boy J.C. • Full Term, 37 weeks by P.A. • 2600 g, appropriate for G.A. • Cephalic presentation • Repeat low-segment C.S. • 23 year old, G2P2 • • • OB Index: G2P2 (2002) Previous Pregnancy: Date: 2007 Sex: Male BW: 2.7 kg Place: Perpetual Help Hospital Delivery Type: 1o Low-segment C.S. AOG: Full Term Complications: Cephalopelvic Disroportion • LMP: September 04, 2008 • Prenatal Checkups: 2 at PGH • Medications Taken: None • Illnesses/Infection: None • Alcohol/Tobacco Use: None • Onset of Uterine Activity: Spontaneous • Intensity of Contractions: Moderate • Membrane Status: Intact • Analgesia: None • Mode: Abdominal • Amniotic Fluid: Slightly Meconium Stained • Analgesia: Subarachnoid Block (+) grimace, HR 50’s, acrocyanotic, some flexion • Thermoregulation • Suctioning • Tactile stimulation • Thermoregulation • Suctioning • Tactile stimulation • PPV Some flexion, HR 100, (+) grunting, (+) grimace, acrocyanotic (+) crying, acrocyanotic, active, HR 130s, RR 50-60 • Given blow by O2 • Stimulation • Thermoregulation • Weaned off from O2 (+) grunting, (+ retractions • • APGAR Score: 5, 9 Resuscitation: Supplementary O2 10 LPM via hood Positive Pressure-Ventilation • (-) Hypertension • (-) Diabetes Mellitus • (-) Bronchial Asthma • (-) Blood Dyscrasias • GENERAL APPEARANCE: limp, in respiratory distress • VITAL SIGNS: T: 36.6oC HR: 130 bpm RR: 50 cpm Wt: 2600 g Lt: 49 cm HC: 32.5 cm CC: 31 cm AC: 28 cm • SKIN: acrocyanotic, (-) lesions, (+) cracking, rare veins • HEAD: (-) molding, (-) cephalhematoma, both fontanels flat and soft, (-) overlapping sutures, BT: 8cm, BP: 9cm, SOB: 9cm, OF: 10.5cm, OM: 11.5cm • EYES: (-) discharges, anicteric sclerae, both pupils equally reactive to light • EARS: (-) low-set ears, formed, firm with instant recoil • MOUTH: (-) circumoral cyanosis, (-) cleft lip, formed tongue, (-) cleft palate • CHEST/LUNGS: barrel-shaped, (+) subcostal & intercostal retractions, raised areola with 3-4 mm bud, (+) grunting, (-) tachypnea • HEART: adynamic precordium, (-) thrills, normal rate, regular rhythm, (-) murmur • ABDOMEN: globular but not distended, nonpalpable liver • UMBILICUS: translucent, (-) meconium stained, 2 arteries & 1 vein • BACK: lanugo with bald areas, (-) dimpling, straight spine • GENITALIA: both testes descended, scrotum with good rugae • ANUS: patent, (+) passage of meconium • EXTREMITIES: (-) polydactyly, (-) hip dislocation, plantar crease over anterior 2/3, equally strong & palpable pulses • NEUROLOGIC EXAM: (+) moro reflex, (+) sucking reflex, (+) grasping reflex • Meconium Pneumonitis • Full term 37 weeks by PA 2600 grams AGA cephalic presentation delivered by repeat LSCS, AS 5,9 (+) history of meconium staining baby received non-vigorous, HR 60s, poor muscle tone, with no response (+) tachypnea (+) grunting (+) retractions Differential Rule-in Rule-out Hyaline Membrane Disease (+)tachypnea (+) grunting (+)retractions -rare in term neonates -mother not GDM -worsens / peaks at 48-36 hours Transient Tachypnea of the Newborn -usually follows uneventful normal FT SVD or cesarean section -cyanosis relieved by minimal 02 -with rapid recovery in 3 days -PE: lungs clear w/o rales or rhonchi -benign, self-limited course -Early onset tachypnea with or without retractions (+) expiratory grunting Neonatal Pneumonia (+)tachypnea (+) grunting (+)retractions (+) cyanosis Pre-natal history suggests infection -usually predisposed by pre-mature labor, PROM, increased IE -CBC usually: neutropenia, leukocytosis -cannot be fully ruled-out Meconium Aspiration Syndrome (+) history of meconium staining -baby received nonvigorous, HR 60s, poor muscle tone, with no response (+)tachypnea (+) grunting (+)retractions -cannot be fully ruledout Neonatal Sepsis Respiratory distress Cannot be fully ruled • Born at PGH Nursery on May 7, 2009 with APGAR score 5, 9 • Started on Piperacillin-Tazobactam (75mkd) 195 mg IV q12 Started on Amikacin (15mkd) 40 mg IV OD • Piptazo Combination antibiotic containing the extendedspectrum penicillin and the B-lactamase inhibitor tazobactam Amik An aminoglycoside With synergistic effect with Blactams • Labs: • CBC with PC • Blood typing • ABG • • • Na, K, Cl, Ca, CXR APL Blood C/S Venoclysis started with D10W (80) @ 9cc/hr NPO, Hgt q8 O2 support at 10 lpm/hood NICU • Admitted at NICU 3 on May 7, 2009 • Received with fair pulses BP 30-40/20’s • Given total of 50 cc/kg PNSS IV bolus, BP improved to 40-50/30’s but still with fair pulses • Started on Dopamine @ 10mcg/kg/min to run for 1cc/hour (Dopamine 0.9cc + D5W 23.1cc) • UVC inserted 50 cc/kg PNSS IV bolus To increase BP Dopamine @ 10mcg/kg/min Maintenance bp to run for 1cc/hour (Dopamine 0.9cc + D5W 23.1cc) • • • • • Due to persistent desaturation (O2 sats 80’s), patient intubated with MV settings 100%, 18/3, RR 60 LT 0.4 O2 sats improved to 98-100% ABGs ordered D10W increased to run for 10 cc/hour STAT NaHCO3 5 meqs given NaHCO3 5 meqs To counteract metabolic acidosis MV settings 100%, 18/3, RR 60 ? LT 0.4 05/07/09 hood 23:10 100% O2 pH 7.189 pCO2 51.20 pO2 76.00 HCO3 19.80 BEb -8.2 O2sat 91.40% Respiratory Acidosis Decrease Ventilation Hypoxemia ABG 05/08/09 0.4 00:18 S/P INTUBATION 100% 18/3 pH 7.252 pCO2 39.70 N pO2 188.00 HCO3 17.70 BEb -8.5 O2sat 99.50% Metabolic Acidosis NaHCO3 5 meqs 60 ABG 05/08/09 60 0.4 06:51 AFTER CORRECTION 100% pH 7.407 N pCO2 28.00 pO2 146.00 HCO3 17.80 BEb -5 O2sat 99.30% 18/3 Component 05/07/09 Reference Range Unit WBC 5.56 5.0 – 30.0 X109/L RBC 3.74 4.0 – 6.0 X1012/L HGB 129 120-180 g/L HCT 0.386 0.370 – 0.540 MCV 103.2 80.0 – 100.0 Fl MCH 34.5 27.0 – 31.0 Pg MCHC 334 320 – 360 g/L RDW 17.2 11.0 – 16.0 % Platelet 227 150 – 450 X109/L NRBC 2/100 Complete Blood Count Component 05/07/09 Reference Range Unit Neutrophil 0.697 0.500 – 0.700 % Lymphocyte 0.182 0.200 – 0.500 % Monocyte 0.101 0.020 – 0.090 % Eosinophil 0.016 0.000 – 0.060 % Basophils 0.004 0.000 – 0.020 % Stab Metamyelocyt e Myelocyte Promyelocyte Blast Atypical Lymphocyte % Test 05/09/09 05/12/09 Units Normal Values Calcium 1.60 1.92 mmol/L 2.12 – 2.52 Sodium 143 140 mmol/L 136.00 – 145.00 Potassiu m 3.9 4.3 mmol/L 3.50 – 5.10 Chloride 108 106 mmol/L 98.00 – 107.00 • PWI: FT 37 weeks PA, 2600g, AGA, ceph, repeat LSCS, LBB, AS 5,9; Neonatal Pneumonia vs MAS; PPHN precaution r/o sepsis • MV settings maintained • IVF shifted to D10IMB Ca 300 @ 10cc/hr D10IMB Ca 300 @ 10cc/hr To correct hypocalcemia • Decrease RR to 50 then decrease by 2 q2 until 30 • Decrease FiO2 by 5 q2 until 60% ABG 05/08/09 17:00 100% 18/3 pH 7.468 pCO2 14.40 pO2 191.00 HCO3 10.50 BEb -9.8 O2sat 99.80% 60 0.4 Dec. RR to 50 then dec by 2 O2 til 30 Dec.. FiO2 by 5 O2 til 60% Pneumonia, both inner lung zones • MV setting at 80%, 18/3, 44, 0.4 • ABGs ordered • Once FiO2 60%, may start feeding with 5cc EBM q3/OGT with SAP • • • • • Start feeding 5cc EBM as ordered, if tolerated 3x, start increments: increase 5cc every feeding until 30cc MV setting: 60% 18/5 26 0.4 Wean FiO2 by 5 q2 til 21% Wean RR by 2 q2 til 10 Extract ABGs at RR=10 ABG 05/09/09 44 0.4 09:32 WEANING 80% pH 7.360 pCO2 32.70 pO2 149.00 HCO3 18.40 BEb -5.1 O2sat 99.20% 18/3 • Prepare for extubation • Prepare O2 hood FiO2 30% • MV settings at 21%, 18/3, 14, 0.4 • Revise inotropes: Dopamine 0.5cc + D5W 23.5 cc to run at 1cc/hour then consume then discontinue • S/P Extubation • Placed on O2 hood FiO2 30% • Racemic epinephrine nebulization started to continue 2 more doses 15 minutes apart • Patient noted to be jaundiced up to thighs • For TB DB IB • Increase feeding to 35cc q3/OGT • • • • • • For CPT with proper shields Dopamine discontinued NCPAP 30% PEEP 5 ABGs Noted vomiting with feeding; abdomen soft but distended Feeding decreased to 30cc ABG 05/11/09 04:13 S/P EXTUBATION 30% pH 7.324 N pCO2 38.60 N pO2 84.00 HCO3 20.30 BEb -4.7 O2sat 95.60% Maintain now N • • • • Increased feeding to 35cc TB DB IB noted Maintained on phototherapy PWI: FT 37 wks by PA, 2600 g, AGA, cephalic, delivered via primary LSCS, LBG, AS 5,9; Neonatal pneumonia; Hyperbilirubinemia no set-up Test 05/11/09 05/12/0 Units 9 TB 16.1 14.6 umol/L DB IB 0 16.1 0.0 14.6 Normal Values 17.00 – 180.00 umol/L 0.00 – 10.00 umol/L 10.00 – 180.00 • 13cc of feeding residual noted; no abdominal distention • Feeding deferred • Wean FiO2 by 5 q2 until 21% • Coffee-ground noted • NPO • Start Famotidine 1mg IV q12 • Give Vit K 2mg slow IV push • ABGs ordered at 25% PEEP 5 ABG 05/11/09 17:00 25% 18/3 pH pCO2 60 0.4 7.329 40.80 pO2 68 HCO3 21.80 BEb -3.5 O2sat 92.40 Atelectasis, Right Upper Lobe Atelectasis/Consolidation, Medial Segment of R Lower Lobe • PWI: FT, 37 wks by PA, 2600g, AGA, cephalic, rpt LSCS, LBG, AS 5,9; neonatal pneumonia; hyperbilirubinemia with no set-up; rule out nosocomial sepsis • Still with jaundice and coffee ground material • • • • • For repeat CBC with PC, blood CS, eletrolytes To start Ceftazidime (50mkd) 130mg IV q12h NPO IVF revised to: D10IMB Ca 400 @ 13cc/hr Please put patient on right side up Complete Blood Count Compone nt 05/07/09 05/12/09 Reference Range Unit WBC 5.56 24.42 5.0 – 30.0 X109/L RBC 3.74 3.66 4.0 – 6.0 X1012/L HGB 129 122 120-180 g/L HCT 0.386 0.358 0.370 – 0.540 MCV 103.2 97.8 80.0 – 100.0 Fl MCH 34.5 33.3 27.0 – 31.0 Pg MCHC 334 341 320 – 360 g/L RDW 17.2 17.3 11.0 – 16.0 % Platelet 227 142 150 – 450 X109/L NRBC 2/100 1 Complete Blood Count Component 05/07/09 05/12/09 Reference Range Unit Neutrophil 0.697 0.77 0.500 – 0.700 % Lymphocyt e 0.182 .07 0.200 – 0.500 % Monocyte 0.101 0.10 0.020 – 0.090 % Eosinophil 0.016 0.006 0.000 – 0.060 % Basophils 0.004 0.000 – 0.020 % Stab Metamyelo cyte Myelocyte Promyelocy te Blast Atypical % Meconium-stained amniotic fluid may be aspirated during labor and delivery, causing neonatal respiratory distress. Because meconium is rarely found in the amniotic fluid prior to 34 weeks' gestation, meconium aspiration chiefly affects infants at term and postterm. 3 major constituents of meconium: 1. Intestinal secretions 2. mucosal cells 3. solid elements of swallowed amniotic fluid are the 3 major solid constituents of meconium. Water - major liquid constituent, (8595%) Factors that promote meconium passage in utero include: • placental insufficiency, • maternal hypertension, • preeclampsia, • oligohydramnios, and • maternal drug abuse, especially of tobacco and cocaine. In utero meconium passage results from neural stimulation of a mature GI tract and usually results from fetal hypoxic stress. As the fetus approaches term, the GI tract matures, and vagal stimulation from head or cord compression may cause peristalsis and relaxation of the rectal sphincter leading to meconium passage. Meconium directly alters the amniotic fluid, reducing antibacterial activity and subsequently increasing the risk of perinatal bacterial infection. Meconium is irritating to fetal skin, thus increasing the incidence of erythema toxicum. However, the most severe complication of meconium passage in utero is aspiration of stained amniotic fluid before, during, and after birth. Aspiration induces hypoxia via 4 major pulmonary effects: 1. airway obstruction 2. surfactant dysfunction 3. chemical pneumonitis 1. Airway obstruction Complete obstruction - atelectasis. Partial obstruction - ball-valve effect. Hyperdistention of the alveoli occurs from airway expansion during inhalation and airway collapse around inspissated meconium in the airway, causing increased resistance during exhalation. 2. Surfactant dysfunction free fatty acids of the meconium (eg, palmitic, stearic, oleic), have a higher minimal surface tension than surfactant Meconium strip it from the alveolar surface, resulting in diffuse atelectasis. 3. Chemical pneumonitis Enzymes, bile salts, and fats in meconium irritate the airways and parenchyma, causing a release of cytokines results in a diffuse pneumonia that may begin within a few hours of aspiration. Presence of meconium in amniotic fluid is required to cause meconium aspiration syndrome (MAS), but not all neonates with meconium-stained fluid develop meconium aspiration syndrome. The presence of thick particulate meconium in the amnionic fluid increases the likelihood of prenatal aspiration. Green urine may be observed in newborns with meconium aspiration syndrome less than 24 hours after birth. Meconium pigments can be absorbed by the lung and can be excreted in urine. •Cyanosis •End-expiratory grunting •Alar flaring •Intercostal retractions •Tachypnea •Barrel chest in the presence of air trapping •Auscultated rales and rhonchi (in some cases) •Yellow-green staining of fingernails, umbilical cord, and skin may be observed. – Placental insufficiency – Maternal hypertension – Preeclampsia – Oligohydramnios – Maternal drug abuse, especially of tobacco and cocaine – Maternal infection/chorioamnionitis – Fetal gasping secondary to hypoxia – Inadequate removal of meconium from the airway prior to the first breath – Use of positive pressure ventilation (PPV) prior to clearing the airway of meconium Acid-base status • Metabolic acidosis from perinatal stress is complicated by respiratory acidosis from parenchymal disease and persistent pulmonary hypertension of the newborn (PPHN). • ABG measurement of pH, partial pressure of carbon dioxide (pCO2), partial pressure of oxygen (pO2), and continuous measurement of oxygenation by pulse oximetry are necessary for appropriate management. Serum electrolytes: Obtain sodium, potassium, and calcium concentrations when the infant with MAS aged 24 hours because the syndrome of inappropriate secretion of antidiuretic hormone (SIADH) and acute renal failure are frequent complications of perinatal stress. CBC count • In utero or perinatal blood loss, as well as infection, contributes to postnatal stress. • Hemoglobin and hematocrit levels must be sufficient to ensure adequate oxygen-carrying capacity. • Neutropenia or neutrophilia with left shift of the differential may indicate perinatal bacterial infection. gross overaeration of the lungs and bilateral nodular infiltrates The nodular infiltrates represent areas of patchy or focal alveolar atelectasis and the overaerated spaces in between, compensatroy, focal alveolar overdistension When aspiration occurs, intubation and immediate suctioning (tracheal suctioning) of the airway can remove much of the aspirated meconium No clinical trials justify suctioning based on the consistency of meconium. Do not perform the following harmful techniques in an attempt to prevent aspiration of meconium-stained amniotic fluid: • Squeezing the chest of the baby • Inserting a finger into the mouth of the baby The American Academy of Pediatrics Neonatal Resuscitation Program Steering Committee If the baby is not vigorous (defined as minimal or absent respiratory effort, poor muscle tone, or heart rate <100 beats/min): Use direct laryngoscopy, intubate, and suction the trachea immediately after delivery. Suction for no longer than 5 seconds. If no meconium is retrieved, do not repeat intubation and suction. If meconium is retrieved and no bradycardia is present, reintubate and suction. If the heart rate is low, administer positive pressure ventilation and consider suctioning again later. If the baby is vigorous (defined as good respiratory effort, crying, good muscle tone, and heart rate >100 beats/min): Do not electively intubate. Clear secretions and meconium from the mouth and nose with a bulb syringe or a large-bore suction catheter. In either case: The remainder of the initial resuscitation steps should ensue and include drying, stimulating, repositioning, and administering oxygen as necessary. • Maintain an optimal thermal environment • Minimal handling • Sedation - to decrease agitation • Continue respiratory care. Oxygen therapy via hood or positive pressure is crucial in maintaining adequate arterial oxygenation. If mechanical ventilation is required, make concerted efforts to minimize the mean airway pressure and to use as short an inspiratory time as possible. Oxygen saturations should be maintained at 90-95%. • Surfactant therapy • For treatment of persistent pulmonary hypertension of the newborn (PPHN), inhaled nitric oxide is the pulmonary vasodilator of choice • Pay careful attention to systemic blood volume and blood pressure. Volume expansion, transfusion therapy, and systemic vasopressors are critical in maintaining systemic blood pressure greater than pulmonary blood pressure, thereby decreasing the right-to-left shunt through the patent ductus arteriosus. 1. 2. chronic lung disease infections Most with complete recovery of pulmonary function Intrapartum events initiating the meconium passage may cause the infant to have longterm neurologic deficits: CNS damage, seizures, mental retardation, and cerebral palsy. Yellow color usually results from accumulation of unconjugated, nonpolar, lipid-soluble bilirubin pigment in the skin May be due in part to deposition of pigment from conjugated bilirubin Elevated levels of indirect, unconjugated bilirubin potentially neurotoxic Unconjugated hyperbilirubinemia factors: Increase load of bilirubin to be metabolized by liver Hemolytic anemia, polycythemia, shortened red cell life, increased enterohepatic circulation, infection Damaged or reduced the activity of the transferase enzyme or other related enzymes Genetic deficiency, hypoxia, infection, thyroid deficiency Blocked transferase enzyme Absence or decreased amounts of enzyme or reduced bilirubin uptake by liver cells Genetic defect, prematurity Jaundice appearing after the 3rd day and within the 1st week suggests bacterial sepsis or urinary tract infection Other causes: syphilis, toxoplasmosis, CMV, enterovirus Regardless of the cause, goal of therapy is to prevent indirect-reacting bilirubin related neurotoxicity Tx: phototherapy and exchange therapy THANK YOU!